[box type=”bio”] What to Learn from this Article?[/box]
Modified tension- slide technique of distal biceps tenodesis described in this article makes this procedure safe, reliable, easy to reproduce, cost-effective, less time consuming and effective method in achieving the goals of a strong fixation and an anatomic repair of the tendon back into its native footprint.
Case Report | Volume 6 | Issue 5 | JOCR November-December 2016 | Page 104-108 | Jagadish Prabhu, Mohammed Khalid Faqi, Fahad Al-Khalifa, Rashad Khamis Awad DOI: 10.13107/jocr.2250-0685.656
Authors: Jagadish Prabhu[1], Mohammed Khalid Faqi[1], Fahad Al-Khalifa[1], Rashad Khamis Awad[1]
[1]Department of Orthopedics, Bahrain Defence Force Hospital – Royal Medical Services, Kingdom of Bahrain.
Address for Correspondence
Dr. Jagadish Prabhu,
Department of Orthopedics, Bahrain Defence Force Hospital – Royal Medical Services, Riffa, Kingdom of Bahrain.
E-mail: drjags@rediffmail.com
Abstract
Introduction: Many surgical techniques have been described in the literature. In this article, we describe surgical technical details along with tips and tricks of distal biceps tendon tenodesis using the EndoButton and tension – slide technique, a modification of the suspensory cortical button technique, which allows the surgeon to tension and repairs the biceps tendon through the single longitudinal anterior incision. This modification in surgical technique of using dual implants, i.e., EndoButton and interference screw as fixation tools and concept of tendon sliding principle made this procedure unique. In this article, we describe surgical technique along with tips and tricks of distal biceps tendon tenodesis using the EndoButton and tension – slide technique and also discussed about modification of EndoButton technique reported in many other articles to overcome the possible complications.
Case Report: We report six consecutive patients, presented with distal biceps tendon rupture (4 acute; 2 chronic cases) between June 2013 and March 2015, who underwent single-incision, anatomical distal biceps tenodesis procedure with bicortical EndoButton and tenodesis screw using tension slide technique. Radiographs were taken immediate post-operative to document for displacement or loosening of EndoButton if any.
Conclusion: The use of an EndoButton and an interference screw for repairing distal biceps tendons have been previously described. We describe a modification of originally described technique which is worth considering, as it provides two levels of fixation, whilst avoiding possible complications of such procedures. It is ideal for repairing both acute and chronic ruptures, without the need for allograft or autograft augmentation and describes detailed technical steps to avoid possible iatrogenic complications.
Keywords: Biceps tendon repair, EndoButton, sliding technique.
Introduction
DDistal biceps tendon rupture is a relatively uncommon injury. It usually occurs in middle-aged men who sustain a sudden force to a flexed arm. This injury represents only 3% of all injuries to the biceps tendon; 96% of such injuries involve the long head, and 1% involve the short head [1, 2].
Anatomic repair of the ruptured distal biceps tendon to the radial tuberosity is recommended to prevent the loss of strength and endurance in forearm supination and elbow flexion [2, 3, 4, 5]. Repair of distal biceps tendon rupture using bone tunnels, suture anchors, interference screws or the EndoButton has been described in many articles [2, 6, 7, 8, 9].
EndoButton repair of distal biceps tendon ruptures was first described by Bain and colleagues in 2000 [7]. Subsequent clinical and biomechanical studies have demonstrated high patient satisfaction, a very low incidence of complications and higher load to failure when compared to other techniques [7, 8, 10, 11, 12, 13].
In this article, we describe our modified EndoButton and tension – slide technique for distal biceps tenodesis, along with tips and tricks aimed to avoid the possible complications associated with this procedure.
Case Report
We report six consecutive patients, presented with distal biceps tendon rupture (4 acute; 2 chronic cases) between June 2013 and March 2015, who underwent single-incision, anatomical distal biceps tenodesis procedure with bicortical EndoButton and tenodesis screw using tension slide technique (TST). Radiographs were taken immediate post-operative to document for displacement or loosening of EndoButton if any.
