[box type=”bio”] What to Learn from this Article?[/box]
Group B Streptococcal prosthetic knee joint infection is associated with foodborne transmission from the consumption of raw freshwater fish.
Case Report | Volume 7 | Issue 4 | JOCR July – August 2017 | Page 54-57| Gin Way Law, Limin Wijaya, Andrew Hwee Chye Tan DOI: 10.13107/jocr.2250-0685.850
Authors: Gin Way Law[1], Limin Wijaya[1], Andrew Hwee Chye Tan[1]
[1]Department of Orthopaedic Surgery, Singapore General Hospital, Singapore 169608, Singapore.
Address of Correspondence
Dr. Gin Way Law,
Department of Orthopaedic Surgery, Singapore General Hospital, Singapore General Hospital, Outram Road, Singapore 169608, Singapore.
E-mail: gin.law26@gmail.com
Abstract
Introduction: Group B Streptococcal (GBS) prosthetic joint infections (PJI) are rare, accounting for only 4.6-6% of primary and revision total knee replacements (TKRs). In 2015, there was an outbreak of GBS infections in Singapore with an association confirmed between consumption of Chinese-style raw fish dishes (snakehead fish, Asian bighead carp) and GBS infection, Type III GBS ST283 strain, affecting more than 200 patients in Singapore. This outbreak is the largest of its kind in the world and also the first time that foodborne transmission of GBS has been proven. We present the first reported case in the literature of a confirmed PJI in a TKR related to foodborne transmission of GBS through consumption of raw fish (Snakehead fish).
Case Report: Our patient is a 66-year-old Chinese female admitted with a 24-h history of acute right knee pain and swelling with associated fever in the context of consuming raw fish porridge 3 days before the onset of her symptoms. She had a TKR performed in the same knee 7 years before this presentation. Her GBS PJI was confirmed on both blood and intraoperative tissue/fluid cultures during the outbreak of GBS infections in Singapore. This was managed with debridement, polyethylene liner change, retention of metal prosthesis, and culture-directed antibiotics with good outcomes.
Conclusion: Snakehead fish is a popular dish in the Asian community as a traditional remedy to promote wound healing after surgery. Our paper highlights the link between raw fish consumption and invasive GBS causing PJIs. This can occur in healthy adults, even in the absence of gastrointestinal symptoms, despite being a foodborne transmission. Our paper also highlights that GBS PJIs can be managed with debridement, antibiotic therapy, and implant retention with good outcomes in the setting of acute hematogenous infection. We recommend the inclusion of raw fish consumption on history taking in the workup of suspected PJIs and counseling patients preoperatively on the risk of GBS PJIs with the consumption of raw fish dishes (snakehead fish and Asian bighead carp) to mitigate unnecessary PJI risk.
Keywords: Group B Streptococcus, Prosthetic Joint Infection, Raw Fish, Foodborne Transmission, DAIR.
Introduction
Prosthetic joint infections (PJI) are associated with significant morbidity and require prompt diagnosis and early management. Staphylococcus aureus and Staphylococcus epidermidis account for the majority (65%) of PJIs, whereas streptococcal infections are responsible for 14.5-21% of all PJIs. Group B streptococcal (GBS) infections are rare and are responsible for infection in 4.6-6% of primary and revision total knee replacements (TKRs) [1].
In 2015, there was an outbreak of GBS infections in Singapore with an association confirmed between consumption of Chinese-style raw fish dishes and GBS infection, Type III GBS ST283 strain, affecting more than 200 patients in Singapore [2, 3]. The dishes were prepared using snakehead fish and Asian bighead carp. This outbreak is the largest of its kind in the world and also the first time that foodborne transmission of GBS has been proven. While most strains of GBS that affect humans tend to only cause infections in newborns or people with weak immune systems, this particularly aggressive strain of GBS has been seen to cause severe infections even in healthy people [4].
Earlier studies have suggested that penicillin-susceptible streptococcal PJIs managed with debridement, antibiotic therapy, and implant retention (DAIR) have better outcomes compared to PJIs due to other organisms. This in combination with other predictors of good outcomes such as acute hematogenous or early post-operative PJIs (<3 weeks), stable implants, short duration of symptoms before debridement, and absence of sinus tracts, makes DAIR an attractive alternative in infection eradication compared to the more aggressive traditional two-stage reimplantation procedure with its associated increased surgical and perioperative risk.
