[box type=”bio”] What to Learn from this Article?[/box]
Restoration of length, radial bow and rotation often becomes secondary to achieving union in patients with fractures through contracted forearms, and shortening osteotomies may be necessary to restore bony apposition.
Case Report | Volume 6 | Issue 5 | JOCR November-December 2016 | Page 55-58 | Mark Ayzenberg, Nathan C Tiedeken, Dillon E Arango, James Raphael. DOI: 10.13107/jocr.2250-0685.630
Authors: Mark Ayzenberg[1], Nathan C Tiedeken[1], Dillon E Arango[1], James Raphael[1]
[1]Department of Orthopaedics, Einstein Medical Center, Philadelphia, PA 19141, USA.
Address of Correspondence
Dr. Nathan C Tiedeken,
Einstein Medical Center, 5501 Old York Road, Willowcrest Building 4th Floor, Philadelphia, PA 19141, USA.
E‑mail: nathan.tiedeken@gmail.com
Abstract
Introduction: There is a paucity of information on management of forearm fractures through pre‑existing ischemic contractures. The prevention of a Volkmann’s contracture in forearm compartment syndrome requires vigilant clinical evaluation and emergent fasciotomy, but many of the patients who develop these contractures often do so as a result of delayed presentation due to substance abuse and intoxication. This case describes the first report and management of a severely displaced both bone (BB) forearm fracture through a chronic forearm Volkmann’s contracture.
Case Report: A 39 year old female presented with an acute both bone forearm fracture in the setting of a Volkmann’s contracture. Although very limited in use, the arm was functional for holding objects and was determined to be important in her activities of daily living. The surgical management involved open reduction internal fixation with radial and ulnar shortening osteotomies to restore cortical alignment secondary to the extensive overlying soft tissue contractures.
Conclusion: Restoration of the radial bow and other standard principles of open reduction and internal fixation of BB fractures may not be as important as obtaining fracture union in patients with these complicated injuries due to the pre‑existing functional limitations of the limb. The soft tissue envelope in a contracted forearm is commonly fibrotic and provides an abnormal fracture healing environment. Careful attention to osseous and soft tissue healing in the postoperative period is recommended. This report details the first case, technical difficulties, and subsequent management of a BB fracture in the setting of subsequent management of a both bone fracture in the setting of a chronic Volkmann’s contracture.
Keywords: Both bone fracture, Volkmann’s contracture, compartment syndrome.
Introduction
In 1881, Volkmann first described an ischemic forearm contracture that resulted as a consequence of an untreated forearm compartment syndrome [1, 2]. Increased pressure within the osseofascial compartments leads to decreased capillary perfusion, resulting in progressive ischemia and eventual muscle necrosis [3, 4]. The resulting myonecrosis causes muscle fibrosis and debilitating contractures. Seddon described a Volkmann contracture classification system that was later revised by Tsuge. Divided into three types, the mild type primarily affects the finger flexor muscles. The moderate type affects both the wrist and finger flexors, while the severe type involves extensor muscles in addition to both the wrist and finger flexors [5, 6].
Contracture prevention requires astute clinical evaluation and emergent operative intervention in the setting of compartment syndrome. Adult patients that develop this contracture often do so as a result of delayed presentation, such as in cases of intoxication or refusal of surgical intervention [7, 8]. Prolonged external pressure on the forearm during a drug‑induced haze was the most common cause for the development of forearm compartment syndrome and subsequent Volkmann’s contracture [6]. Owen et al. studied changes in forearm compartment pressures in volunteers placed in positions typical of patients found after drug overdose. This study demonstrated that pressures in limbs compressed between a hard surface and the body easily reached pressures that resulted in muscle ischemia [9]. In 2012, statistics showed a nationwide increase in illegal drug use in the United States, with approximately 9.2% of the population using illicit drugs within the last month [10]. As drug use continues to be prevalent in society, orthopedic surgeons must be aware of the management of potential sequelae of drug abuse, including Volkmann’s contracture.
