[box type=”bio”] Learning Points for this Article: [/box]
Cerebrotendinous xanthomatosis patient with totally displaced femoral neck fracture could be treated by cementless bipolar hemiarthroplasty with satisfactory outcomes.
Case Report | Volume 7 | Issue 5 | JOCR September – October 2017 | Page 54-58| Witchuree Wejjakul, Swist Chatmaitri, Thongek Wattanarojanaporn, Anuwat Pongkunakorn, Chupong Ittiwut, Vorasuk Shotelersuk. DOI: 10.13107/jocr.2250-0685.894
Authors: Witchuree Wejjakul [1], Swist Chatmaitri [1], Thongek Wattanarojanaporn [1], Anuwat Pongkunakorn [1], Chupong Ittiwut [2], Vorasuk Shotelersuk [2]
[1] Department of Orthopaedic Surgery, Lampang Hospital and Medical Education Center, Lampang, Thailand, 2 Center of Excellence for Medical Genetics, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand.
Address of Correspondence
Dr. Anuwat Pongkunakorn,
Department of Orthopaedic Surgery, Lampang Hospital and Medical Education Center, 280 Paholyothin Road, Mueang, Lampang 52000, Thailand.
E-mail: dranuwat@hotmail.com
Abstract
Introduction: Cerebrotendinous xanthomatosis (CTX) is a rare autosomal recessive lipid storage disease caused by mutations of the CYP27A1 gene and deficiency of the sterol-27-hydroxylase enzyme in bile acid biosynthesis. It is characterized by the accumulation of cholestanol and bile alcohols in plasma, the formation of xanthomatous lesions in various tissues, and organ degeneration. This disorder is also associated with osteoporosis and increased risk of fracture. To date, only two CTX patients with femoral neck fractures have been reported. Neither was treated by arthroplasties, and the operative outcomes are lacking.
Case Report: We report the case of a 46-year-old Thai female who presented with consecutive bilateral femoral neck fractures following minor trauma within a 3-year period and received cementless bipolar hemiarthroplasties. Her phenotypic expression included Achilles tendon masses, childhood-onset cataracts, intellectual disability, and cerebellar ataxia. A brain computed tomography showed non-enhancing hypodense lesions in the bilateral cerebellar hemispheres with mild brain atrophy. Histopathology from an Achilles tendon biopsy revealed tendinous xanthoma and molecular analysis confirmed a homozygous nonsense mutation, c.1072C>T (p.Gln358Ter), in exon 6 of the CYP27A1 gene. The intra-operative crack of a calcar femorale was a major complication during both prosthetic insertion surgeries and warranted cerclage wiring. At the 7-month follow-up of the right hip and the 41-month follow-up of the left hip, postoperative radiographs showed well-fixed and well-aligned prostheses. Independent household ambulation could be resumed with Harris hip scores of 81 points equally.
Conclusion: CTX is associated with osteoporosis, and middle-aged patients could present with femoral neck fracture following minor trauma. Cementless bipolar hemiarthroplasty for a totally displaced fracture is justified for a patient who has cognitive impairment. Intra-operative fracture is a major complication during prosthetic insertion and warrants cerclage wiring to achieve predictable bone healing and a satisfactory result.
Keywords: Cerebrotendinous xanthomatosis, femoral neck fracture, hip arthroplasty.
Introduction
Cerebrotendinous xanthomatosis (CTX) is a rare inborn error of lipid metabolism, inherited in an autosomal recessive pattern. The estimated incidence ranges from 1:134,970 to 1:461,358 in Europeans, 1:71,677 to 1:148,914 in Americans, and 1:64,267 to 1:64,712 in East Asians [1]. It is caused by mutations of the CYP27A1 gene leading to an absence of the sterol 27-hydroxylase enzyme with a bile acid synthesis defect and cholestanol accumulation in serum and tissues in multiple organs, called xanthoma [2]. The clinical manifestation is typically characterized by bilateral cataracts and diarrhea in childhood and progressive neurological dysfunction and tendon xanthoma in early adulthood [3]. Some investigators have described the association between CTX and osteoporosis that causes a higher risk of fracture after low-energy trauma [4]. Their hypotheses involved Vitamin D deficiency and intestinal calcium malabsorption. To date,<20 patients with CTX who suffered fragility fractures have been reported [4, 5]. Among these, only two patients with femoral neck fractures have been studied, and the operative outcomes with this particular disease are lacking. Here, we present a case of a CTX patient who sustained consecutive bilateral femoral neck fractures, as well as some reviews of the latest literatures.
