[box type=”bio”] What to Learn from this Article?[/box]
1. Spinal Subdural hematoma should be a differential in cases presenting with rapidly progressive radiculopathy.
2. A detailed knowledge of the MRI appearance as per the chronological stages helps in diagnosis and management planning.
Case Report | Volume 5 | Issue 2 | JOCR April-June 2015 | Page 72-74| Kothari Manish K, Shah Kunal Chandrakant, Nene Abhay M. DOI: 10.13107/jocr.2250-0685.280
Authors: Kothari Manish K[1], Shah Kunal Chandrakant[1], Nene Abhay M[1]
[1] Department of Orthopaedics, Wockhardt Hospital, South Mumbai, India.
Address of Correspondence
Dr Kothari Manish Kundanmal
Associate, Spine Surgeon, Wockhardt Hospital, South Mumbai, India.
Email:- manishkkothari@gmail.com
Abstract
Introduction: Spinal Subdural hematoma is a rare cause of radiculopathy and spinal cord compression syndromes. It’s early diagnosis is essential. Chronological appearance of these bleeds vary on MRI.
Case Report: A 56 year old man presented with progressive left lower limb radiculopathy and paraesthesias with claudication of three days duration. MRI revealed a subdural space occupying lesion compressing the cauda equina at L5-S1 level producing a ‘Y’ shaped dural sac (Y sign), which was hyperintense on T1W imaging and hypointense to cord on T2W image. The STIR sequence showed hyperintensity to cord. There was no history of bleeding diathesis. The patient underwent decompressive durotomy and biopsy which confirmed the diagnosis.
Conclusion: Spinal subdural hematoma may present with rapidly progressive neurological symptoms. MRI is the investigation of choice. The knowledge of MRI appearance with respect to the chronological stage of the bleed is essential to avoid diagnostic and hence surgical dilemma
Keywords: Spinal subdural haematoma, extramedullary spinal cord compression, MRI scan.
Introduction
Spinal subdural haematomas are extremely rare occurrences. They are known to cause cord compression and radicular pain [1]. MRI has made it possible to chronologically label these haematomas as hyperacute, acute, subacute and chronic. We report a case with early subacute spinal subdural haematoma managed surgically.
Case report
A 56 year old gentleman presented to emergency with progressive history of pain along the left posterior aspect of thigh and postero lateral aspect of leg, going up to the lateral aspect of foot since three days. It was associated with paraesthesias in the same areas but no numbness. The paraesthesias were progressive. He did not have any back pain or contralateral leg pain. His pain worsened after walking for a couple of minutes and was relieved after taking rest. The general examination was unremarkable. On local examination there was no spasm or tenderness at the lumbar spine. There was mild restriction of forward bending. The straight leg raising test was positive on the left side at 40 degrees. There was no sensori-motor loss. The left ankle jerk was absent. The standing AP and lateral radiographs did not reveal any abnormality. MRI was done, which revealed a subdural space occupying lesion compressing the cauda equina at L5-S1 level producing the “Y” shaped dural sac on axial images (Fig 1). The lesion was hyperintense on T1W imaging (Fig 2) and hypointense to cord on T2W image (Fig 3). The STIR sequence showed hyperintensity to cord (Fig 4). 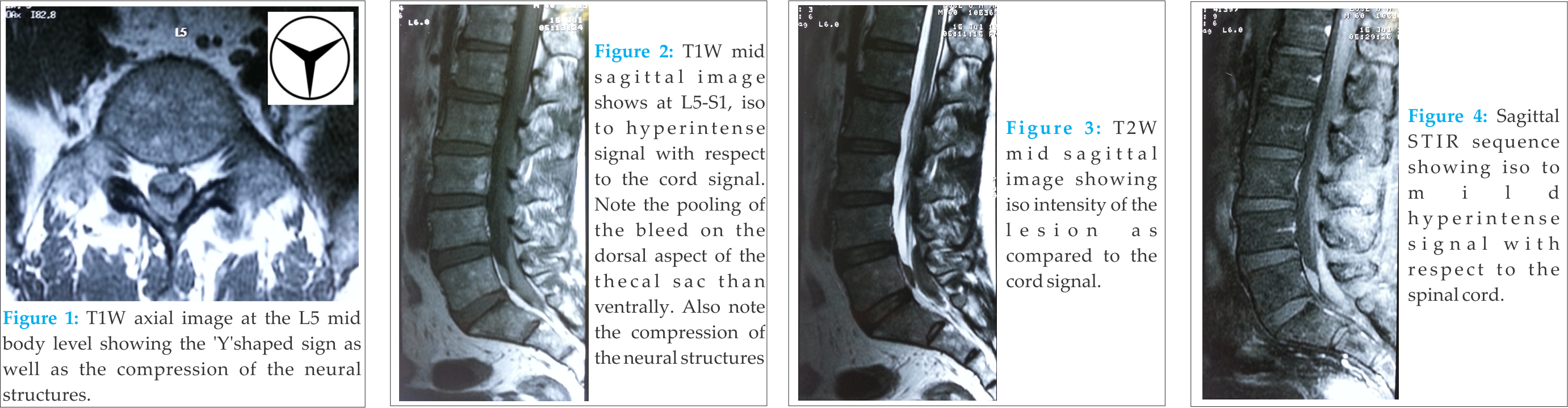 The radiological differentials included spinal subdural hematoma and lymphoma. The patient did not give any history of spinal intervention or bleeding diathesis or medications. There were no signs or symptoms related to higher functions. The patient underwent decompressive durotomy and frozen section biopsy which confirmed the diagnosis of a hematoma. Post operatively patient improved.