Although both bone (BB) forearm fractures are common injuries in the pediatric population, adult BB fractures are less common [11]. While the mainstay of treatment for pediatric patients is nonoperative or with less invasive reduction techniques, the adult population frequently requires open reduction internal fixation (ORIF). ORIF with compression plating has resulted in high union rates for adult BB fractures [12]. Adherence to operative principles such as restoration of radial bow and compression plating has been shown to be critical in the adult functional outcome [12]. A BB fracture in a patient with a Volkmann’s contracture presents a formidable surgical undertaking. Restoration of length, sagittal, coronal, and rotational alignment of the radius and ulna can be technically challenging in the setting of a severely contracted forearm. The patients with a patients with a Volkmann’s contracture have a variable range of motion, and depending on preoperative function of the contracted forearm, re‑establishment of the radial bow or alignment may not be as crucial as obtaining a solid union. In addition to fracture care, soft tissue management is essential as the surrounding soft tissues are often compromised and may demonstrate scars from prior surgeries, skin contractures or skin grafts. The surgeon must take all of these variables into consideration, when formulating a plan of care for these complicated patients. Close attention to post‑operative wounds and osseous union is important as the decreased muscle viability overlying the fracture site can delay healing and tenuous soft tissues can be compromised. The management of an adult BB forearm fracture in the setting of a pre-existing Volkmann’s contracture has not been previously discussed. This report describes the management of a 39-year-old female with a chronic Volkmann’s contracture who presented with an acute BB forearm fracture after a motor vehicle accident.
Case Report
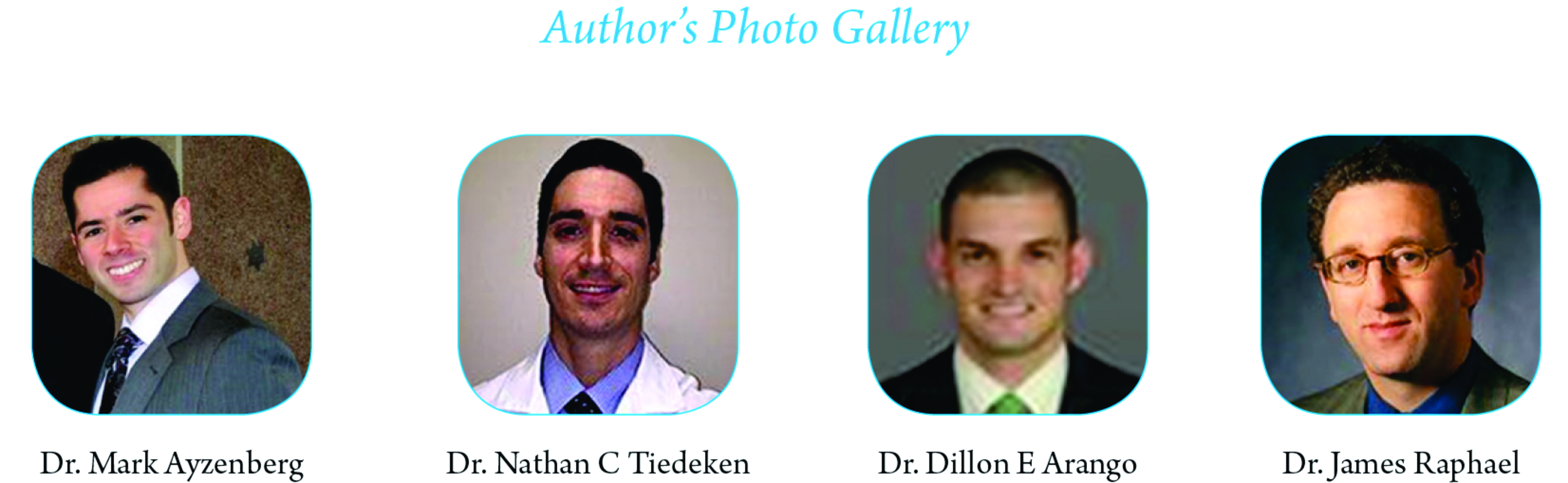
A 39‑year‑old female presented as an unrestrained driver involved in a high‑velocity motor vehicle accident. After initial stabilization, secondary survey demonstrated an acute, osseous deformity of the right forearm with a concomitant Volkmann’s contracture. Neurovascular examination was intact but limited secondary to the chronic contracture. The radiographic examination revealed a displaced and shortened BB forearm fracture (Fig. 1). Past medical history revealed longstanding substance abuse with a previous right forearm compartment syndrome. 6 years prior, she was found unconscious for an unknown duration on her right arm while in a drug‑induced haze. Despite emergent dorsal and volar fasciotomy, extensive myonecrosis was observed intraoperatively and she, subsequently, developed a Volkmann loped a Volkman. Clinical examination of the contracture demonstrated a static wrist flexion contracture of 90° with clawing deformities of the small and ring fingers lacking any functional pronation or supination. The thumb was held in a fixed flexion deformity, while the index and long fingers exhibited a 35° extension contracture at the metacarpal phalangeal joints with limited motion at the distal interphalangeal and proximal interphalangeal joints. Her elbow range of motion was limited to a 35° arc of motion (75‑110°). Despite these deformities, the patient reported her right upper extremity was integral in her activities of daily living. She has been able to drive an automatic transmission vehicle using her left upper extremity without difficulty despite her contracture on the right.
