[box type=”bio”] Learning Points for this Article: [/box]
The Odontoideum bone is a rare malformation that can decompensate at any age and involve functional and vital prognosis.
Case Report | Volume 7 | Issue 4 | JOCR July – August 2017 | Page 3-5| Lassaad Hassini, Mohamed Ali Khalifa, Zeineb Alaya, Mohamed Laaziz Ben Ayeche, Walid Osman, Mourad Mtaoumi. DOI: 10.13107/jocr.2250-0685.822
Authors: Lassaad Hassini[1], Mohamed Ali Khalifa[1], Zeineb Alaya[2], Mohamed Laaziz Ben Ayeche[1], Walid Osman[1], Mourad Mtaoumi[1]
[1] Department of Orthopaedics, Faculty of Medicine of Sousse, Sahloul Hospital, Sousse, Tunisia.
[2] Department of Rheumatology, Faculty of Medicine of Sousse, Farhat Hached Hospital, Sousse, Tunisia.
Address of Correspondence
Dr. Lassaad Hassini, Department of Orthopaedics, Faculty of Medicine of Sousse, Sahloul Hospital, Sousse, Tunisia.
E-mail: lassaadhassini@hotmail.fr
Abstract
Introduction: Odontoideum bone or the mobile odontoid process is one of the rarest malformations of the cervico-occipital hinge. It exposes to the atlo-axial instability and to the risk of bulbo-medullary compression threatening then the vital and functional prognosis. We report the case of a 16-year-old patient who was the victim of a raod accident resulting in acervical spine injury. Radiological investigation found an odontoideum bone malformation associated with C1C2 dislocation.
Case Report: A 16-year-old patient with no medical history had a road accident. Clinical evaluation found an incomplete tetraplegia.The imaging has revealed an atlo-axoidal dislocation with aspinal cord compression. Furthermore, radiological exams relvealed an odentoideum bone. A transcranial traction by a Gardner stirrup was set for 15 days to obtain a progressive reduction of the displacement. A full neurological recovery (FB-FD) was obtained.The patient was then operated to stabilize the reduction. A C1-C2 posterior zygapophyseal arthrodesis was performed. An autograft harvested from the iliac crest was used. Complementary open reduction and fixation of the cervico-occipital hinge was made using lamellar hooks and compression rods. At the 18-month follow-up, the clinical examination found no neurological deficiency and the plain radiography showed a complete fusion of the arthrodesis.
Conclusion: Odontoideum bone is a rare and potentially life-threatening malformation. It is most often asymptomatic but symptoms could occur any time after a benign trauma. The prognosis mainly depends on the precocity of the management. Preventive surgery is recommended byseveral authorsin case of instability.
Keywords: Cervico-occipital hinge, trauma, odontoideum bone, c1c2 dislocation.
Introduction
Odontoideum bone is a malformation of the cervico-occipital hinge. It results from a non-union of the center of ossification of the odontoid to the body of the axis. It exposes to the atlo-axial instability and to the vital risk of bulbo-medullary compression. It is difficult to know the actual incidence of this malformation since many cases remain asymptomatic. Symptoms occur at any age and the clinical presentation is variable. We report the case of a patient with a tetraplegia resulting from a C1C2 duslocation. Odontoideum bone was diagnosed was associated to this injury.