Surgical technique
All surgical procedures were done under general anesthesia, with the arm placed onto an arm table and the elbow extended with the tourniquet inflated. A longitudinal 4-5 cm anterior incision starting at the antecubital fossa and extending distally along the ulnar border of the brachioradialis, exploiting the interval between the brachioradialis and pronator teres with radial (lateral) retraction of the brachioradialis and medial retraction of the pronator teres. The lateral antebrachial cutaneous nerve is identified and protected as it exists between the biceps and the brachialis at the antecubital fossa. Ligation of the recurrent branch of the radial artery minimizes hematoma formation and may protect against heterotopic ossification (HO). The lateral antebrachial cutaneous nerve and the posterior interosseous nerve (PIN) are protected using limiting forceful lateral retraction and maintaining supination, respectively.
The distal biceps tendon was identified and retrieved into the wound. Flexing the elbow and using a retractor to elevate the tissue of the distal brachium anteriorly can accomplish this by allowing better exposure. The tendon can be adherent to the adjacent tissues or the lacertus fibrosus. This may require limited tenolysis to mobilize the tendon stump.
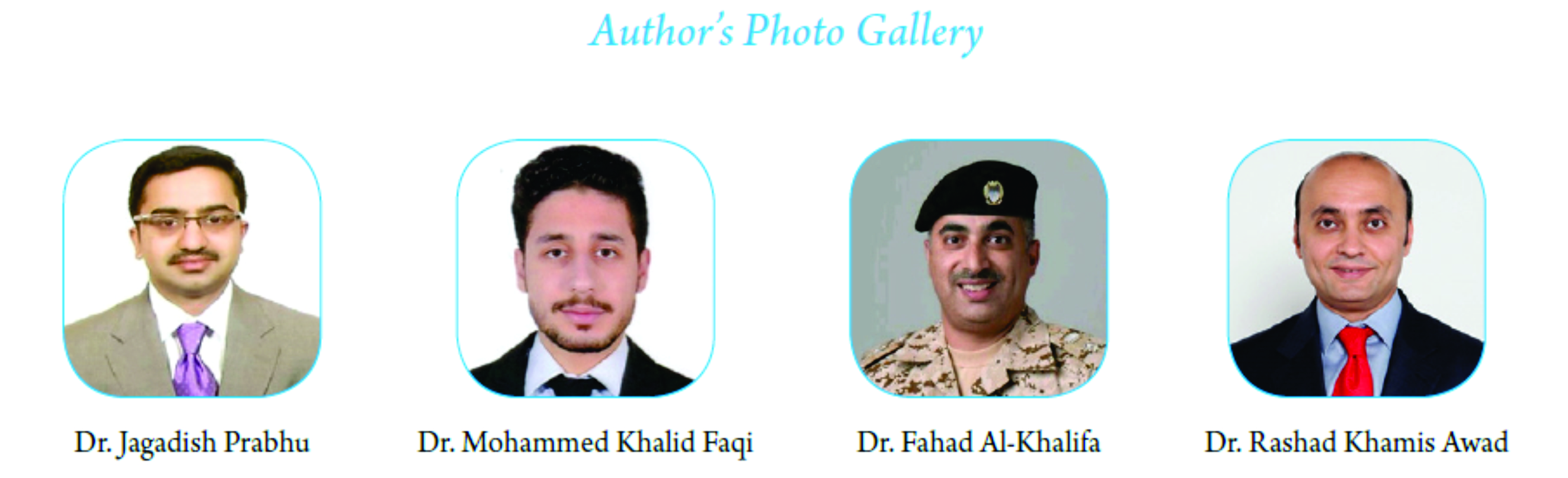
Once the tendon is isolated, a number 5 synthetic polyester suture (Ethibond Excel, Ethicon Inc.; Johnson and Johnson, USA) is woven into the distal biceps tendon using Krackow technique or whipstitch suture technique (Fig. 1a and 2a). We used 4 holed EndoButton without continuous loop (4.0 mm × 12 mm Endo-Button CL Ultra, Smith and Nephew, Andover, MA, USA). One limb of the suture from the tendon end was threaded through the central two holes of the EndoButton (inside out – outside in). The other suture end from the tendon was passed through the terminal two holes of the EndoButton in a reverse manner, i.e., from outside in – inside out) (Fig. 1b). It is important to make certain that the suture limbs are not tangled.
