[box type=”bio”] What to Learn from this Article?[/box]
Lower limb intratendinous ganglion cysts are extremely uncommon and do not form a differential diagnosis on routine basis, thus every lower limb cyst should be subjected to ultrasonography or magnetic resonance imaging to know better about the pathology before going for an excision/surgical procedure.
Case Report | Volume 6 | Issue 5 | JOCR November-December 2016 | Page 85-88 | Puneet Maheshwari, Pramod Maheshwari, Pramod Bapna DOI: 10.13107/jocr.2250-0685.646
Authors: Puneet Maheshwari[1], Pramod Maheshwari[1], Pramod Bapna[2]
[1]Department of Orthopaedics, Maheshwari Nursing Home, 163, Bhagat Singh Marg, Dewas, Madhya Pradesh, India,
[2]Department of Radiologist, Bapna Advance Mediscan, Dewas, Madhya Pradesh, India.
Address of Correspondence
Dr. Puneet Maheshwari,
163, Bhagat Singh Marg, Maheshwari Nursing Home, Dewas – 455 001, Madhya Pradesh, India.
E-mail: Puneet 1984@gmail.com
Abstract
Introduction: Ganglion cysts are commonly seen in wrist joints and knee joint, but intra-tendinous ganglion cysts are extremely rare. We report the first case of intratendinous ganglion cyst of semi-tendinous tendon.
Case Report: A 4-year-old boy presented with painless soft tissue swelling over knee with no history of recent trauma. Radiograph was normal and USG showed a well-defined hypoechoic cystic lesion. Patient was taken for surgery and the lesion was removed. Lesion came out to be a ganglion cyst originating from the semitendinosus tendon. Post-operative USG was done to confirm complete removal of the ganglion.
Conclusion: Intra-articular ganglion cysts are common, and we find it regularly in our daily practice. However, we should be aware of the occurrence of intratendinous ganglion cysts also which on examination may look like a lipoma. Thus for all cysts around the tendons, an USG is must. Also repeat USG should be done to rule out incomplete excision and recurrence.
Keywords: Intra tendinous ganglion cyst, semitendinous tendon ganglion, ganglion, knee
Introduction
A ganglion cyst is common soft tissue tumour-like lesion, which is generated by mucous degeneration of joint capsule, tendon, or tendon sheath [1]. The cyst may be monoloculated or multiloculated. Popliteal fossa cysts communicate with the knee joint via a stalk are called as Baker’s cyst, whereas non-communicating cysts are ganglion cysts and juxta-articular myxomas [2]. It can occur in any part of the body including wrists, foot, and hand but an intratendinous cyst is a rare occurrence, especially around the knee joint. In intratendinous cyst, the cyst is present inside the tendon sheath and originates within the tendon [3, 4].
To our knowledge, this the first reported case of an intratendinous ganglion cyst of the semitendinosus tendon.
Case Report
A 4-year-old boy presented with soft tissue painless swelling, insidious in onset, gradually progressive over the side of the left knee joint. There was no history of any associated significant trauma or inflammation in recent past.