Case Report
A single 46-year-old Thai woman presented with acute right hip pain after falling onto the ground and could not bear weight. Her underlying diseases were hypertension and mild intellectual disability (IQ=60). At the age of ten, she developed bilateral cataracts and underwent bilateral intraocular lens replacement at the age of about 20. Thereafter, a painless mass gradually developed at the medial side of the left foot and both Achilles tendons became enlarged. At the age of 43, she sustained a left femoral neck fracture owing to a fall in her home and underwent hip hemiarthroplasty (Fig. 1a and b). Her ambulatory status was household independence. A physical examination revealed a thin woman (height 153 cm, weight 38 kg) with her right lower limb in the external rotation position. The left posterior tibial tendon insertion and both Achilles tendons were enlarged in irregular shapes (Fig. 2 a-c). Pes cavus in both feet and camptodactyly of her left little finger were observed. The hip radiographs showed a complete, totally displaced, transcervical fracture of the right femur, Garden classification Type 4 (Fig. 3). The proximal femur appearance was categorized as Dorr Type B. Retention of the well-fixed cementless bipolar prosthesis in the left hip was found. Other bone-surveying radiographs of spine, pelvis, and femurs revealed generalized osteopenia. She underwent hip hemiarthroplasty using a posterolateral approach and a cementless bipolar prosthesis (Avenir Muller stem, Zimmer, Switzerland). There was an accidental crack of the calcar femorale during the stem insertion. A loop of cerclage wiring was then added to prevent fracture propagation. The posterior capsule and short external rotators were repaired. The operative record of the left hip hemiarthroplasty also noted a calcar femorale fracture during the prosthesis insertion warranting cerclage wiring. Cementless bipolar prosthesis (Modular Taperloc stem, Biomet, USA) had been implanted through a posterolateral approach.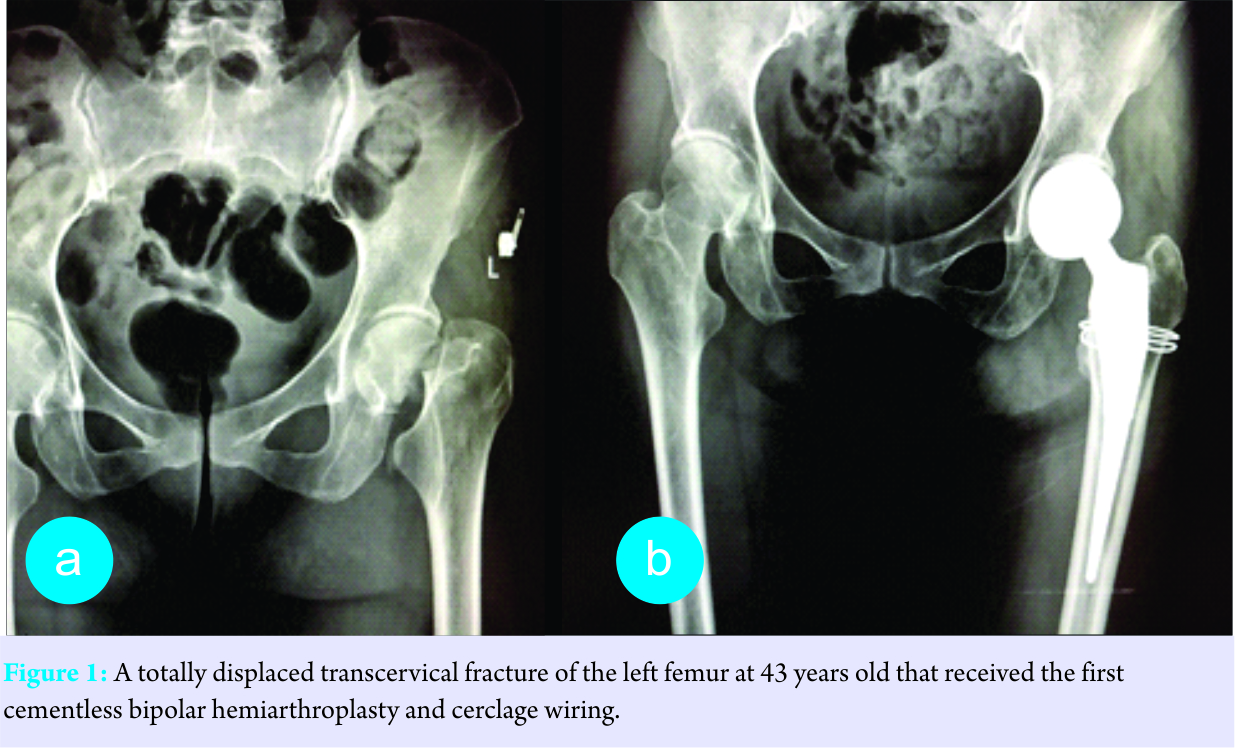
Since these clinical findings were largely in line with CTX, investigations for a definitive diagnosis were undertaken with patient consent. An Achilles tendon biopsy was performed, and histopathology confirmed tendinous xanthoma, characterized by lipid crystal clefts surrounded by foamy histiocytes and multinucleated giant cells. Electrocardiography and a chest radiograph were unremarkable. Serum cholesterol, alkaline phosphatase, calcium, phosphorus, and magnesium levels were normal. Testing for serum cholestanol level was not available in our laboratory. Neurological evaluation found good motor function and mild cerebellar ataxia. A brain computed tomography (CT) showed non-enhancing hypodense lesions in both cerebellar hemispheres, with mild cerebral and cerebellar atrophy (Fig. 4).