With the elbow in full extension and full supination, the radial tuberosity was exposed and debrided of any remaining soft tissue. Under c-arm image guidance, a 2.7 mmx 15″ guide wire is passed through the radial tuberosity, aiming 30° ulnar, with the forearm in maximum supination so that guide pin trajectory is away from PIN (Fig. 1c and 2c). Fluoroscopic images were used to confirm that the guide pin is passed through center of the tuberosity and crossed only 2-3 mm beyond the posterior cortex. Then, the size of the tendon we prepared was measured, using tendon-sizing block (Fig. 2b). Usually, the size of the tendon is around 7-8 mm. If the size of the tendon is 8 mm, same size endoscopic cannulated drill is passed over the guide wire to drill the anterior cortex and intramedullary canal (Fig. 1d). Then, a 4.5 mm EndoButton drill is used over the guide wire to drill the posterior cortex (Fig. 1e). The guide wire and drill were then removed and copious irrigation of the wound was done to remove bone dust and fragments.
Care is taken to ensure that the tendon is appropriately aligned. Placing the elbow in 20-30° flexion and full supination, hold the looped EndoButton at the tip of long thin straight artery forceps or EndoButton holder and pass through both drill holes to deliver the EndoButton to the dorsal aspect of the proximal radius (Fig. 1f). Once the button cleared the posterior cortex, the deployment instrument was removed while the button deployed itself, locking into place on the posterior cortex. Pulling on the sutures shuttles the biceps tendon into the radius. The sutures were tensioned until the tendon was in contact with the posterior cortex. By placing tension onto the trailing suture, the EndoButton locks into position and prevents proximal migration of the tendon (Fig. 1g). Fluoroscopy is useful to assess the position of the EndoButton as it is advanced through the radius and locked into position (Fig. 1h, 3a and b). Using both suture threads, knots are tied under tension after back passing one of the suture threads through the biceps tendon just adjacent to anterior cortex (Fig. 1h).