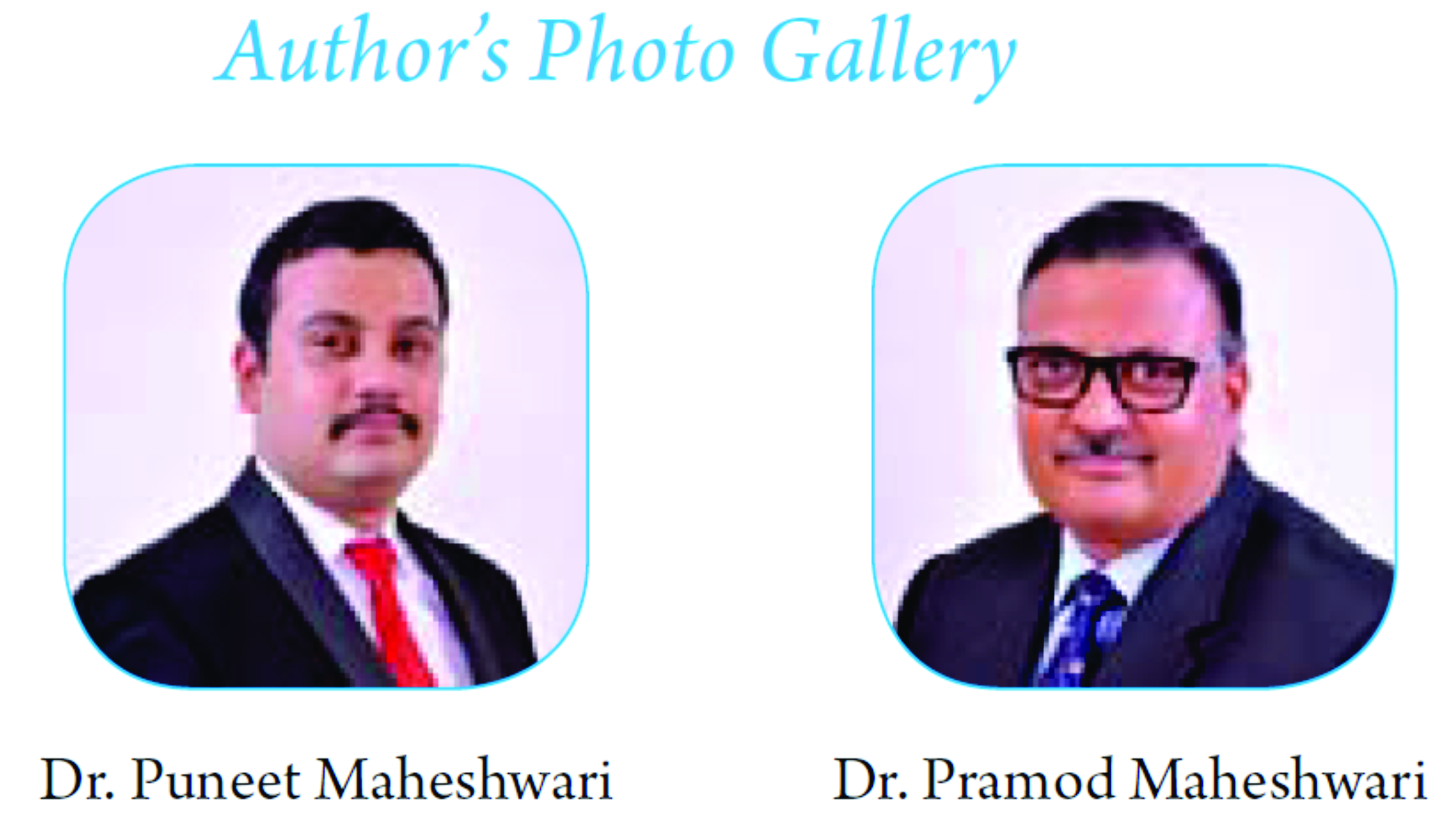
The physical examination revealed a palpable, well-defined 3 cm × 1.5 cm, subcutaneous swelling over the posteromedial aspect of the left knee joint. The swelling was non-tender and not moveable. It was not adherent to the overlying skin. There was no functional or neurological deficit associated (Fig. 1, 2).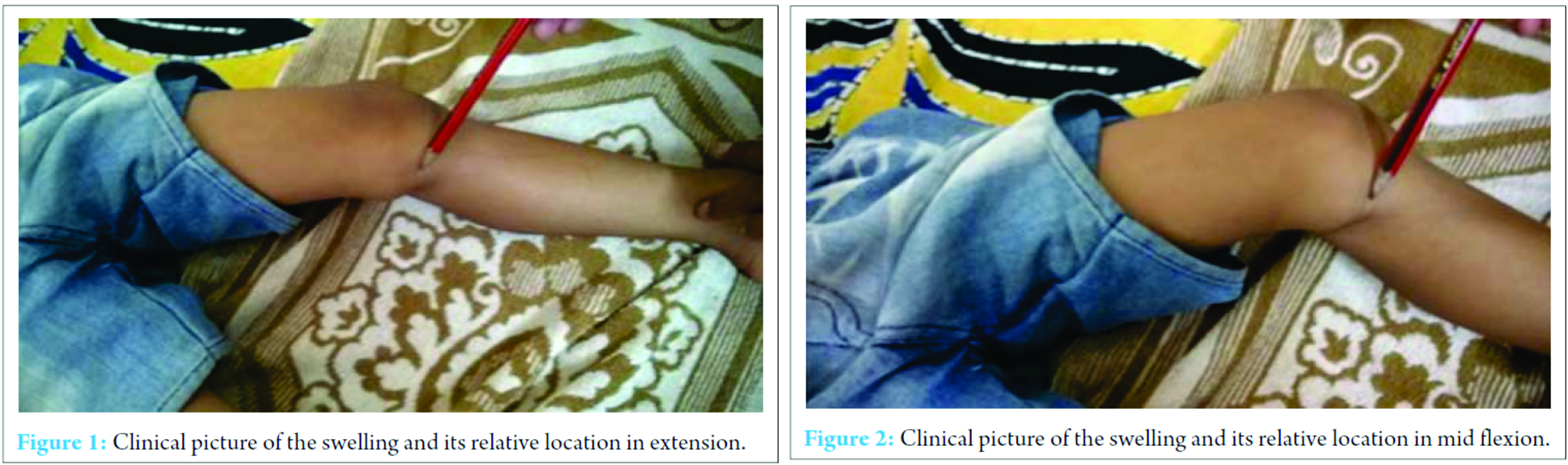
X-ray of the knee joint was unremarkable (Fig. 3, 4). Ultrasonography (USG) revealed a hypoechoic well-defined cystic lesion with clear contents is visualized on the antero-medial aspect of the left knee over the semitendinosus tendon. The lesion measures 25 mm × 10 mm. The lesion is causing splaying of the gracilis and sartorius muscles near knee; the lesion extends lower down and posteriorly and appears to fuse close to pes anserine insertion near the pulsation of the medial geniculate artery (Fig. 5, 6). Doppler USG showed no evidence of vascular involvement.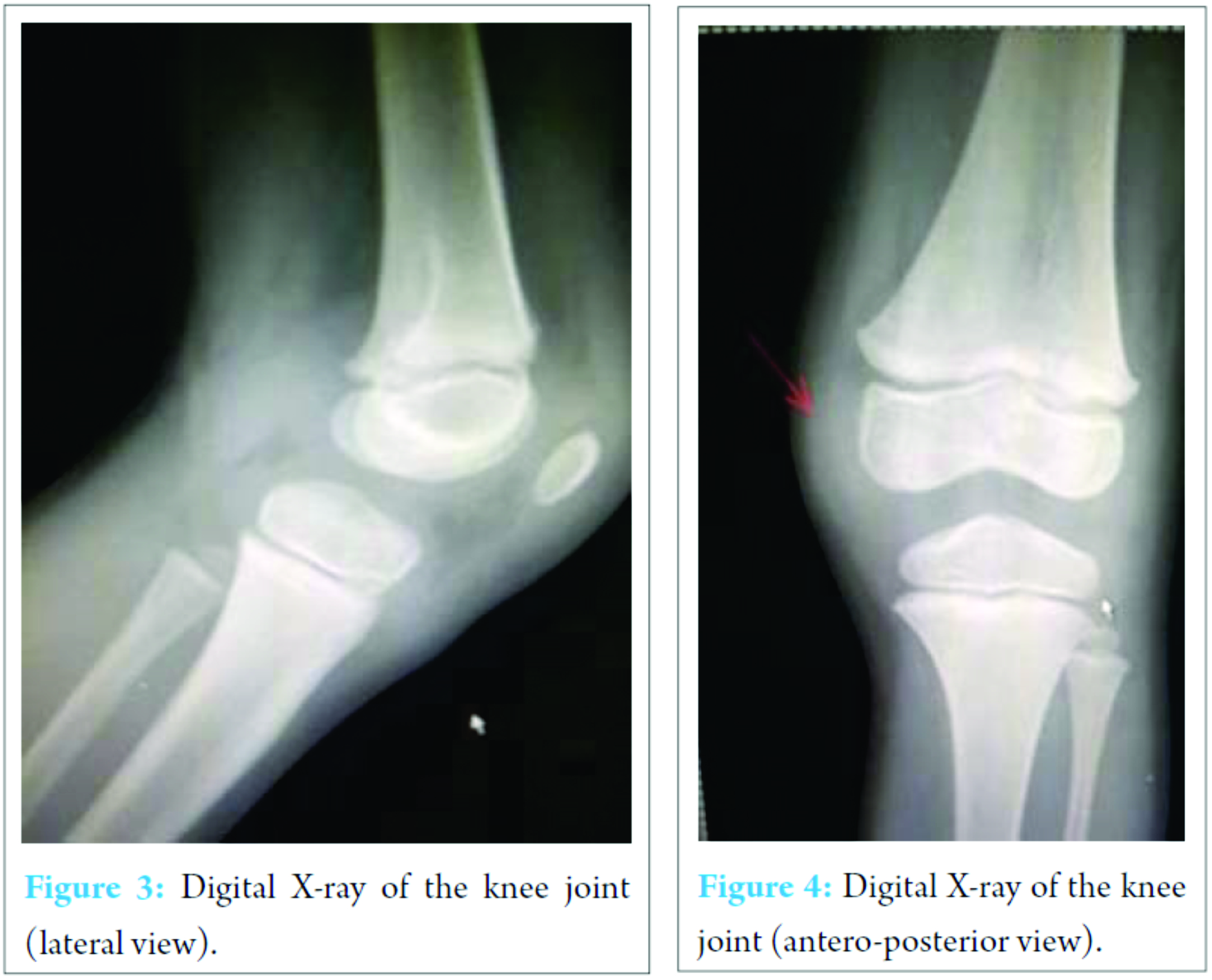
At surgery, posteromedial longitudinal incision was taken centered over the swelling. Swelling was exposed by blunt dissection. There was no sign of any tendon inflammation or adhesions. Grossly, the mass appeared completely encapsulated and contained in the semitendinosus tendon. The tendon sheath was incised longitudinally, and the swelling was delivered intact after dissecting it from the tendon taking care not to damage the tendon. On incising, the mass a transparent gelatinous fluid