[box type=”bio”] What to Learn from this Article?[/box]
Ganglion cyst must be considered in the differential diagnosis of a swelling around knee joint line although it is rare; and though arthroscopic resection is the gold standard treatment of ganglion cyst of knee, we may need an open excision occasionally.
Case Report | Volume 5 | Issue 3 | JOCR July-Sep 2015 | Page 69-71 | Partha Saha, Utpal Bandyopadhyay, Anindya S. Mukhopadhyay, Srikanta Kundu, Subhadip Mandal. DOI: 10.13107/jocr.2250-0685.313.
Authors: Partha Saha[1], Utpal Bandyopadhyay[1], Anindya S Mukhopadhyay[1], Srikanta Kundu[1], Subhadip Mandal[1].
[1] Department of Orthopaedics, Nil Ratan Sircar Medical College & Hospital,
Kolkata, West Bengal, India.
Address of Correspondence
Dr. Partha Saha
Department of Orthopaedics, N.R.S. Medical College & Hospital, 138 A.J.C. Bose Road, Kolkata – 700014, West Bengal, India.
E mail – partha.orthoatnrs@gmail.com
Abstract
Introduction: Intra-articular ganglion cysts of the knee joint are rare occurrences. They are usually encountered as incidental findings in magnetic resonance imaging (MRI), or in arthroscopy. They may originate from both the cruciate ligaments and the menisci, from the popliteus tendon and alar folds, infrapatellar fat pad of Hoffa, and subchondral bone cysts. Those arising from the Hoffa’s fat pad, usually present as palpable mass at anterior aspect of the knee joint. We report a case of intra-articular ganglion cyst of knee arising from the infrapatellar fat pad and protruding anterolaterally through retinacular rent into the subcutaneous plane.
Case Report: A 19-year-old young man, presented with a painless gradually increasing swelling at the anterior aspect of left knee of 9 months duration. MRI scan revealed a multilobulated, cyst with septations within the anterior aspect of the knee joint, just inferolateral to the patella, with deep extension into the infrapatellar fat pad, and superficial extension into the subcutaneous space across the retinaculum. After diagnostic arthroscopy, we performed an open excision of the cystic mass and confirmed the retinacular rent pre-operatively.
Conclusion: Arthroscopic resection and debridement is the gold standard treatment in ganglion cyst of the knee. However, a subcutaneous extension may lead to incomplete arthroscopic resection: Leaving behind the residual tissue which may cause recurrence. Therefore, proper pre-operative evaluation of MR images of these cases is very important.
Keywords: Intra-articular ganglion, subcutaneous ganglion cyst of knee, Ganglion cyst of knee joint.
Introduction
A ganglion is a cystic tumor-like lesion of unknown etiology, surrounded by a dense network of connective tissue, filled with a gelatinous fluid containing hyaluronic acid and other mucopolysaccharides [1]. They most commonly occur around dorsum of the wrist. Intra-articular ganglion cysts of the knee joint are uncommon. They are usually encountered as incidental findings in magnetic resonance imaging (MRI), or in arthroscopic examination [2]. They may originate from both the cruciate ligaments and the menisci, from the popliteus tendon and alar folds, infrapatellar fat pad of Hoffa, and subchondral bone cysts [2]. Those arising from the Hoffa’s fat pad have been reported to present as palpable mass at anterior aspect of knee joint [2-5]; however, to the best of our knowledge, none of them had subcutaneous communications across the retinaculum. We report a case of intra-articular ganglion cyst of knee arising from the infrapatellar fat pad and protruding anterolaterally through retinacular rent into the subcutaneous plane.