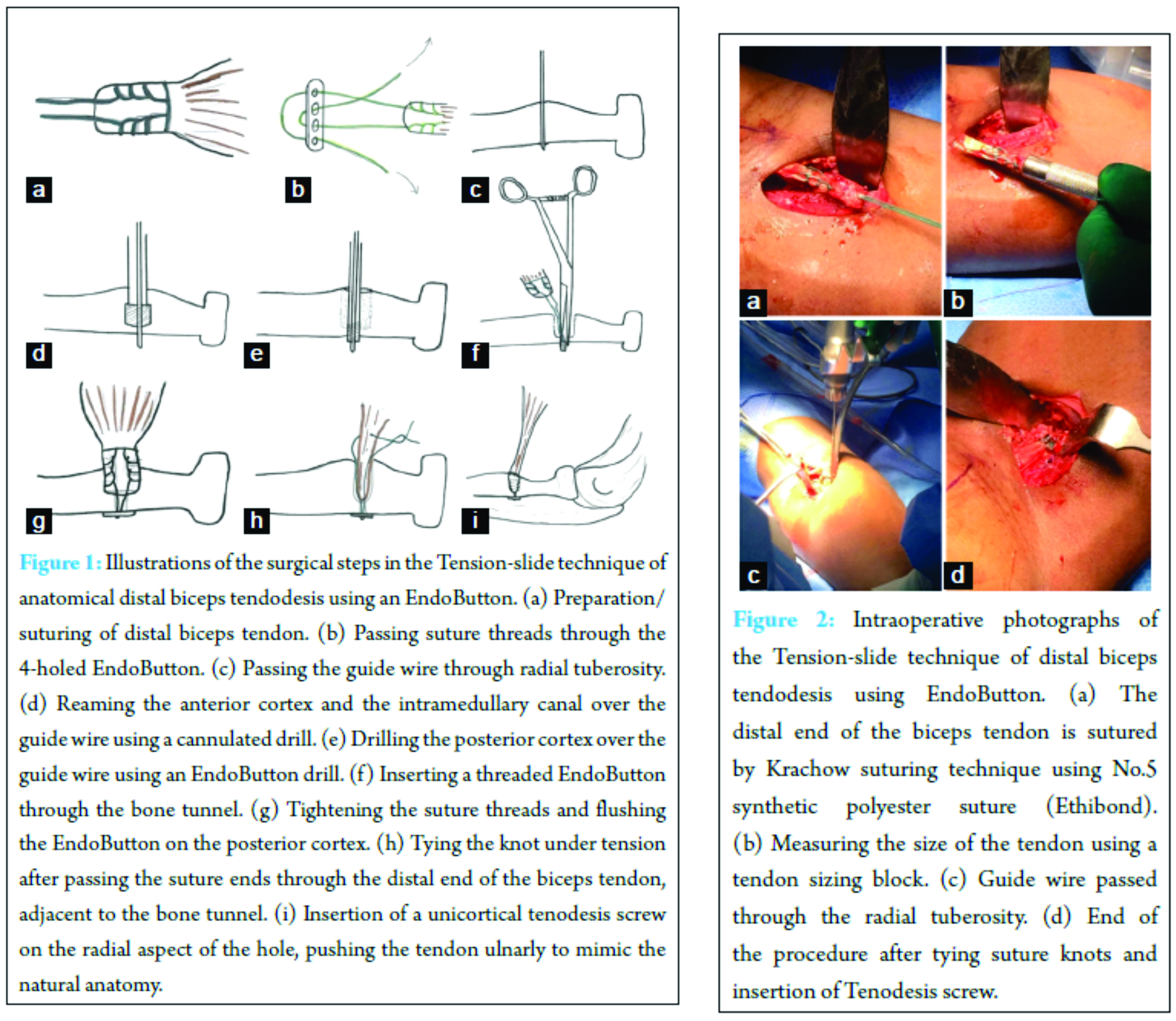
A 7 mm × 10 mm (one size less than size of the tendon) unicortical interference screw (PEEK Tenodesis Screw, Arthrex Inc. Naples, FL, USA) was then inserted on the radial aspect of the hole, pushing the tendon ulnar to mimic the natural anatomy and potentially increase supination strength (Fig. 1i and 2d).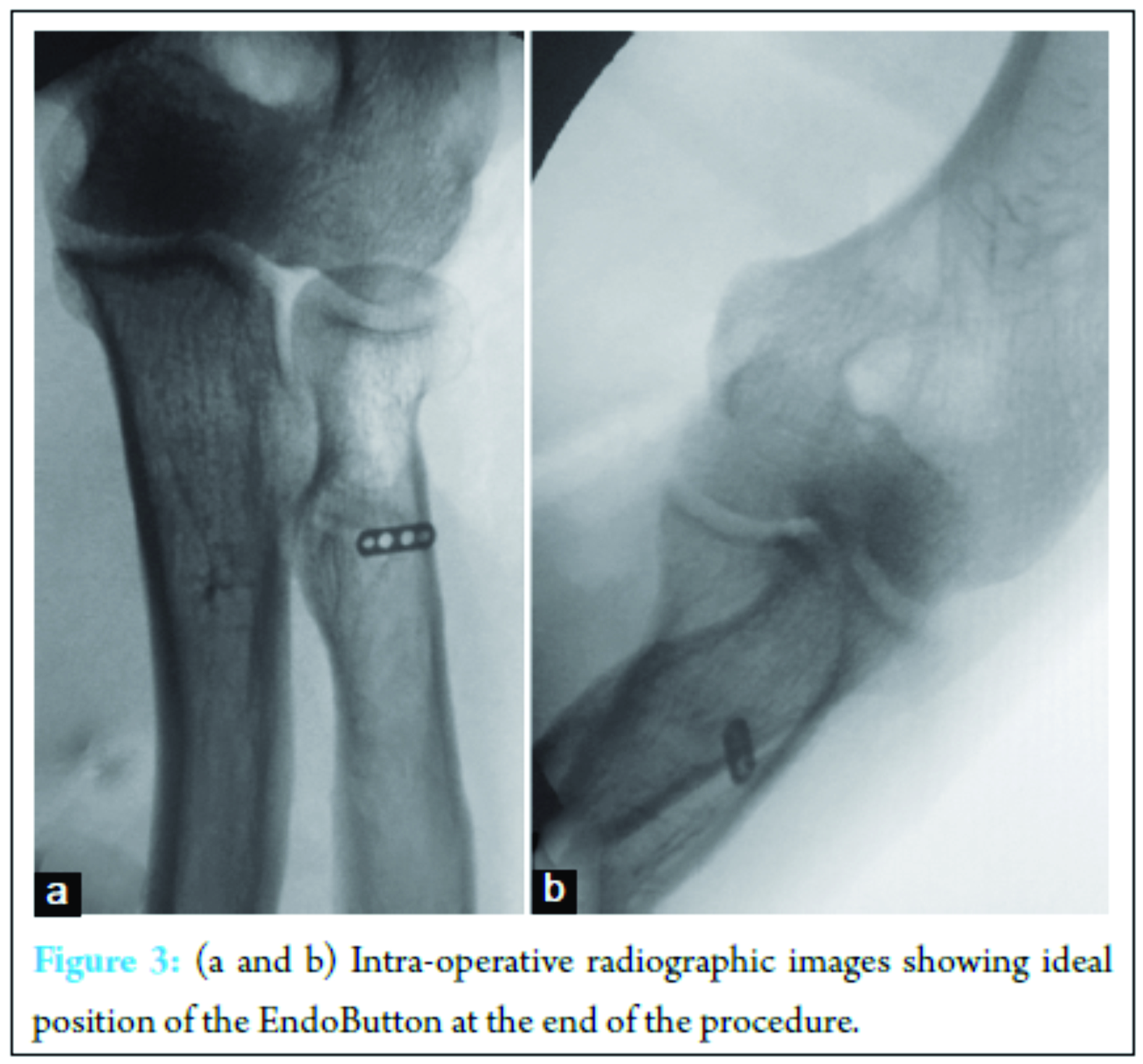
Post-operative Management
Postoperatively, patients were placed in a soft dressing, and early passive range of motion (ROM) exercises started from day one and gravity-assisted flexion and extension started after 2 weeks. Active strengthening exercises started at 8 weeks, with an expected return to heavy activities at 3-5 months, depending on the patient. Elbow and forearm ROM were recorded at regular intervals.
Results
All patients were satisfied with their outcome and were able to return to activities of daily living. No neurovascular complications occurred. There was no clinical or radiological evidence of radioulnar synostosis in any patient. All patients had an intact biceps tendon and had a return of grade 5 power. The average range of flexion was from 5° to 130°. The average supination was 80° and average pronation 75°. None of the patients suffered failure of fixation with immediate active motion. Patients achieved near full ROM and near complete return of strength and endurance without any complications.
Discussion