spilled out indicating a ganglion cyst. The tendon sheath was repaired. The wound was closed in layers. The skin wound healed with the secondary intention (Fig. 7). Follow-up USG was done to confirm complete removal of the ganglion cyst (Fig. 8, 9).
Follow-up USG was done to confirm complete removal of the ganglion cyst (Fig. 8, 9).
Discussion
Ganglion cysts are common tumour-like benign lesions in the soft tissues usually located around the joint capsules and tendon sheaths. Conventionally, they are classified on the basis of their origin: Tendon sheath, joint, bone, or soft tissue. Incidence of an intratendinous ganglion cyst is relatively rare [3, 4].
Lece´ne [5] was the first to report intratendinous cyst within the common extensor tendon of the middle finger. Since then there are multiple references in the literature of the intratendinous cysts mostly of the upper limbs [4, 6, 7, 8]. Intratendinous cysts of the lower extremities are extremely rare, and there are only few cases reported so far [9, 10, 11, 12, 13, 14].
In 2010 Kim et al. [15] and in 2014, Ananthi et al. [12] reported ganglion cyst in semimembranosus tendon.
USG and magnetic resonance imaging (MRI) can differentiate a ganglion cyst from other soft tissue lesions and provide excellent information about the location and dimensions of the lesion along with its margins especially intratendinous cysts [1, 3, 16].