Case Report
A.A.M., a 19-year-old young man, presented with a painless gradually increasing swelling at the anterior aspect of left knee for last 9 months. There was no history of trauma, local injections, instability, locking episodes, clicking, snapping, or any constitutional symptoms. Clinical examination revealed a 2.5 cm × 2.5 cm round, soft, cystic, non-tender, irreducible swelling at anterolateral aspect of left knee 1.5 cm above the lateral joint line just lateral to the patellar tendon with discoloration of the overlying skin. It was partially mobile, not fixed to the extensor mechanism or overlying skin, and was more prominent in knee extension (Fig. 1). He could squat and sit cross-legged without any discomfort with a normal range of movement. There was no effusion, no joint line tenderness, and no evidence of ligamentous laxity. McMurray’s test was negative. Blood investigations were within normal limits. Plain radiographs were also normal apart from the increased soft tissue shadow (Fig. 2). MRI scan revealed a multilobulated, cyst with septations within the anterior aspect of the knee joint, just inferolateral to the patella, with deep extension into the infrapatellar fat pad. Superficially, it was extending into the subcutaneous space across the retinaculum (Fig. 2). It was hypointense on T1-weighted images and hyperintense on T2-weighted images. We performed diagnostic arthroscopy which revealed no other obvious intra-articular pathology. The cyst was not clearly visible through arthroscopy. Then we went for open excision of the cystic mass through lateral parapatellar approach (incision included that of the anterolateral arthroscopic portal). The cyst was found to be protruding just beneath the skin through a retinacular rent (Fig. 3). The rent was surgically extended above and below. The cyst origin from the fat pad was confirmed. The cyst got ruptured toward the end of the procedure. However, the entire mass was taken out, but we had to sacrifice the fat pad almost entirely. Histopathological examination was carried out, and it was compatible with a ganglion cyst. Post-operatively the patient underwent appropriate rehabilitation making an uneventful recovery and returned to his normal activities. He was symptom-free in his last follow-up at 6 months post-operatively. However, the discoloration of the overlying skin did not improve.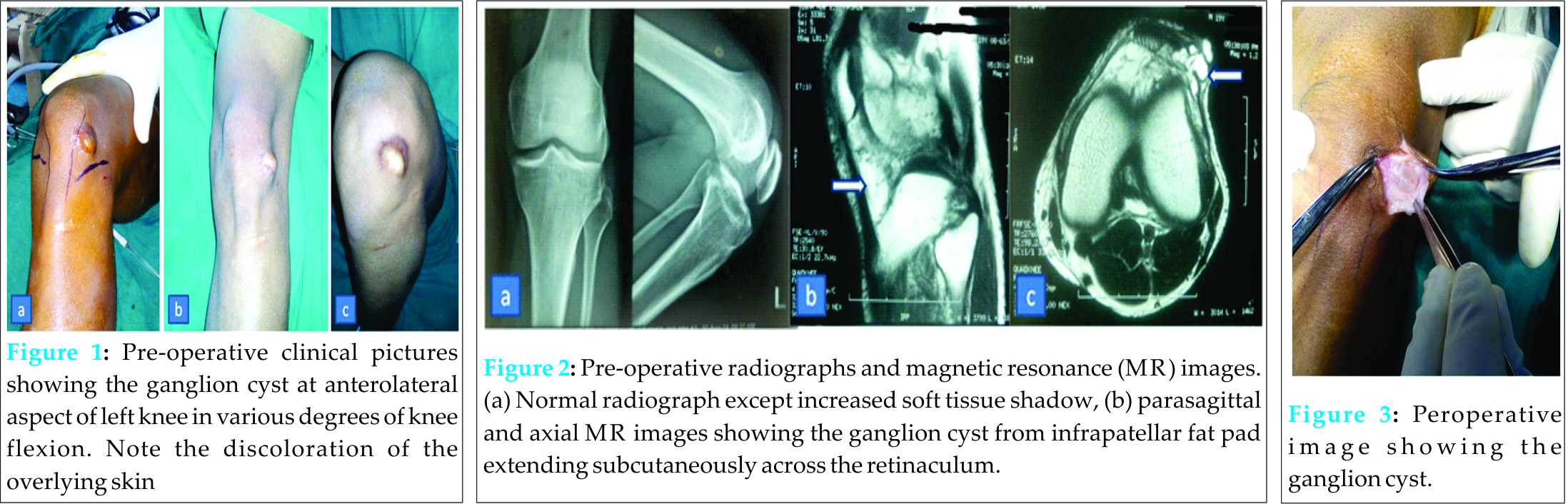
Discussion
Between the first description of an anterior cruciate ligament (ACL) ganglion by Caan in 1924 during a routine autopsy and the early 1990s, only a handful of sporadic cases were described in the literature. The last 30 years have seen a huge increase in the number of these cases being reported owing to the widespread use of both MRI and arthroscopy. The prevalence of intra-articular cystic knee masses is 1.3% in MRI and 0.6% in arthroscopy [1,6]. The pathogenesis and etiology of ganglion cyst formation remains unclear. Several theories have been suggested: (a) Synovial tissue herniation, (b) mucinous degeneration of connective tissue after trauma, (c) synovial ectopia or displacement during embryogenesis, etc. [7]. The histological finding that ganglia are fluid-filled structures without any epithelial lining confirms that they are not true cysts, and thus favors the degenerative theory over others [8]; and, even though, ganglia may develop in the absence of trauma, it is postulated that repetitive microtrauma from joint and soft tissue motion may play an important role [4]. Intra-articular ganglia of knee originates most commonly from the ACL accounting for more than 50% cases; whereas, the location at infrapatellar fat pad is far less common (approximately 4%) [2]. However, only 10% of them are symptomatic with most being incidental finding on MRI or arthroscopy [2]. The symptoms are usually non-specific, like knee pain, locking, clicking or popping sensation, decreased range of motion, etc., and depend on the site and size of the cyst. Ganglia anterior to the ACL tend to limit extension, whereas those posterior to the posterior cruciate ligament often limit knee flexion [1,9,10].