Surgical techniques for the repair of distal biceps tendon tears using an EndoButton have been previously described [7, 8, 10, 11]. In this article, we describe a technique in which we consider the best possible modifications of the previously described techniques, aiming to simplify the surgical procedure, achieve a very strong fixation, excellent patient outcome, and avoid the possible surgical complications.
The technique, we describe, is minimally invasive as it requires only a small anterior longitudinal incision [14], through which the surgeon can identify and repair the biceps tendon. This single incision technique has an advantage over the double incision technique described by Boyd and Anderson, which has the risk of HO, radioulnar synostosis, stiffness, and PIN palsy [15, 16].
We favor the longitudinal incision, rather than the transverse incision which has been associated with a high rate of neurologic complications [17]. The transverse incision can be used in case of acute injuries, where the avulsed distal biceps tendon can be found without much exploration and tissue retraction. On the other hand, in chronic biceps tendon rupture, the incision has to be extended proximally to find the retracted tendon and retrieve it back to its anatomical site. Moreover, having the transverse skin incision at the antecubital crease risks drilling the cortex with distally directed trajectory, which in turn increase the risk of damaging the PIN.
An anatomic study evaluating the safest trajectory of guide pins during biceps repair found that avoiding a radially directed trajectory reduces the risk of injury to the PIN. Moreover, the authors found that the best way to prevent nerve injury was aiming guide pin 30° ulnarly through center of radial tuberosity, with forearm in maximum supination, which increases the distance between the guide wire and the PIN [7, 9, 18]. Drilling over distally or radially directed guide wire, placed the PIN at significant risk of injury, compared with an ulnar or direct anterior to posterior trajectory [7, 18].