The radiological differentials included spinal subdural hematoma and lymphoma. The patient did not give any history of spinal intervention or bleeding diathesis or medications. There were no signs or symptoms related to higher functions. The patient underwent decompressive durotomy and frozen section biopsy which confirmed the diagnosis of a hematoma. Post operatively patient improved.
Discussion
Spontaneous non traumatic spinal subdural hematomas (SSH) are rare and literature is sparse. In contrast to their cranial counterparts which have bridging veins as a source of bleed, the pathogenesis and aetiology of SSH are not fully known. Various theories have been studied like migration from the intracranial space, [1] redistribution of clival subdural hematoma to dependant areas in lower lumbar spine [2] and collection of blood in the “intradural” space. [3]. These have been reported to occur after vigorous back massage [4] and even paraspinal muscle needling [5]. Symptoms include back pain and/or radiculopathy with variable amount of neurological deficit ranging from an acute rapidly progressive paraparesis to slowly developing mild deficit depending on the severity of neural compression. About half of these patients develop complete sensorimotor deficit. [6] Symptoms also vary according to the level of the bleed. The extent of bleed can vary from one to seven segments [6] MRI is the investigation of choice for diagnosis as well as for planning surgery. The differential diagnosis of an intradural mass includes haematoma, lipomatosis, abscess and tumours. In our case the MRI findings were suggestive of a haematoma versus lymphoma. The MRI findings in a spinal bleed vary according to the stage of bleed. [7] The hyperacute bleed is iso/hypointense on T1W sequence and hyperintense on T2W sequence. The acute hematoma is slightly hypo-/isointense on T1Wimages and hypointense on T2W images. In early subacute hematoma the T1W image is hyperintense and hypointense on T2W images. The late subacute hematoma is hyperintense on T1- and T2- weighted images. The chronic hematoma is usually hypointense on T1W and T2W images. Our patient had an early subacute haematoma as it was hyper on T1W and hypo on T2W images. The “Y” shaped sign we noted, is similar to the “Inverted Mercedes Benz” sign described by Kasliwal et al. [8]. This sign is a result of the encasement of blood around arachnoid lined neural structure. This helps to differentiate between an epidural and subdural location of the haematoma. Similarly, in the sagittal sections, the bleed takes the contour of the compressed arachniod membrane resembling two convex discs in apposition to each other, suggestive of liquid nature of the lesion. Location of the lesion in the dependant area (L5-S1) adds to this information. In contrast, intradural lymphomas usually take a fusiform or sausage shape, although any shape is possible.