Mutation analysis in the CYP27A1 gene was investigated by extraction of the genomic DNA from peripheral blood leukocytes and sent for singleton whole-exome sequencing analysis. The sequencing libraries were enriched by SureSelect Human All Exon V5 kits and sequenced using IlluminaHiSeq 4000 Sequencer. The data were mapped to the human GRCh37/hg19 reference sequence using CASAVA v1.7 (Illumina) followed by variant calling with SAM tools and annotated by ANNOVAR to generate gene-based annotation. A homozygous c.1072C>T (p.Gln358Ter, rs533885672) stop-codon mutation in exon 6 of the CYP27A1 (NM_000784.3) was identified in the patient. The family pedigree was plotted, and no consanguinity was found. Parental blood samples were not available.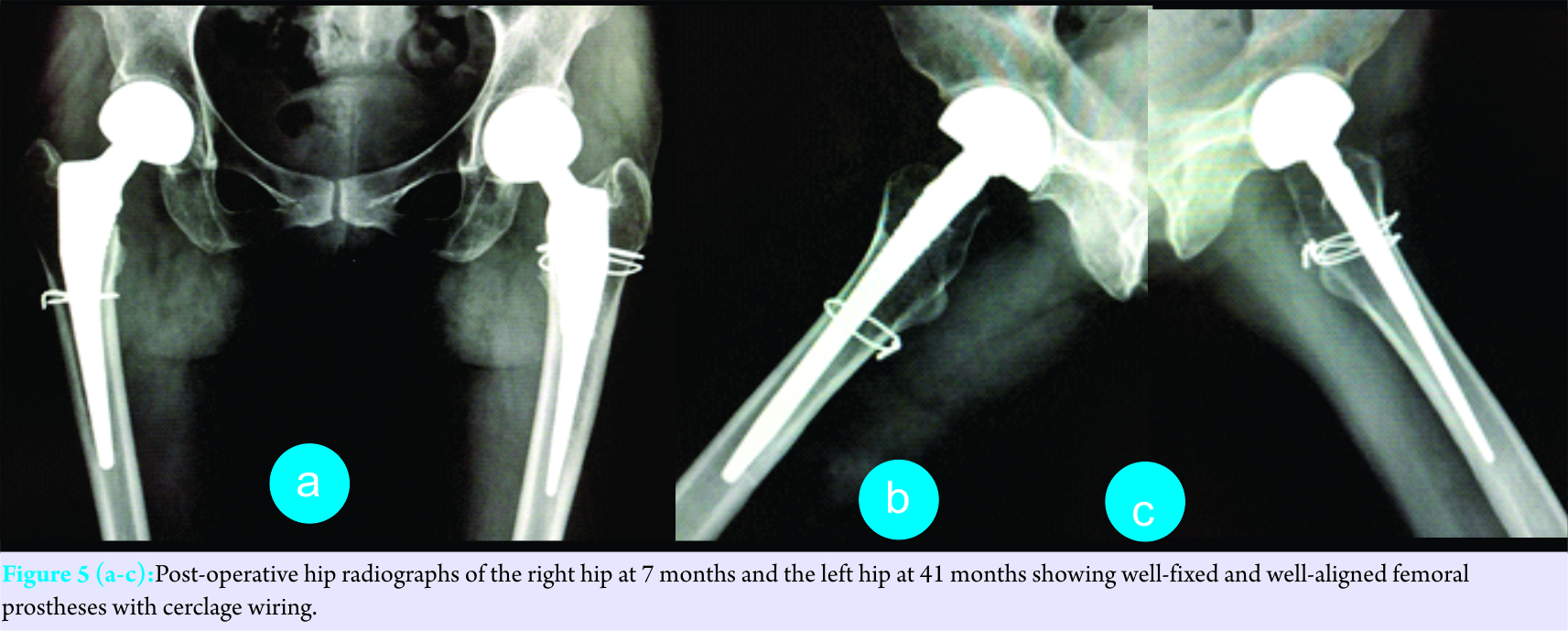
She was prescribed oral calcium carbonate with Vitamin D2 for osteoporotic prophylaxis and allowed partial weight bearing for 6 weeks. The hip radiographs at the latest follow-up (post-operative 7 and 41 months for right and left hips, respectively) showed well-fixed and well-aligned femoral prostheses (Fig. 5a-c).The right leg was found to be 5 mm shorter. A CT scan of both hips and femurs demonstrated 12° and 15° anteversion of right and left femoral stems, respectively. The native acetabular anteversion was 23°. She occasionally had slight pain in both hips but no compromise in activity. She could stand without support and walk with a slight limp for 10–15 minutes. She was capable of going up or down stairs with handrails. Both hip joints had a full range of movement with Harris hip scores of 81 points equally.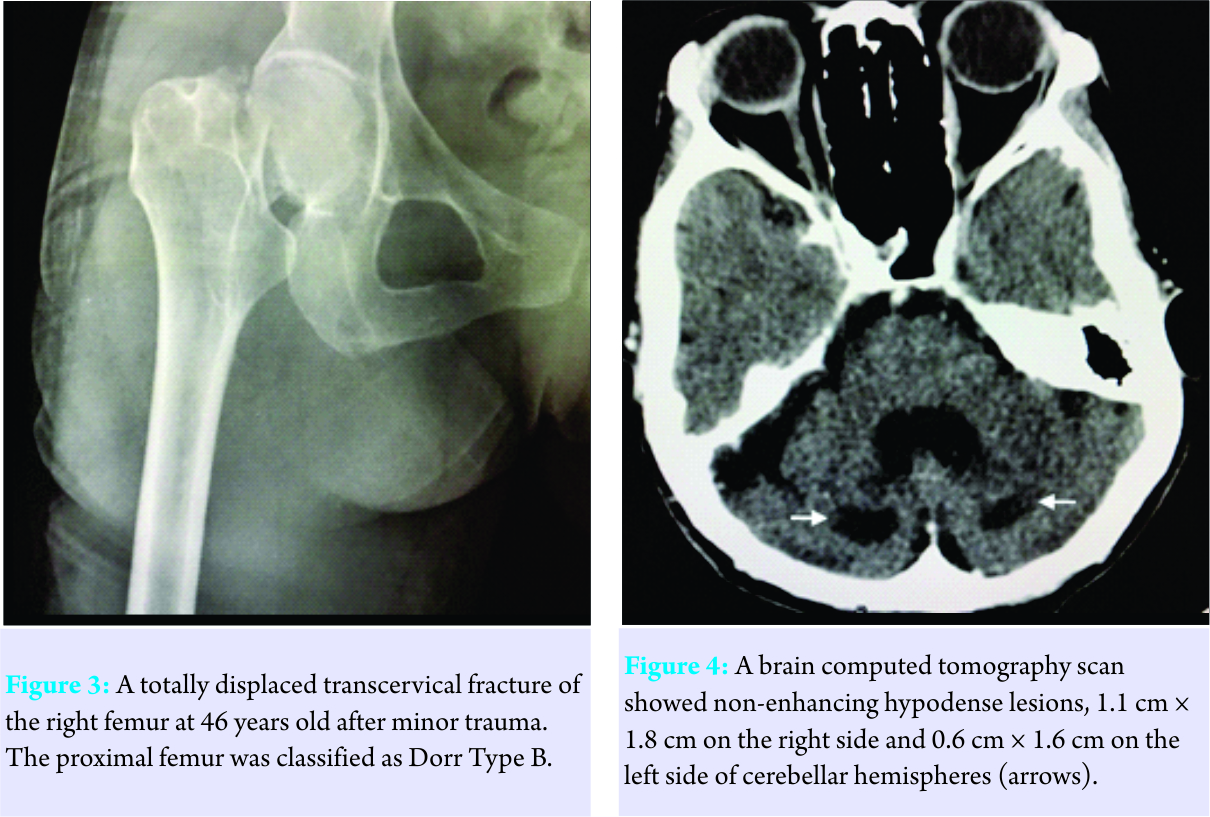
Discussion
CTX is a rare autosomal recessive disorder caused by mutations of the CYP27A1 gene, located on 2q35 (chr2: 219646472-219680016, GRCh37/hg19 assembly). This gene provides instructions in producing sterol 27-hydroxylase, a key enzyme that oxidizes cholesterol to 27-hydroxycholesterol (27-OHC), which is subsequently hydroxylated to be chenodeoxycholic acid (CDCA). Decreased CDCA leads to a compensatory increased activity of cholesterol 7-alpha-hydroxylase and a marked accumulation of 7alpha-hydroxy-4-cholesten-3-one, a bile acid precursor. Further efficient conversion of this precursor into cholestanol and bile alcohols which accumulate in plasma and tissues results in organ degeneration which worsens over time unless treated. The main systemic manifestations are chronic diarrhea, juvenile cataract, tendon xanthoma, and neurological dysfunction. Tendinous