Etiology of intratendinous ganglion cysts is presently unclear, and most probably recurrent injury to the tendon followed by cystic degeneration is the cause [13]. In cases where no traumatic recurrent history is present probably, a congenital anomaly may be the cause [14]. Mucinous fluid is rich in hyaluronic acid, albumin, globulin, and glucosamine [17]. Treatment options include aspiration of the cyst with or without infiltration with steroid locally. Excision of the cyst is usually the treatment the choice. Recurrence of ganglion cysts has been reported in literature, which may be due to partial surgical excision with a recurrence rate of 4-40% [8, 18, 19, 20].
To our knowledge, this the first reported case of intratendinous cyst of the semitendinosus tendon.
Conclusion
Intratendinous ganglion cyst is a relatively uncommon lesion. Incidence of the upper limb is more common than lower limbs. All cysts around the joints and tendons should undergo USG evaluation both preoperatively as well as postoperatively. We have presented the first case report of an intratendinous ganglion cyst of the semitendinosus tendon with findings using USG.
Clinical message
Finding and removing a cyst is a routine procedure, but attention should be given toward its etiology and pathogenesis. Benign ganglion cysts are extremely rare in tendons especially in lower limbs, but this differential should be kept in mind when a lower limb cyst is presented. It is better to use USG/MRI imaging (non-invasive diagnostic tools) to ascertain the pathology before putting the patient under the knife.