We present the first reported case of GBS PJI linked to the GBS outbreak in Singapore, treated with DAIR.
Case Report
A 66-year-old female was admitted to a tertiary hospital with a 24-h history of acute right knee pain and swelling with associated fever, chills, and rigors. She had a right TKR performed 7 years before this presentation and was on fenofibrate for hypercholesterolemia. She consumed raw fish (snakehead fish) porridge at the local market 3 days before the onset of her symptoms. There was no other history to suggest any primary hematogenous sources of infection.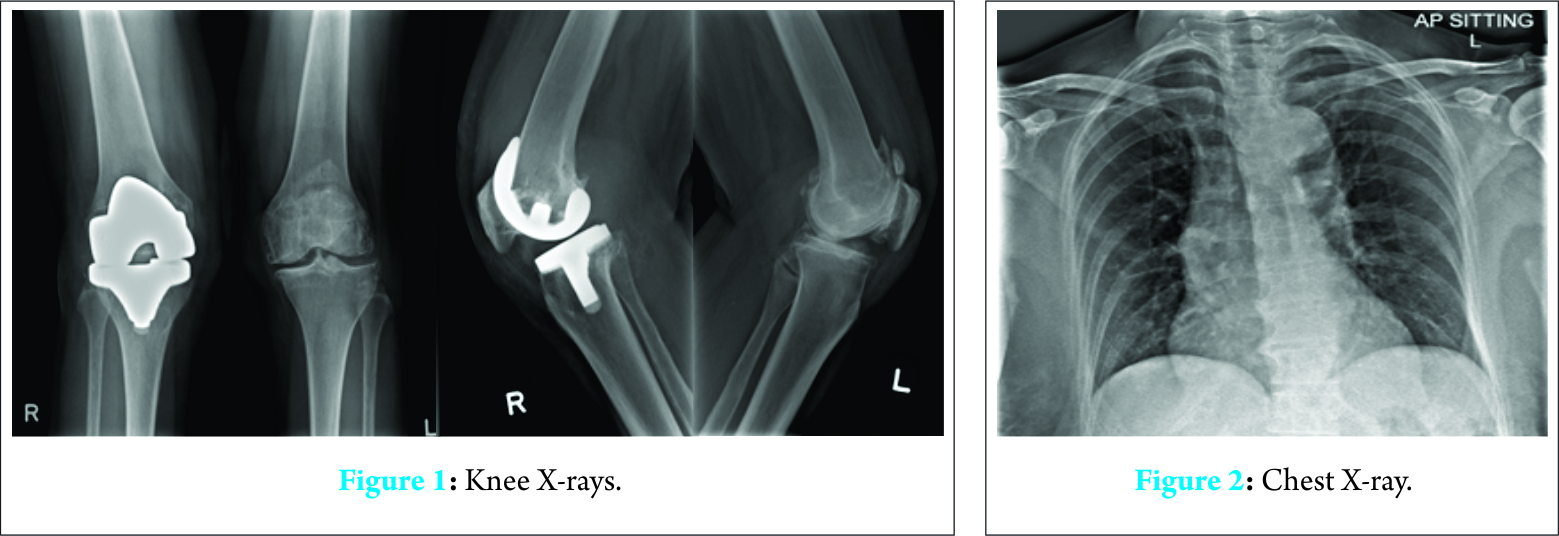
On examination, she was toxic-looking, febrile but hemodynamically stable. Her right knee was hot, tender, and grossly swollen with a markedly limited range of motion secondary to pain. She was otherwise neurovascularly intact in her right lower limb. Cardiorespiratory and abdominal examinations were normal.
Investigations
Inflammatory markers were markedly raised with C-reactive protein (CRP) 333 mg/L, white cell count 16.26 × 109/L and erythrocyte sedimentation rate 84 mm/h. Other blood tests were within normal range. Her right knee X-ray showed no features of prosthesis loosening or periprosthetic fractures (Fig. 1). Chest X-ray showed no evidence of consolidation in the lungs (Fig. 2).
Treatment
Our patient was diagnosed with an infected prosthetic right knee, and the decision was made for an arthrotomy, washout, and change of polyliner. This was performed on the day of her presentation and empirical antibiotics were commenced. The choice of a combination of cefepime, vancomycin, and rifampicin was made in consultation with our infectious diseases physician.