xanthoma appears in the second or third decade of life and is most often found in the Achilles tendon [6]. Neurological dysfunction includes spastic paraparesis, cerebellar ataxia, cognitive impairment, psychiatric disturbances, peripheral neuropathy, epilepsy, and parkinsonism. The biochemical abnormalities include high plasma and tissue concentration of cholestanol and decreased levels of CDCA and 27-OHC. Definitive diagnosis is obtained by molecular analysis of the CYP27A1 gene [6]. CTX is an underdiagnosed disorder, and early diagnosis is often difficult. More than 300 patients with CTX have been reported worldwide without a clear genotype-phenotype correlation [7]. The estimated prevalence is <5:100,000 worldwide and approximately 1:50,000 in Caucasians [8]. The predicted incidence of CTX ranges from 1:263,222 to 1:468,624 in Africans and1:36,072 to 1:75,601 in South Asians [1]. Interestingly, this case is the first Thai patient diagnosed as CTX which could be owing to its rarity or to being underreported. Molecular analysis confirmed a homozygous c.1072C>T stop-codon mutation in exon 6 of the CYP27A1 gene which leads to 174-amino acids premature truncation of the CYP27A1 protein. Although this variant was found in heterozygous state in four East Asians in the Exome Aggregation Consortium database of 121,358 alleles, no individuals have been found to be homozygous for this variant (rs533885672). In addition, this mutation has not been reported in any patients with CTX and is absent in our 719 Thai in-house Exome database. Osteoporosis and increased bone fractures have been reported to be associated with CTX. Berginer et al. observed a high frequency of fractures in nine of 15 CTX patients [4]. Decreased bone mineral densitometry (BMD) and histological abnormality in bone biopsies confirmed osteoporosis. BMD reduction was also described in six of eight patients by Federico et al. and 20 of 30 patients by Mignarri et al.[5,6]. However, the mechanism underlying in alteration of bone metabolism is still unclear, and the severity of osteoporosis does not correlate with biochemical parameters [2]. Berginer et al. found significantly low levels of serum 25-hydroxyvitamin D (25-OHD) and 24,25(OH)2D, but a normal metabolically active 1,25(OH)2D level in their patients which might relate to a defective side-chain hydroxylation of Vitamin D [4]. An alternative hypothesis was described by Federico et al. who found normal levels of Vitamin D metabolites in their patients but decreased intestinal radiocalcium absorption. Skeletal demineralization may correlate with impairment of intestinal calcium and Vitamin D absorption owing to changes in the quantity and