Operative intervention with ORIF and compression plating was performed. The ulna was exposed through the flexor carpi ulnaris and extensor carpi ulnaris interval. A dorsal approach between extensor carpi radialis brevis and extensor digitorum comminus was utilized as previous skin grafting and fasciotomy scarring precluded the use of a volar incision (Fig. 2). Despite a general anesthesia, paralytics and a supraclavicular block, intraoperative restoration of forearm length was impossible due to the forearm contracture. Ulnar and radial osteotomies of 2.1 cm were required to achieve reduction of the forearm with two 7‑hole limited contact dynamic compression plates (Fig. 2). The osteotomy of 2.1 cm was the minimal amount of bone resection possible that would allow us to realign the fracture. No soft tissue, release was performed given her longstanding contractures and to minimize compromise of soft tissues for fracture site healing. Post‑operative evaluation demonstrated no complications, well‑healed incisions, intact hardware, and a maintained forearm reduction (Fig. 3). At final follow‑up of 4 months, her range of motion of the elbow and wrist were unchanged from her preoperative examination (75‑110° elbow motion and a fixed 90° wrist flexion contracture), and she fully regained her preoperative functional ability.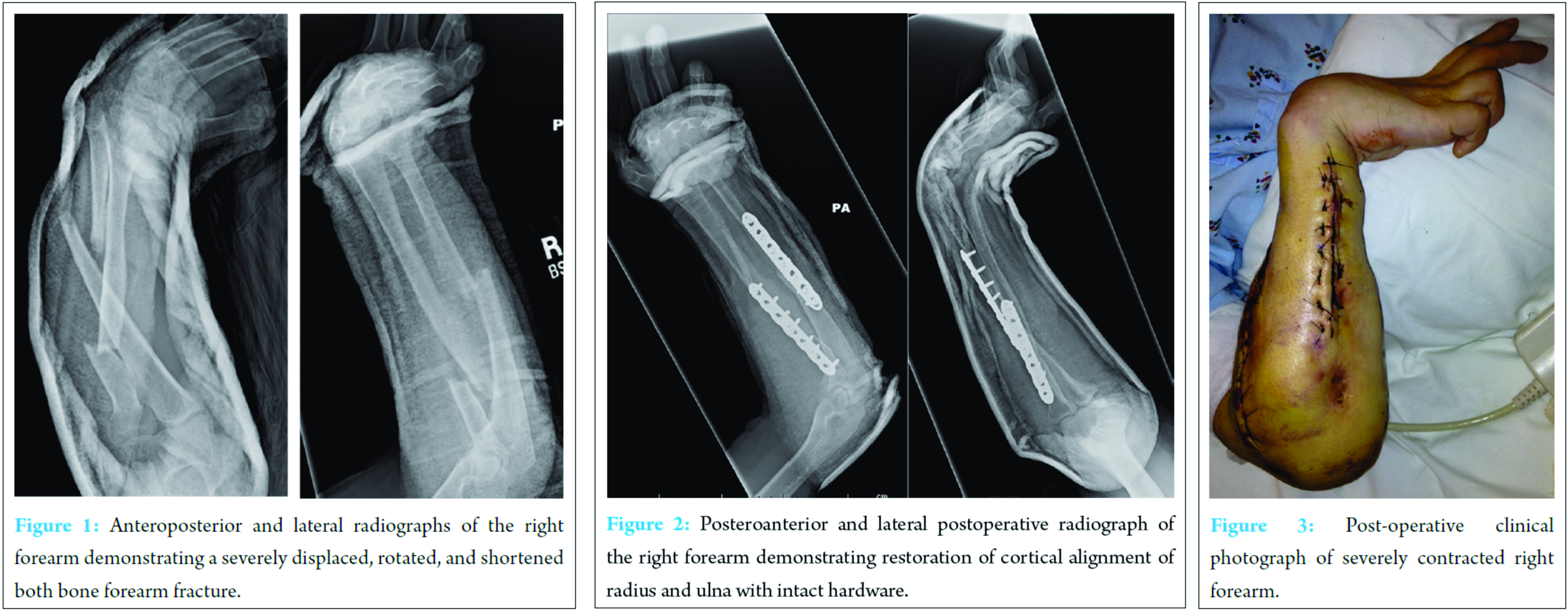
Discussion
Treating patients with fractures through a contracted extremity is a complicated process requiring careful preoperative planning. To obtain a successful outcome, the surgeon requires an understanding of not only the acute injury but also the details surrounding the chronic contracture. In the described case, previous medical documentation detailed the prior fasciotomy incisions and the status of the volar compartment. Applying this historical knowledge to the current injury, it was determined that a volar approach to the radius would be compounded by abnormal anatomy, fibrotic muscle, and potential wound coverage issues. A surgical approach minimizing exposure through contracted tissues is important for surgical anatomy and post‑operative wound healing. For these reasons, a dorsal approach to the radius afforded a safer and less complicated approach for fracture fixation in this patient.