Case Report
A 16-year-old patient with no medical history had a road accident. Clinical evaluation found an incomplete tetraplegia. Plain radiography showed anodontoidoaxoidal dislocation (Fig. 1). The computed tomography (CT) scan confirmed the injury and revealed an associated odontoideum bone (Fig. 2). 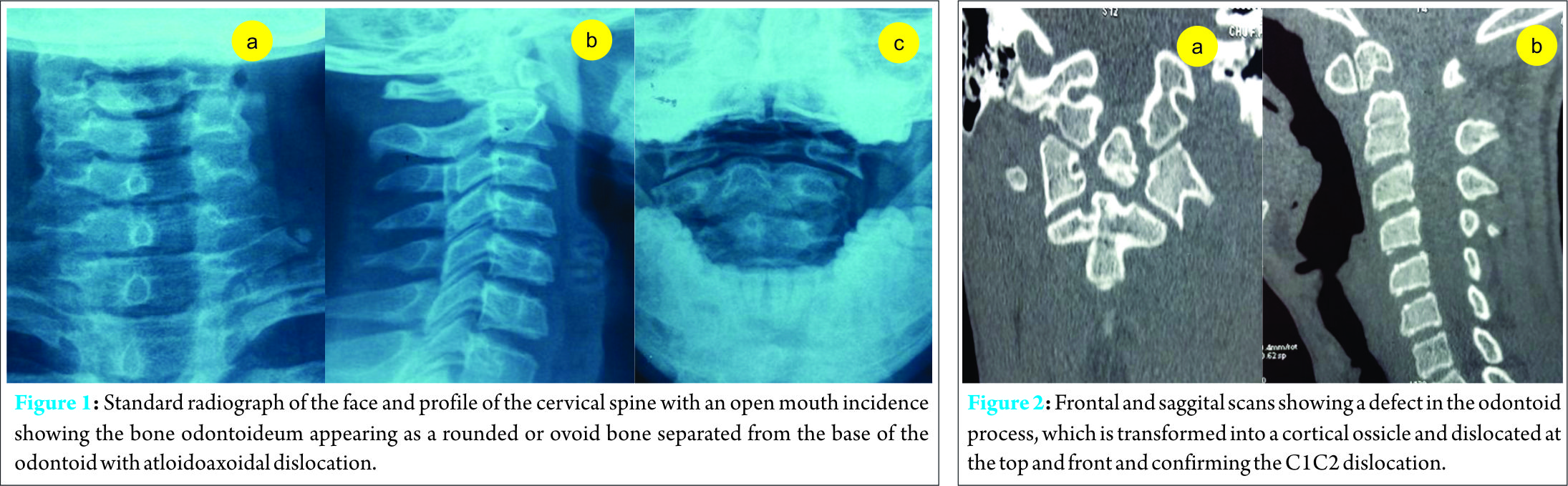 Cervical magnetic resonance imaging (MRI) showed a medullary contusion with major compression of the bulbo-medullary junction (Fig. 3). A respiratory failure was associated and the patient was initially managedin the intensive care unit. Urgent cervical spine surgery was not possible because of the general condition of the patient. A progressive reduction using a transcranial traction by a Gardner stirrup wasthen set for 15 days. The evolution was marked by complete neurological recovery (FB-FD) with improvement of the general condition of the patient. The patient was operated in prone position with the transcranial traction maintained. The surgical procedure consisted of exposure of the posterior arches of C1 and C2 with posterior osteosynthesis by C1 and C2 laminar hooks mounted on compression on stems (Vertex, Medtronic®). The arthrodesis was reinforced using an iliac graft interposed between the plates of C1 and C2 previously revived (Fig. 4).
Cervical magnetic resonance imaging (MRI) showed a medullary contusion with major compression of the bulbo-medullary junction (Fig. 3). A respiratory failure was associated and the patient was initially managedin the intensive care unit. Urgent cervical spine surgery was not possible because of the general condition of the patient. A progressive reduction using a transcranial traction by a Gardner stirrup wasthen set for 15 days. The evolution was marked by complete neurological recovery (FB-FD) with improvement of the general condition of the patient. The patient was operated in prone position with the transcranial traction maintained. The surgical procedure consisted of exposure of the posterior arches of C1 and C2 with posterior osteosynthesis by C1 and C2 laminar hooks mounted on compression on stems (Vertex, Medtronic®). The arthrodesis was reinforced using an iliac graft interposed between the plates of C1 and C2 previously revived (Fig. 4).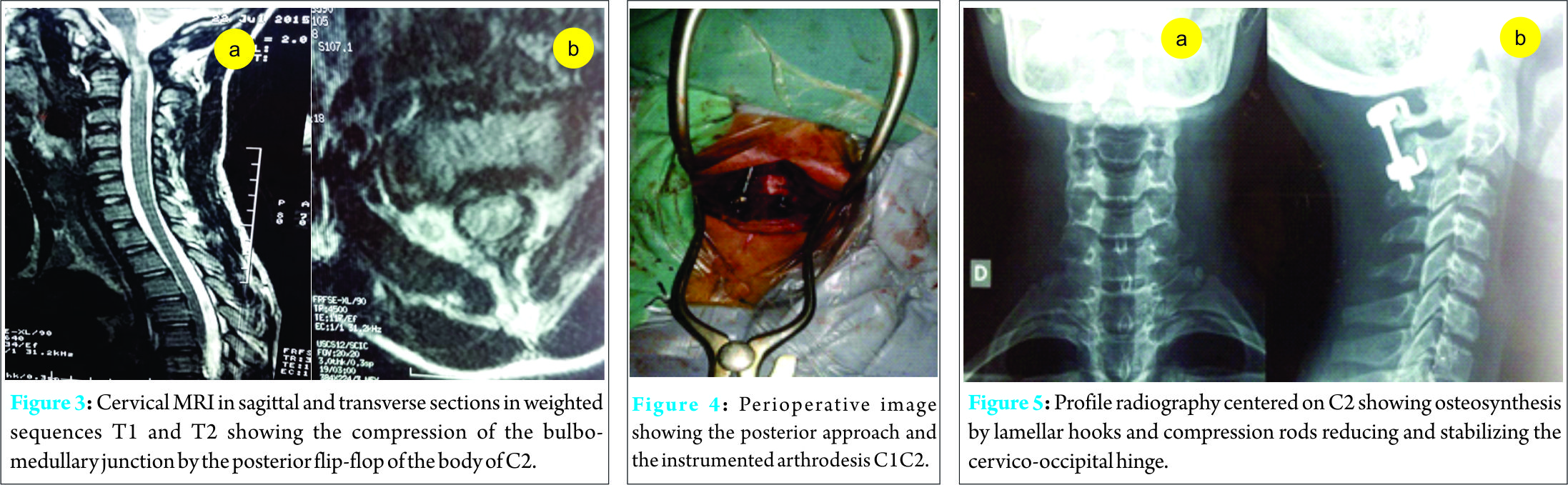 The postoperative follow-up was simple and the radiological control showed a perfect reduction of dislocation (Fig. 5). At the 18-month follow-up, the neurological evaluation is normal and the computed tomography (CT) scan showed a complete fusion of the posterior arthrodesis (Fig. 6).
The postoperative follow-up was simple and the radiological control showed a perfect reduction of dislocation (Fig. 5). At the 18-month follow-up, the neurological evaluation is normal and the computed tomography (CT) scan showed a complete fusion of the posterior arthrodesis (Fig. 6).
Discussion