Intraoperatively, she had large amounts of pus in her right knee joint. Her femoral and tibial metal implants were well-fixed. No sinus tracts were found. The GBS PJI of her right TKR was confirmed on both intraoperative fluid and tissue cultures. Blood cultures were also positive for GBS.
She was managed with intravenous (IV) benzylpenicillin thereafter based on antibiotic sensitivities. Her drain was removed on post-operative day 4.
During her admission, she had deranged liver function tests (LFTs). Initial ultrasound showed two 1 cm faint hypoechoic lesions in her right hepatic lobe suspicious of evolving hepatic abscesses given recent bacteremia. This was managed with antibiotics alone and subsequent computed tomography scan showed complete resolution of the suspected liver abscesses. Her LFTs normalized afterward.
Outcome and follow-up
She improved postoperatively but had intermittent low-grade fever despite downtrending inflammatory markers. She was able to mobilize independently with a walking stick on discharge and her right knee active range of motion was 0-120°.
She was given 6 weeks of high-dose IV benzylpenicillin and was followed up by both orthopedics and infectious disease teams. Her antibiotic regime was switched to oral clindamycin at 6 weeks postsurgery in view of its superior bioavailability profile over oral penicillin.
Table 1 shows her inflammatory markers trend from the time of her presentation, postoperatively on day 4, on discharge at 4 weeks and subsequently on follow-up at 6 weeks, 3 months, 6 months, 10 months, 1.5 years, and 2 years, respectively. Her inflammatory markers showed a significant drop postoperatively and continued on a downward trend on subsequent follow-ups. Her CRP and WBC count normalized after 3 months.
At 6 weeks, she had complete resolution of her fever and was mobilizing independently without walking aids. She continued to do well thereafter.
Our patient was planned for long-term antibiotics suppression with oral clindamycin. However, after 1.5 years of clindamycin, she was keen for a trial of cessation of antibiotics suppression therapy. Clindamycin was stopped after discussion with her infectious disease physician.
She remained clinically well 6-month postcessation of antibiotics.
Discussion
There were 360 cases of GBS infections with 2 fatalities in Singapore in 2015 compared to an average of 150 cases per year in the previous 4 years [4, 5]. Over 200 confirmed patients were affected by the GBS infection, Type III GBS ST283 strain due to the consumption of Chinese-style raw fish dishes [2, 3]. While most strains of GBS that affect humans tend to only cause infections in newborns or people with weak immune systems, this particularly aggressive strain of GBS has been seen to cause severe infections even in healthy people [4].
A joint investigation conducted by the National Environmental Agency, the Agri-Food and Veterinary Authority of Singapore and the Ministry of Health during the outbreak revealed detection of GBS in raw fish samples (snakehead fish and Asian Bighead Carp) during field investigations at various locations including sources and distribution chains [5, 6]. The sale of raw fish dishes containing snakehead fish and Asian bighead carp was hence suspended on July 24, 2015 (during epidemiologic week 29) [5, 6]. Our patient consumed raw fish (snakehead fish) porridge at the local market before the suspension on the sale of this fish on July 13, 2015, from one of these sources involved in the investigation and developed acute right knee pain and swelling with associated fever, chills, and rigors 2 days after.
Her operation for an arthrotomy, washout and change of polyliner was performed on July 16, 2015, within 24 h of the onset of her symptoms and her GBS PJI was subsequently confirmed on both blood and intraoperative tissue/fluid cultures.
PJI is an infrequent complication of total joint arthroplasty, occurring in 0-15% of cases [7]. A common approach to the treatment of PJIs is a two-stage revision, with success rates ranging from 85% to 100% for infection eradication. However, this is not without drawbacks. A two-stage exchange requiring two surgical procedures as a minimum may lead to multiple surgical interventions, prolonged antibiotic exposure, protracted immobility, and hospitalization stays with attendant potential complications and medical expenses [8]. The removal of a well-seated cemented prosthesis may also result in degradation of bone stock and perioperative fractures [9].
Our case demonstrated that GBS PJIs can be effectively treated with a combination of antibiotic therapy, exchange of polyethylene liner and debridement with metal prostheses retention. This is in congruence with several earlier studies.