Reference
1. McCarthy CL, McNally EG. The MRI appearance of cystic lesions around the knee. Skeletal Radiol 2004;33(4):187-209.
2. Resnick DL, Kang HS, Pretterklieber ML. Internal Derangements of Joints. 2nd ed. Philadelphia, PA: Saunders, Elsevier; 2007. p. 1589-1598.
3. Costa CR, Morrison WB, Carrino JA, Raiken SM. MRI of an intratendinous ganglion cyst of the peroneus brevis tendon. AJR Am J Roentgenol 2003;181(3):890-891.
4. Rayan GM. Intratendinous ganglion. A case report. Orthop Rev 1989;18(4):449-451.
5. Lece´ne MP. Three cases of pseudocystic gelatinous degeneration of juxta-articular connective tissue and tendon tissue. Bull Mem Soc Nat Chir 1927;53:2.
6. Ikeda K, Tomita K, Matsumoto H. Intratendinous ganglion in the extensor tendon of a finger: A case report. J Orthop Surg (Hong Kong) 2001;9(2):63-65.
7. Young SC, Freiberg A. A case of an intratendinous ganglion. J Hand Surg Am 1985;10(5):723-734.
8. Seidman GD, Margles SW. Intratendinous ganglia of the hand. J Hand Surg Am 1993;18(4):707-710.
9. Graves FT. A ganglion in the muscle belly of peroneus longus. Br J Surg 1956;43(180):438-439.
10. Siebert CH, Kaufmann A, Niedhart C, Heller KD. The quadriceps tendon cyst: an uncommon cause of chronic anterior knee pain. Knee Surg Sports Traumatol Arthrosc 1999;7(6):349-351.
11. Schram AJ, Kirschenbaum SE. Presentation of a unique ganglionic cyst. J Foot Surg 1988;27(6):530-532.
12. Ananthi Kumarasamy S, Kannadath BS, Soundamourthy S, Subramanian A, Sinhasan SP, Bhat RV. Semimembranosus ganglion cyst. Anat Cell Biol 2014;47(3):207-209.
13. Robertson DE. Cystic degeneration of the peroneus brevis tendon. J Bone Joint Surg Br 1959;41-B(2):362-364.
14. Pedrinelli A, Castellana FB, Bragança de Vasconcellos Fontes R, Coelho RF, Alvaro de Menezes LA. Anterior cruciate ligament ganglion: case report. Sao Paulo Med J 2002;120(6):195-197.
15. Thornburg LE. Ganglions of the hand and wrist. J Am Acad Orthop Surg 1999;7(4):231-238.
16. Kishimoto K, Akisue T, Fujimoto T, Kawamoto T, Hara H, Hitora T, et al. Intra-tendinous ganglion in the long head of the biceps humeri. Skeletal Radiol 2008;37(3):263-265.
17. Kim SK, Park JM, Choi JE, Rhee SK, Shim SI. Intratendinous ganglion cyst of the semimembranosus tendon. Br J Radiol 2010;83(988):e79-e82.
18. Nahra ME, Bucchieri JS. Open and arthroscopic excision of ganglion cyst and related tumors. In: Wiesel S, editor. Operative Techniques in Orthopaedic Surgery. Vol. 3. Philadelphia, PA: Lippincott Williams & Wilkins; 2011. p. 3010-3021.
19. Rozbruch SR, Chang V, Bohne WH, Deland JT. Ganglion cysts of the lower extremity: An analysis of 54 cases and review of the literature. Orthopedics 1998;21(2):141-148.
20. Pontious J, Good J, Maxian SH. Ganglions of the foot and ankle. A retrospective analysis of 63 procedures. J Am Podiatr Med Assoc 1999;89(4):163-168.
| How to Cite This Article: Maheshwari P, Maheshwari P, Bapna P. Case Report: Intratendinous Ganglion Cyst of the Semitendinosus Tendon: First Reported Case and Literature Review. Journal of Orthopaedic Case Reports 2016 Nov-Dec;6(5):85-88. Available from: https://www.jocr.co.in/wp/2016/11/10/2250-0685-646-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com