There are no definite guidelines for management. Treatment involves conservative management with serial MRI in cases with preserved neurology [9], [10]. In cases with serious neurological deficit, laminectomy and drainage is required. Predictors of good outcome include pre operative neurological deficit and level of the lesion. The extent of the hematoma does not influence the surgical outcome. [6] Thus, one needs to be aware of the different stages of bleed and its MRI appearance for diagnosis. Early diagnosis using MRI imaging and prompt management is the key to prevent disastrous neurological consequences.
Conclusion
Spinal subdural hematoma may present with rapidly progressive neurological symptoms. MRI is the investigation of choice. The knowledge of MRI appearance with respect to the chronological stage of the bleed is essential to avoid diagnostic and hence surgical dilemma. Early symptoms without significant neurological deficits may be considered for conservative management.
Clinical
1. Spinal Subdural hematoma should be a differential in cases presenting with rapidly progressive radiculopathy.
2. MRI is the investigation of choice.
3. A detailed knowledge of the MRI appearance as per the chronological stages helps in diagnosis and management planning.
References
1. Bortolotti C, Wang H, Fraser K, Lanzino G. Subacute spinal subdural hematoma after spontaneous resolution of cranial subdural hematoma: causal relationship or coincidence? Case report. J Neurosurg 2004;100(4, Suppl Spine):372-4.
2. Ahn ES, Smith ER. Acute clival and spinal subdural hematoma with spontaneous resolution: clinical and radiographic correlation in support of a proposed pathophysiological mechanism. Case report. J Neurosurg 2005; 103(2, Suppl):175-9.
3. Schwartz FT, Sarrawi MA, Fox JL: Unusual hematomas outside the spinal cord. Report of two cases. J Neurosurg 1973; 39:249–5
4. Maste P, Paik SH, Oh JK, Kim YC, Park MS, Kim TH, Kwak YH, Jung JK, Lee HW, Kim SW. Acute spinal subdural hematoma after vigorous back massage: a case report and review of literature. Spine (Phila Pa 1976). 2014 Dec 1;39(25):E1545-8.
5. Ji GY, Oh CH, Choi WS, Lee JB. Three cases of hemiplegia after cervical paraspinal muscle needling. Spine J. 2015 Mar 1;15(3):e9-e13.
6. Thiex R, Thron A, Gilsbach JM, Rohde V. Functional outcome after surgical treatment of spontaneous and nonspontaneous spinal subdural hematomas. J Neurosurg Spine 2005; 3(1):12-16.
7. Braun P, Kazmi K, Nogués-Meléndez P, Mas-Estellés F, Aparici-Robles F. MRI findings in spinal subdural and epidural hematomas. Eur J Radiol 2007; 64(1):119-25.
8. Kasliwal MK, Shannon LR, O’Toole JE, Byrne RW. Inverted Mercedes Benz sign in lumbar spinal subdural hematoma. J Emerg Med. 2014 Dec;47(6):692-3.
9. Kulkarni AV, Willinsky RA, Gray T, Cusimano MD. Serial magnetic resonance imaging findings for a spontaneously resolving spinal subdural hematoma: case report. Neurosurgery 1998; 42(2):398-400
10. Yong Jin Park, Seok Won Kim, Chang IL Ju, Hui Sun Wang. Spontaneous resolution of non-traumatic cervical spinal subdural hematoma presenting acute hemiparesis: A Case Report. Korean J Spine 2012: 9(3):257-260.
| How to Cite This Article: Kothari Manish K, Shah Kunal Chandrakant, Nene Abhay M. Spinal Subdural Haematoma . Journal of Orthopaedic Case Reports 2015 April-June;5(2): 72-74. Available from: https://www.jocr.co.in/wp/2015/04/20/2250-0685-280-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com