Odontoideum Bone, first described by Giacomini in 1886, refers to the replacement of the odontoid apophysis by a small independent bone in the cranial position with respect to the axis. The pathogenesis of this condition remains a participant of debate since, for some authors, it would be of embryonic origin [2], while for others it would be of vascular or traumatic origin whose common point is the osseous necrosis [1,2,3,4,8]. Congenital theory is supported by the association of odontoideum bone with other congenital ailments such as Klippel–Feil syndrome, trisomy 21 or multiple epiphyseal dysplasia [6]. Furthermore, some familial cases were reported. A recent study further reinforces this theory: Of 18 cases of odontoideumbone only one was revealed posttraumatic [7]. Corinna et al. raised the possibility of development of an odontoideum bone years after a trauma following which explorations of the cervico-occipital hinge had been normal. They explained this by delayed bone remodeling related to vascular involvement during the trauma. The prevalence of odontoideum bone in the general population remains unknown due to the often asymptomatic nature of the malformation which may never occur (accidental discovery) or sometimes cause sudden death without the diagnosis being recognized. For the clinical picture, the mobile odontoid apophysis can be revealed by high cervicalgia, neck stiffness, torticollis, dizziness, motor or sensory motor impotence, as in the case of our observation [9]. Neurological examination may reveal a picture of myelopathy, radiculopathy, or cranial pairs [10]. Note that the severity of the clinical signs is not always correlated with the degree of atloidoaxoid instability [9]. The radiological assessment should include X-rays, cervical CT, and MRI. On plain radiographs, odontoideum bone appears as a rounded or ovoid bone, separated from the base of the odontoid. CT with multiplanar reconstruction is the key investigation. It allows agood study of the osseous structures of the cervico-occipital hinge confirming the diagnosis of odontoideum bone. It shows an abnormal appearance of the odontoid process, which is transformed into a corticalizedossicle, detached from the base of the odontoid, usually dislocated at the top and front. C1-C2 diastasis is diagnosed when the distance between C1 and odentoideum bone is >3mm in adults and 4-5mm [11] in children. MRI is useful for studying repercussions on bulbar-medullary junction and for detecting signs of spinal cord injury [10]. The treatment of odentoideum bone depends on the clinical presentation. Only symptomatic patients should benefit from surgical management which aims to stabilize and to reduce lordosis by arthrodesis and osteosynthesis most often by posterior approach. In asymptomatic participants, the prophylactic surgical indication is discussed according to the data of the dynamic plates. However, the majority of authors advocate regular clinical or radiological monitoring. In these cases, participants must be warned of the risk of complications of this condition to avoid any risk situation [9].