While restoration of forearm length, radial bow, and rotation are the principles of BB fracture care in the noncontracted adult patient, a BB fracture in a Volkmann’s contracture may require less emphasis on these principles given each patient’s preoperative function. In a contracted forearm, fibrotic musculature maintains a set length due to the radius and ulna being intact. In the setting of a BB fracture, this fibrotic, inelastic muscle mass no longer maintains its length, and shortening of the fracture segments occurs. When traditional methods of restoring length and rotation fail due to the pre‑existing contracture, achieving union must become the most important goal. This may require radial and ulnar shortening osteotomies at the cost of restoring an anatomic radial bow. While the postoperative function of noncontracted patients with a BB fracture has been correlated with the restoration of the radial bow, this may not hold true in patients with a Volkmann’s contracture [12]. An understanding of preoperative function in the fractured, contracted extremity can help dictate intraoperative decision making when preinjury length cannot be obtained. The patient in this report had limited function of the contracted extremity but stated she routinely used her contracted forearm for tasks such as carrying groceries. Thus, it was determined that achieving a bony union with excellent cortical contact would continue to afford the same postoperative function once healed, despite the loss of anatomic radial bow.
While post‑operative vigilance is required for any patient with a surgically treated BB fracture, more frequent clinical and radiographic follow‑up is required in the setting of a BB fracture through a contracted forearm. Decreased vascularity at the fracture site and the soft tissues as a result of previous compartment syndrome and fasciotomy scarring can compromise fracture and wound healing. The dermis in Volkmann’s contracture may exhibit areas of skin grafts, contractures, and inelastic scar tissue. In normal fracture environments, forearm musculature is a rich source of blood supply to aid in fracture healing. This blood supply provides progenitor cells that differentiate into osteoclasts and osteoblasts to contribute to fracture healing [13, 14, 15]. In the setting of a Volkmann contracture, the surrounding musculature has become a fibrotic, avascular mass. These abnormal soft tissue conditions result in decreased cutaneous vascularity, which can compromise osseous and wound healing. Depending on the extent of muscle necrosis and vascular damage, the treating surgeon must remain vigilant for the development of a delayed or atrophic nonunion. Alteration of normal BB postoperative protocols may require prolonged immobilization, and weight bearing restrictions to reflect this delayed osseous healing.