composition of bile acids [5]. From our extensive reviews, there are four articles reported a total of 17 CTX patients with bone fractures. These included one vertebral [5],one ulnar [9] and unidentified fractures in unpublished six American CTX patients [10]. Another nine patients with 16 fractures were reported by Berginer et al. [4]. Among these, two hip fractures (one cervico-trochanteric and one femoral neck) were treated by internal fixation with nail-plate devices. Postoperatively, both of them had subsequent femoral shaft fractures distal to the plates [4]. Our patient had consecutive bilateral femoral neck fractures with total displacement from minor trauma within a 3-year period. Most surgeons agree that elderly patients with a displaced fracture should receive arthroplasty, but there is no clear consensus in younger patients. Internal fixation is generally recommended in the patients who are mobile, independent, and not cognitively impaired, whereas arthroplasty significantly reduces the re-operation rate [11]. Total hip replacement is indicated in active patients due to better functional score and lower revision rate than hemiarthroplasty. However, higher risk of post-operative dislocation should be aware and possibly preventable using dual mobility cup or anterior surgical approach. For this middle-aged patient with mild cognitive impairment, bipolar hemiarthroplasty could be justified according to her household activity and higher risk of post-operative dislocation. To the best of our knowledge, this is the first case report of bilateral femoral neck fractures in a CTX patient treated by hip arthroplasties. There is no consensus regarding cemented versus cementless fixation for bipolar hemiarthroplasty. A meta-analysis concluded that both fixation methods are comparable [12]. The type of stem can be determined according to the Dorr classification of the proximal femur and cortical thickness on a pre-operative film. Use of cementless stem has been recommended in Dorr Type A and a cemented stem in Dorr Type C femur. For Dorr Type B, both types of stem can be used depending on the patient’s age and bone quality according to femoral cortical thickness index (CTI). A value of ≤0.40 should be a warning sign for osteoporosis [13]. The cemented stem is preferred in osteoporotic bone that initial stability from cementless fixation is questionable or immediate full-weight bearing is expected. The proximal femur of this patient was classified as Dorr Type B, and CTI value was 0.51, so cementless stem was selected. We found intra-operative fractures during both stem insertions and needed cerclage wiring. The fractures healed completely without stem