Zimmerli et al. and Cui et al. both supported the treatment of acute hematogenous infections with debridement and prosthesis retention in the presence of a previously well-functioning joint replacement, stable implants with good soft tissue condition, and the availability of antimicrobial agents with specific activity against the respective biofilm microorganisms [10, 11].
Meehan et al. in their study of the outcomes of penicillin-susceptible streptococcal PJIs also suggested that prompt debridement with retention of prostheses in PJIs with culture-proven streptococcal organisms to be a reasonable treatment alternative in acute PJIs. PJIs due to streptococci in their study had better outcomes than PJIs due to other organisms when treated with debridement and retention of prosthesis, consistent with earlier studies [8, 12, 13].
Meehan et al. highlighted several criteria predicting favorable outcomes, including short duration of symptoms before debridement (<5 days), penicillin-susceptible streptococcal causative organisms, well-fixed prostheses, interval of at least 1 month after prosthesis implantation, and prolonged duration of IV antimicrobial therapy [8]. Burger et al. suggested similar criteria predicting favorable outcomes but also included the absence of sinus tracts or prolonged post-operative drainage [12]. These are in keeping with our patient in this case report.
Open debridement with exchange of the polyethylene liner facilitates a more thorough washout, especially in the posterior knee joint. In 2013, Lora-Tamayo et al. in their retrospective, multicenter, observational study of S. aureus PJI cases managed with DAIR (2003-2010) showed that the exchange of removable components of the prosthesis was an independent predictor of success. By exchanging the polyethylene component of the prosthesis, the risk of failure was reduced by 33% [14]. This is consistent with Byren et al.’s study in 2009 of infected arthroplasties treated with DAIR, where modular prosthesis components were exchanged when an open debridement was performed. The subgroup of patients in this study who underwent arthroscopic washout without exchange of the modular components was associated with a significant risk of treatment failure [9].
There are several unique features in our case report. In addition to being the first reported case in the literature of a confirmed PJI related to foodborne transmission of GBS, the link between raw fish consumption and invasive GBS infection even in healthy adults is an interesting one. This is especially so, given the absence of gastrointestinal symptoms in our case, despite being a foodborne transmission.
The snakehead fish dish, in the Asian community, is a popular dish as a traditional remedy to promote wound healing after surgery, in postpartum mothers and after injury [15]. We feel that this is relevant in the counseling of patients who are undergoing joint replacement surgery as they may be more inclined to consume this dish in the post-operative setting to boost recovery. The risk of developing PJI, among other infections, should be highlighted with the consumption of raw fish (snakehead fish) given its significant associated morbidity and potentially devastating consequences. This risk, in our opinion, outweighs its medicinal benefits of wound healing and can be mitigated or eliminated completely with appropriate counseling.
Conclusion
We recommend the inclusion of raw fish consumption on history taking in the workup of suspected PJI. We support the use of debridement with polyethylene liner change together with culture-directed antimicrobial therapy as the treatment of choice in GBS-infected TKRs if patients present acutely with symptoms and signs of PJI in the absence of prosthesis loosening or sinus tract formation, failing which, removal of implants may then have to be considered.
Clinical Message
It is important to counsel patients, especially those from the Asian community, who are undergoing joint replacement surgery on the risk of developing joint infection with raw fish consumption (snakehead fish) given that they may be more inclined to consume this dish in the post-operative setting to boost recovery. We recommend the inclusion of raw fish consumption on history taking in the workup of suspected PJI. This can happen in healthy adults, even with the absence of gastrointestinal symptoms, despite being a food-borne transmission. We support the use of debridement with polyethylene liner change together with culture-directed antimicrobial therapy as the treatment of choice in GBS-infected TKRs if patients present acutely with symptoms and signs of PJI in the absence of prosthesis loosening or sinus tract formation, failing which, removal of implants may then have to be considered.
References
1. Mortazavi SM, Schwartzenberger J, Austin MS, Purtill JJ, Parvizi J. Revision total knee arthroplasty infection: Incidence and predictors. Clin Orthop Relat Res 2010;468(8):2052-2059.1. Mortazavi SM, Schwartzenberger J, Austin MS, Purtill JJ, Parvizi J. Revision total knee arthroplasty infection: Incidence and predictors. Clin Orthop Relat Res 2010;468(8):2052-2059.