Although the overall incidence of untreated adult forearm compartment syndrome is rare, drug‑induced unconsciousness and prolonged external pressure on the forearm has become a more common cause of Volkmann’s contracture in the adult population. As illicit substance abuse continues to rise, so does the risk of untreated forearm compartment syndrome. A general knowledge of operative care and potential pitfalls in the treatment of BB fractures in a contracted upper extremity must be understood.
Conclusion
This is the first report in the literature describing, the management of a BB fracture through a pre-existing Volkmann’s ischemic contracture. This patient demonstrated significant pain, fracture displacement, and acceptable pre-operative function, which precluded conservative management. ORIF was performed with an ulnar and dorsal forearm approach, which minimized exposure through previously operated volar contracted tissues. When managing a BB fracture in a Volkmann’s contracture, extensive radial and ulnar shortening osteotomies may be required to regain cortical contact, fracture compression, and an acceptable alignment. Frequent radiographic and clinical evaluation in the postoperative period is imperative for managing these complex upper extremity injuries.
Clinical Message
It is important to determine preoperative function in developing a surgical plan to treat patients with fractures through a contracted extremity. Restoration of length, radial bow and rotation often becomes secondary to achieving union in these patients, and shortening osteotomies may be necessary in order to restore bony apposition. Careful preoperative planning and consideration of the soft tissue envelope is critical in a successful approach.
References
1. Volkmann R. von. Die ischaemischen muskellahmungen und-kontrakturen. Zentrabl Chir. 1881; 8:801—803.
2. Hovius SE, Ultee J. Volkmann’s ischemic contracture. Prevention and treatment. Hand Clin. 2000; 16:647-657.
3. Kalyani BS, Fisher BE, Roberts CS, Giannoudis PV. Compartment syndrome of the forearm: A systematic review. J Hand Surg Am 2011;36:535-543.
4. Leversedge FJ, Moore TJ, Peterson BC, Seiler JG 3rd. Compartment syndrome of the upper extremity. J Hand Surg Am 2011;36:544-559.
5. Seddon HJ. Volkmann’s contracture: Treatment by excision of the infarct. J Bone Joint Surg Br 1956;38-B(1):152-174.
6. Tsuge K. Treatment of established Volkmann’s contracture. J Bone Joint Surg Am 1975;57(7):925-929.
7. Conner AN. Prolonged external pressure as a cause of eschaemic contracture. J Bone Joint Surg Br 1971;53(1):118-122.
8. Osborne AH, Dorey LR, Harvey JP Jr. Volkmann. J Bone Joint Surg Brt Surg Br cause of eschaemic contracture. J Bone Joint SurSurg 1972;104:794-798.
9. Owen CA, Mubarak SJ, Hargens AR, Rutherford L, Garetto LP, Akeson WH. Intramuscular pressures with limb compression clarification of the pathogenesis of the drug-induced muscle-compartment syndrome. N Engl J Med 1979;300(12):1169-1172.
10. Results from the 2012 National Survey on Drug Use and Health. National Institute on Drug Abuse. January, 2014. Available from: http://www.samhsa.gov/data/ NSDUH/2012SummNatFindDetTables/NationalFindings/ NSDUHresults2012.htm. [Last accessed on 2015 Jul].
11. Landin LA. Epidemiology of children’s fractures. J Pediatr Orthop B. 1997;6(2):79-83.
12. Schemitsch EH, Richards RR. The effect of malunion on functional outcome after plate fixation of fractures of both bones of the forearm in adults. J Bone Joint Surg Am 1992;74:1068-1078.
13. Henrotin Y. Muscle: A source of progenitor cells for bone fracture healing. BMC Med 2011;9:136.
14. Liu R, Schindeler A, Little DG. The potential role of muscle in bone repair. J Musculoskelet Neuronal Interact 2010;10:71-76.
15. Shah K, Majeed Z, Jonason J, O’Keefe RJ. The role of muscle in bone repair. the cells, signals, and tissue responses to injury. Curr Osteoporos Rep. 2013;11:130-135.
| How to Cite This Article: Ayzenberg M, Tiedeken NC, Arango DE, Raphael J. Acute Both Bone Fracture in a Chronic Contracted Forearm. Journal of Orthopaedic Case Reports 2016 Nov‑Dec;6(5):55‑58. Available from: https://www.jocr.co.in/wp/2016/11/10/2250-0685-630-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com