subsidence. Intra-operative fracture is a major complication during cementless hemiarthroplasty with the reported rate of 5.2–10% [14]. Most of the fractures occurred during impaction of the prosthesis or subsequent reduction of the hip. This patient could return to her pre-fracture status of independent household ambulation. She had good hip function with Harris hip scores of 81 points, comparable with the mean scores of 82 points in the previous study [15]. Current recommended treatment for CTX includes replacement therapy and supportive treatment. Bile acid replacement with CDCA or cholic acid can normalize plasma cholestanol and improve non-neurological symptoms in many CTX patients, but only CDCA can improve the neurological symptoms [1]. Providing CDCA exogenously has a negative feedback to reduce the synthesis of bile acid and prevent accumulation of cholestanol, leading to clinical stabilization and improved neurophysiological parameters [1]. CDCA treatment also increases BMD and 25-OHD serum levels, probably due to bile acid restoration with improved intestinal absorption of food-derived Vitamin D [2]. Treatment with Vitamin D combined with CDCA may prevent osteoporotic complications [4]. Nevertheless, CDCA is not available in our country for a patient prescription. Neurological disability in CTX patients may lead to limited sunlight exposure, and dietary Vitamin D intake may play a more relevant role in Vitamin D storage.
Conclusion
CTX is associated with osteoporosis, and middle-aged patients could present with femoral neck fracture following minor trauma. Cementless bipolar hemiarthroplasty for totally displaced fracture is justified for patients who have cognitive impairment and provides satisfactory results. Intraoperative fracture is a major complication during prosthetic insertion and requires cerclage wiring to achieve predictable bone healing. Moreover, we expand the mutational spectrum of CTX to include a homozygous nonsense mutation, c.1072C>T (p.Gln358Ter), in exon 6 of the CYP27A1 gene.
Clinical Message
CTX is a rare autosomal recessive disorder of lipid metabolism that causes accumulation of cholestanol in plasma and tissues. Multiple organ degeneration includes juvenile cataract, tendon xanthoma, and neurological dysfunction. CTX is also associated with osteoporosis, and femoral neck fracture could be presented in middle-aged patients following minor trauma. Totally, displaced fracture in cognitively impaired patients could be treated by cementless bipolar hemiarthroplasty with satisfactory results. Intraoperative fracture is a major complication during prosthetic insertion and warrants cerclage wiring for optimal bone healing.