Conclusion
Odontoideum bone is a rare, potentially serious, and life-threatening malformation. It is essential to know this condition and not to consider it as a normal variant. It is most often asymptomatic, but symptoms could occur in any time following a benign trauma. The diagnosis is based on CT, which allows the study of the malformation and shows an associated C1C2 dislocation. As for MRI, its role is to evaluate the effect on the contents of the spinal canal and thus to detect the signs of spinal cord suffering. Surgical treatment is effective, based on a posterior arthrodesis. Rarely, a surgical reduction of the dislocation is not obtained by pre-operative traction and has to be carried out by the tanery or posterior approachs. The prognosis depends essentially on the precocity of the management and several authors recommend preventive surgery in case of instability.
Clinical Message
Odontoideum bone is a rare malformation that can decompensate at any age and involve functional and vital prognosis. The diagnosis is based on CT, which allows the study of the malformation and shows an associated C1C2 dislocation. As for MRI, its role is to evaluate the effect on the contents of the spinal canal and thus to detect the signs of spinal pain. Thus, several authors advocate preventive management in case of instability if ever this malformation has been diagnosed. Surgical treatment is effective, based on a posterior arthrodesis. Rarely, a surgical reduction of the dislocation not obtained by pre-operative traction is carried out by the tannery or posterior way. The prognosis depends essentially on the precocity of the management and several authors recommend preventive surgery in case of instability.
References
1. Sankar WN, Wills BP, Dormans JP, Drummond DS. Os odontoideum revisited: The case for a multifactorial etiology. Spine (Phila Pa 1976) 2006; 31(9):979-984.1. Sankar WN, Wills BP, Dormans JP, Drummond DS. Os odontoideum revisited: The case for a multifactorial etiology. Spine (Phila Pa 1976) 2006; 31(9):979-984.
2. Choit RL, Jamieson DH, Reilly CW. Os odontoideum: A significant radiographic finding. Pediatr Radiol 2005; 35(8):803-807.
3. White IK, Mansfield KJ, Fulkerson DH. Sequential imaging demonstrating osodentoideum formation after a fracture through the apical odontoid epiphysis: Case report and review of literature. Child Nerv Syst 2013; 29(11):2111-2115.
4. Dai L, Yuan W, Ni B, Jia L. Os odontoideum: Etiology, diagnosis, and management. Surg Neurol 2000; 53(2):106-108.
5. Satte A, Ech-Cherif El Kettani N, El Quessar A, El Hassani MR, Chakir N, Boukhrissi N, et al. Os odontoideum: Clinical and radiological aspects. Rev Neurol (Paris) 2008; 164(2):177-180.
6. Kirlew KA, Hathout GM, Reiter SD, Gold RH. Os odontoideum in identical twins: Perspectives on etiology. Skeletal Radiol 1993; 22(7):525-527.
7. Zygourakis CC, Cahill KS, Proctor MR, et al. Delayed development of osodontoideum after traumatic cervical injury: Support for a vascular etiology. J Neurosurg Pediatr 2011; 7:201-220.
8. Wada E, Matsuoka T, Kawai H. Os odontoideum as a consequence of a posttraumatic displaced ossiculum terminale. A case report. J Bone Joint Surg Am 2009; 91(7):1750-1754.
9. Laghmari M, El Hymer W, Aniba K, et al. Os odontoideum: A propos d’un cas et revue de la littérature. Pan Afr Med J 2012; 13:44.
10. Diebener J, Sundaram M. Radiologic case study. Os odontoideum. Orthopedics 1994; 17(11):1083-10835.
11. Robson KA. Os odontoideum: Rare cervical lesion. West J Emerg Med 2011; 12(4):520-522.
 |
 |
 |
 |
 |
| Dr. Lassaad Hassini | Dr. Mohamed Ali Khalifa | Dr. Alaya Zeineb | Dr. Osman Walid | Dr. Mtaoumi Mourad |
| How to Cite This Article: Hassini L, Khalifa MA, Alaya Z, Ayeche MLB, Osman W, Mtaoumi M. Odontoideum Bone Revealed by c1-c2 Dislocation of the Cervical Spine during a Diving Accident. Journal of Orthopaedic Case Reports 2017 Jul-Aug: 7(4): 3-5 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