MRI is the investigation of choice because it is the most sensitive, specific accurate, and noninvasive method for depicting such cystic masses, including their size and location, and to detect associated intra-articular pathologies [2]. For intra-articular ganglion cyst in the infrapatellar fat pad, fat-suppressed contrast-enhanced MRI could be useful, because a thin, rim-enhancing feature of intra-articular ganglion cyst allows it to differentiate from synovial hemangioma and synovial sarcoma [3]. Among the various treatments available, arthroscopic resection and debridement are currently the preferred procedure; open surgery may be necessary in particular cases only [2,3,9]. After diagnostic arthroscopy, we performed an open excision of the ganglion cyst since it was not clearly visible on arthroscopy; moreover, we did not have any previous experience of arthroscopic resection of intra-articular ganglion cysts. Hence, in view of the high recurrence rate after incomplete removal of ganglion, we preferred open excision over arthroscopic resection.
Although recurrence is rare after arthroscopic or open surgical treatment of ganglion cyst of knee, the fact that it does occur in other areas even after excision [3], this patient should be followed up on regular basis.
Conclusion
Current literature suggests arthroscopic resection and debridement as the gold standard treatment of ganglion cyst of the knee. However, a subcutaneous extension may lead to incomplete arthroscopic resection: Leaving behind the residual tissue which may cause recurrence. Therefore, proper pre-operative evaluation of MR images of these cases is very important.
Clinical Message
Intra-articular ganglion cysts of the knee joint are rare occurrences. They are usually encountered as incidental findings in MRI, or in arthroscopy. Arthroscopic resection and debridement is regarded as the gold standard treatment in ganglion cyst of the knee. However, very rarely, these masses may extend subcutaneously across the retinaculum. This may lead to incomplete arthroscopic resection: Leaving behind the residual tissue which may cause recurrences. Therefore, proper pre-operative evaluation of MR images of these cases is very important.
Reference
1. Beaman FD, Peterson JJ. MR imaging of cysts, ganglia, and bursae about the knee. Radiol Clin North Am 2007;45(6):969-982, vi.
2. Krudwig WK, Schulte KK, Heinemann C. Intra-articular ganglion cysts of the knee joint: A report of 85 cases and review of the literature. Knee Surg Sports Traumatol Arthrosc 2004;12(2):123-129.
3. David KS, Korula RJ. Intra-articular ganglion cyst of the knee. Knee Surg Sports Traumatol Arthrosc 2004;12(4):335-337.
4. Bui-Mansfield LT, Youngberg RA. Intraarticular ganglia of the knee: Prevalence, presentation, etiology, and management. AJR Am J Roentgenol 1997;168(1):123-127.
5. Liu PC, Chen CH, Huang HT, Chang JK, Chen JC, Tien YC, et al. Snapping knee symptoms caused by an intra-articular ganglion cyst. Knee 2007;14(2):167-168.
6. Sloane J, Gulati V, Penna S, Pastides P, Baghla DP. Large intra-articular anterior cruciate ligament ganglion cyst, presenting with inability to flex the knee. Case Rep Med 2010;2010:705919.
7. Soren A. Pathogenesis and treatment of ganglion. Clin Orthop Relat Res 1966;48:173-179.
8. Bergin D, Morrison WB, Carrino JA, Nallamshetty SN, Bartolozzi AR. Anterior cruciate ligament ganglia and mucoid degeneration: Coexistence and clinical correlation. AJR Am J Roentgenol 2004;182(5):1283-1287.
9. Sarimo J, Rantanen J, Helttula I, Orava S. Intra-articular cysts and ganglia of the knee: A report of nine patients. Knee Surg Sports Traumatol Arthrosc 2005;13(1):44-47.
10. Seki K, Mine T, Tanaka H, Isida Y, Taguchi T. Locked knee caused by intraarticular ganglion. Knee Surg Sports Traumatol Arthrosc 2006;14(9):859-861.
| How to Cite This Article: Saha P, Bandyopadhyay U, Mukhopadhyay AS, Kundu S, Mandal S. Ganglion Cyst of Knee from Hoffa’s Fat Pad Protruding Anterolaterally Through Retinacular Rent: A Case Report. Journal of Orthopaedic Case Reports 2015 July – Sep;5(3):69-71 . Available from: https://www.jocr.co.in/wp/2015/07/10/2250-0685-313-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com