Another possible complication is sustaining a proximal radius fracture. It is important that the bony bridge between the anterior cortical window and the posterior drill hole is adequate to minimize the risk of fracture. Irrigation of the wound after drilling, single incision approach, ligation of the recurrent branch of the radial artery and a minimally invasive technique, all reduce the risk of HO [19].
We recommend the use of a 4-holed EndoButton, rather than the 2-holed. We believe that the 4-holed EndoButton provides a greater surface area of contact, thus allowing distribution of stress on posterior cortex through suture threads. This decreases the possibility of the EndoButton cutting through the outer cortex. The suture threads slide freely since a single thread passes through each hole. On the other hand, two threads have to be passed through each hole in the 2-holed EndoButton, which may restrict the free sliding.
Biomechanical studies have proven that the TST maintains the strength of a suspensory cortical button fixation and significantly reduces gap formation and motion at the repair site [20]. Mazzocca et al. [8] conducted a biomechanical study measuring cyclical load to failure in four techniques for distal biceps brachii tendon repair. The EndoButton technique had a statistically significant (P < 0.001) highest load to failure (440 N) compared with suture anchor (381 N), bone tunnel (310 N), and the interference screw (232 N). EndoButton and TST have been shown to have the highest ultimate tensile load [8, 13]. Clinical studies with the EndoButton have also demonstrated good results with few complications [7]. Another advantage is the ability to start early active ROM exercises compared to other fixation methods.
The advantages of the TST include the ability to tension the repair from an anterior incision, and there is no need to predetermine the length of suture between the button and the biceps tendon stump.
We recommend using C-arm image/fluoroscopy, while passing the guide wire, drilling the cortex and confirming the position of EndoButton before tightening the sutures. This avoids mal trajectory of the guide wire, blowing out the posterior cortex with first drill, intramedullary dislodgement of the EndoButton just before tightening the suture threads and inter-positioning of the PIN or soft tissue between the posterior cortex and the EndoButton, which is depicted by a gap between the EndoButton and the posterior cortex in a lateral view image.
Due to the fact that number 5 synthetic polyester sutures were used to secure the EndoButton, and because the tendon is positioned within the intramedullary canal, allowing maximum surface area between the tendon and the bone, we consider this fixation technique very strong and reliable. That is why we can start early ROM exercises after this procedure compared to other fixation techniques.
In this technique, we use unicortical interference/tenodesis screw in addition to an EndoButton, which is inserted on the radial aspect of the hole, pushing the tendon ulnar to mimic the natural anatomy and potentially increasing the supination strength.
As mentioned earlier, many surgeons used a combination of an EndoButton and interference screws for this procedure, in which they maintained tension on the suture after deploying the EndoButton, followed by insertion of the interference screw. This technique acts as a single unit of fixation. On the contrary, in our technique, the suture knot is tied under tension after back passing the suture through the tendon itself, which itself is an independent fixation. The tenodesis screw inserted acts like a secondary fixation. Hence, we achieve two different independent fixations, which act synergistically and ensures the fixation is held in place, even if one of the two fixations fail.
Conclusion
The use of an EndoButton and an interference screw for repairing distal biceps tendons has been previously described. We describe a modification of originally described technique which is worth considering, as it provides two levels of fixation, whilst avoiding possible complications of such procedures. It is ideal for repairing both acute and chronic ruptures, without the need for allograft or autograft augmentation and describes detailed technical steps to avoid possible iatrogenic complications.
Clinical Message
Even though our study group is small and needs further extensive research considering a larger study group, long-term evaluation along with biomechanical studies to validate our surgical technique further, we believe that these surgical tips and tricks will definitely help the surgeons dealing with such cases.
Clinical message
Even though our study group is small and needs further extensive research considering a larger study group, long-term evaluation along with biomechanical studies to validate our surgical technique further, we believe that these surgical tips and tricks will definitely help the surgeons dealing with such cases.
References
1. Dobbie RP. Avulsion of the lower biceps brachii tendon: Analysis of fifty-one previously unreported cases. Am J Surg 1941;51:662-683.
2. Baker BE, Bierwagen D. Rupture of the distal tendon of the biceps brachii. Operative versus non-operative treatment. J Bone Joint Surg Am 1985;67(3):414-417.