References
1. Appadurai V, DeBarber A, Chiang PW, Patel SB, Steiner RD, Tyler C, et al. Apparent underdiagnosis of cerebrotendinous xanthomatosis revealed by analysis of ~60,000 human exomes. Mol Genet Metab 2015;116:298-304.
2. Martini G, Mignarri A, Ruvio M, Valenti R, Franci B, Del Puppo M, et al. Long-term bone density evaluation in cerebrotendinous xanthomatosis: Evidence of improvement after chenodeoxycholic acid treatment. Calcif Tissue Int 2013;92:282-6.
3. Yanagihashi M, Kano O, Terashima T, Kawase Y, Hanashiro S, Sawada M, et al. Late-onset spinal form xanthomatosis without brain lesion: A case report. BMC Neurol 2016;16:21.
4. Berginer VM, Shany S, Alkalay D, Berginer J, Dekel S, Salen G, et al. Osteoporosis and increased bone fractures in cerebrotendinous xanthomatosis. Metabolism 1993;42:69-74.
5. Federico A, Dotti MT, Lore F, Nuti R. Cerebrotendinous xanthomatosis: Pathophysiological study on bone metabolism. J Neurol Sci 1993;115:67-70.
6. Mignarri A, Gallus GN, Dotti MT, Federico A. A suspicion index for early diagnosis and treatment of cerebrotendinous xanthomatosis. J Inherit Metab Dis 2014;37:421-9.
7. Nie S, Chen G, Cao X, Zhang Y. Cerebrotendinous xanthomatosis: A comprehensive review of pathogenesis, clinical manifestations, diagnosis, and management. Orphanet J Rare Dis 2014;9:179.
8. Lorincz MT, Rainier S, Thomas D, Fink JK. Cerebrotendinous xanthomatosis: Possible higher prevalence than previously recognized. Arch Neurol 2005;62:1459-63.
9. Agrawal NK, Garg S. Cerebrotendinous xanthomatosis: A rare disorder with a rare presentation. BMJ Case Rep 2012;2012. pii: Bcr2012006202.
10. Kuriyama M, Fujiyama J, Kubota R, Nakagawa M, Osame M. Osteoporosis and increased bone fractures in cerebrotendinous xanthomatosis. Metabolism 1993;42:1497-8.
11. Wang J, Jiang B, Marshall RJ, Zhang P. Arthroplasty or internal fixation for displaced femoral neck fractures: Which is the optimal alternative for elderly patients? A meta-analysis. Int Orthop 2009;33:1179-87.
12. Ning GZ, Li YL, Wu Q, Feng SQ, Li Y, Wu QL. Cemented versus uncommented hemiarthroplasty for displaced femoral neck fractures: An updated meta-analysis. Eur J Orthop Surg Traumatol 2014;24:7-14.
13. Sah AP, Thornhill TS, LeBoff MS, Glowacki J. Correlation of plain radiographic indices of the hip with quantitative bone mineral density. Osteoporos Int 2007;18:1119-26.
14. Kuo CL, Tan SH, Lee HC. Intra-operative fractures in cementless bipolar hemiarthroplasty. J OrthopSurg (Hong Kong) 2015;23:218-22.
15. Bezwada HP, Shah AR, Harding SH, Baker J, Johanson NA, Mont MA. Cementless bipolar hemiarthroplasty for displaced femoral neck fractures in the elderly. J Arthroplasty 2004;19 7 Suppl 2:73-7.
 |
 |
 |
 |
 |
| Dr. Witchuree Wejjakul | Dr. Swist Chatmaitri | Dr. Thongek Wattanarojanaporn | Dr. Anuwat Pongkunakorn | Dr. Chupong Ittiwut |
| How to Cite This Article: Wejjakul W, Chatmaitri S, Wattanarojanaporn T, Pongkunakorn A, Ittiwut C, Shotelersuk V. Bilateral Femoral Neck Fractures in Cerebrotendinous Xanthomatosis Treated by Hip Arthroplasties: The First Case Report and Literature Review. . Journal of Orthopaedic Case Reports 2017 Sep-Oct;7(5):54-58 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