2. Kalimuddin S, Chen S, Lim C, Koh T, Tan T, Kam M, et al. Epidemic of severe Streptococcus agalactiae sequence Type 283 infections in Singapore associated with the consumption of raw freshwater fish: A detailed analysis of clinical, epidemiological, and bacterial sequencing data. Clin Infect Dis 2017;64 Suppl 2:S145-S152.
3. Tan K, Wijaya L, Chiew HJ, Sitoh YY, Shafi H, Chen RC, et al. Diffusion-weighted MRI abnormalities in an outbreak of Streptococcus agalactiae serotype III, multilocus sequence Type 283 meningitis. J Magn Reson Imaging 2017;45(2):507-514.
4. Osada J. Recent GBS Outbreak ‘Biggest in the World’. The Straits Times, Singapore Press Holdings. Available from: http://www.straitstimes.com/singapore/recent-gbs-outbreak-biggest-in-the-world. [Last accessed on 2017 Sep 11].
5. Ministry of Health, Singapore. Update on Investigation into Group B Streptococcus cases. Press Releases, News Highlights, 24 July 2015. Available from: https://www.moh.gov.sg/content/moh_web/home/pressRoom/pressRoomItemRelease/2015/update-on-investigation-into-group-b-streptococcus-cases.html [Last accessed on 2017 Sep 11].
6. Rajendram P, Kyaw WM, Leo YS, Ho H, Chen WK, Lin R, et al. Group B Streptococcus sequence Type 283 disease linked to consumption of raw fish, Singapore. Emerg Infect Dis 2016;22(11):1974-1977.
7. Steckelberg JM, Osmon DR. Prosthetic joint infection. In: Bisno A, Waldvogel F, editors. Infections Associated with Indwelling Devices. Washington, DC: American Society for Microbiology. 2000. p. 173-209.
8. Meehan AM, Osmon DR, Duffy MC, Hanssen AD, Keating MR. Outcome of penicillin-susceptible streptococcal prosthetic joint infection treated with debridement and retention of the prosthesis. Clin Infect Dis 2003;36(7):845-849.
9. Byren I, Bejon P, Atkins B, Angus B, Masters S, McLardy-Smith P, et al. One hundred and twelve infected arthroplasties treated with ‘DAIR’ (Debridement, antibiotics and implant retention): Antibiotic duration and outcome. J Antimicrob Chemother 2009;63(6):1264-1271.
10. Zimmerli W, Trampuz A, Ochsner PE. Current concepts: Prosthetic joint infections. N Engl J Med 2004;351:1645-1654.
11. Cui Q, Mihalko WM, Shields JS, Ries M, Saleh KJ. Antibiotic-impregnated cement spacers for the treatment of infection associated with total hip or knee arthroplasty. J Bone Joint Surg Am 2007;89(4):871-882.
12. Burger RR, Basch T, Hopson CN. Implant salvage in the infected total knee arthroplasty. Clin Orthop 1991;273:105-112.
13. Schoifet S, Morrey BF. Treatment of infection after total knee arthroplasty by debridement with retention of the components. J Bone Joint Surg Am 1990;72(9):1383-1390.
14. Lora-Tamayo J, Murillo O, Iribarren J, Soriano A, Sanchez-Somolinos M, Baraia-Etxaburu J, et al. A large multicentre study of methicillin-susceptible and methicillin-resistant Staphylococcus aureus prosthetic joint infections managed with implant retention. Clin Infect Dis 2012;56(2):182-194.
15. Wahab SA, Kadir AA, Hussain NN, Omar J, Yunus R, Baie S, et al. The effect of Channa striatus (Haruan) Extract on pain and wound healing of post-lower segment caesarean section women. Evid Based Complement Alternat Med 2015;2015:1-6.
 |
 |
 |
| Dr. Law Gin Way | Dr. Limin Wijaya | Dr. Andrew Hwee Chye Tan |
| How to Cite This Article: Law GW, Lim FMT, Wijaya L, Tan AHC. Group B Streptococcal Prosthetic Knee Joint Infection Linked to the Consumption of Raw Fish. Journal of Orthopaedic Case Reports 2017 Jul-Aug;7(4):54-57. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