3. D’Alessandro DF, Shields CL Jr, Tibone JE, Chandler RW. Repair of distal biceps tendon ruptures in athletes. Am J Sports Med 1993;21(1):114-119.
4. Morrey BF, Askew LJ, An KN, Dobyns JH. Rupture of the distal tendon of the biceps brachii. A biomechanical study. J Bone Joint Surg Am 1985;67(3):418-421.
5. Rantanen J, Orava S. Rupture of the distal biceps tendon. A report of 19 patients treated with anatomic reinsertion, and a meta-analysis of 147 cases found in the literature. Am J Sports Med 1999;27(2):128-132.
6. Limpisvasti O, Singer DI. Single-incision suture anchor repair of distal biceps tendon rupture. Tech Hand Up Extrem Surg 2003;7(3):82-86.
7. Bain GI, Prem H, Heptinstall RJ, Verhellen R, Paix D. Repair of distal biceps tendon rupture: a new technique using the Endobutton. J Shoulder Elbow Surg 2000;9(2):120-126.
8. Mazzocca AD, Burton KJ, Romeo AA, Santangelo S, Adams DA, Arciero RA. Biomechanical evaluation of 4 techniques of distal biceps brachii tendon repair. Am J Sports Med 2007;35(2):252-258.
9. Saldua N, Carney J, Dewing C, Thompson M. The effect of drilling angle on posterior interosseous nerve safety during open and endoscopic anterior single-incision repair of the distal biceps tendon. Arthroscopy 2008;24(3):305-310.
10. Greenberg JA, Fernandez JJ, Wang T, Turner C. EndoButton-assisted repair of distal biceps tendon ruptures. J Shoulder Elbow Surg 2003;12(5):484-490.
11. Hallam P, Bain GI. Repair of chronic distal biceps tendon ruptures using autologous hamstring graft and the Endobutton. J Shoulder Elbow Surg 2004;13(6):648-651.
12. Kettler M, Lunger J, Kuhn V, Mutschler W, Tingart MJ. Failure strengths in distal biceps tendon repair. Am J Sports Med 2007;35(9):1544-1548.
13. Spang JT, Weinhold PS, Karas SG. A biomechanical comparison of EndoButton versus suture anchor repair of distal biceps tendon injuries. J Shoulder Elbow Surg 2006;15(4):509-514.
14. Kelly E, O’Driscoll S. Mini-incision technique for acute distal biceps tendon repair. Tech Shoulder Elbow Surg 2002;3(1):57-62.
15. Failla JM, Amadio PC, Morrey BF, Beckenbaugh RD. Proximal radioulnar synostosis after repair of distal biceps brachii rupture by the two-incision technique. Report of four cases. Clin Orthop Relat Res 1990;253:133-136.
16. Kelly EW, Morrey BF, O’Driscoll SW. Complications of repair of the distal biceps tendon with the modified two-incision technique. J Bone Joint Surg Am 2000;82-A(11):1575-1581.
17. El-Hawary R, Macdermid JC, Faber KJ, Patterson SD, King GJ. Distal biceps tendon repair: comparison of surgical techniques. J Hand Surg Am 2003;28(3):496-502.
18. Lo EY, Li CS, Van den Bogaerde JM. The effect of drill trajectory on proximity to the posterior interosseous nerve during cortical button distal biceps repair. Arthroscopy 2011;27(8):1048-1054.
19. Wysocki RW, Cohen MS. Radioulnar heterotopic ossification after distal biceps tendon repair: results following surgical resection. J Hand Surg Am 2007;32(8):1230-1236.
20. Sethi P, Obopilwe E, Rincon L, Miller S, Mazzocca A. Biomechanical evaluation of distal biceps reconstruction with cortical button and interference screw fixation. J Shoulder Elbow Surg 2010;19(1):53-57.
| How to Cite This Article: Prabhu J, Faqi MK, Al-Khalifa F, Awad RK. Modified Tension – Slide Technique for Anatomical Distal Biceps Tenodesis using a Bicortical Endobutton and a Tenodesis Screw. Journal of Orthopaedic Case Reports 2016 Nov-Dec;6(5):104-108. Available from: https://www.jocr.co.in/wp/2016/11/10/2250-0685-656-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com