[box type=”bio”] Learning Points for this Article: [/box]
To always consider infection as a possible etiology when treating a pathologic fracture.
Case Report | Volume 7 | Issue 6 | JOCR November – December 2017 | Page 85-88| Nathan M. Krebs, Ryan C. Krebs, Amjad M. Yaish. DOI: 10.13107/jocr.2250-0685.962
Authors: Nathan M. Krebs [1], Ryan C. Krebs [2], Amjad M. Yaish [1]
[1] Department of Orthopedic Surgery, McLaren Macomb Medical Center, Michigan State University, Statewide Campus System, Michigan, USA.
[2] Michigan State University, College of Osteopathic Medicine, Michigan, USA.
Address of Correspondence:
Dr. Nathan M. Krebs,
Department of Orthopedic Surgery, McLaren Macomb Medical Center, Michigan State University, Statewide Campus System, 1000 Harrington St., Mount Clemens, MI 48043, USA.
E-mail: krebsnm@gmail.com
Abstract
Introduction: Hematogenous osteomyelitis of long bones in immunocompetent adults is extremely rare and uncommonly presents as a pathological fracture.
Case Report: A 53-year-old Caucasian male presented with an atraumatic mid-shaft femur fracture secondary to hematogenous osteomyelitis. The organism was found to be Streptococcus anginosus. The patient required multiple surgical debridements and was treated with an antibiotic-impregnated cement rod and external fixator along with IV Rocephin. Furthermore, the patient was on chronic Carbamazepine therapy for the refractory bipolar disorder. We discuss the effect cytochrome p450 inducing medications have on bone health and how this may have contributed to this rare presentation of pathologic fracture.
Conclusion: We report a rare case of femoral osteomyelitis presenting as a pathologic fracture. Treatment involves multiple surgeries and an extended recovery.
Keywords: Femur osteomyelitis, pathologic fracture, hematogenous, Streptococcus anginosus.
Introduction
Pathologic femur fractures in adults secondary to osteomyelitis is an uncommon sequela of the disease process. Most commonly, pathologic long bone fractures in adults aged >40 years result from occult malignancy, which has metastasized to bone [1]. Hematogenous osteomyelitis of long bones in immunocompetent adults is extremely rare, and there are few reports that have ever been published. This condition causing a pathologic fracture is even more rare as only 1 report could be found in the English-language medical literature [2]. We present a case of femoral osteomyelitis, which presented initially as a pathologic fracture.
Case Report
The patient was a 53-year-old Caucasian male presenting to the emergency department with a spontaneous pathologic right mid-shaft femur fracture that occurred while standing in the shower. He did not suffer any other injuries at that time. He admitted to a fall 3 weeks prior, in which he bumped his right thigh in a low energy mechanism during a near syncopal episode. It was ascertained that he had antecedent progressive right knee pain along with new-onset night sweats since the time of the incident. The patient denied any history of cancer or any other history of previous trauma. The patient had an extensive medical history including bipolar disorder, depression, chronic back pain, noninsulin dependent diabetes mellitus, and history of DVT and PE. In addition, he had a history of a previous episode of pneumonia, which was complicated by bacteremia and an empyema 1 month before at another local hospital. Records demonstrated that the blood and empyema cultures grew alpha-hemolytic streptococcus. At the time of admission, the patient had a temperature of 97.7° Fahrenheit and pulse of 106 beats per minute. On initial physical examination, there was gross deformity of the right thigh. It was a closed injury with no obvious signs of infectious etiologies on examination. The patient was distally neurovascularly intact. In addition, the patient had an ipsilateral knee effusion in which he noted was chronic. Examination of the remainder of the extremities was clinically normal. Initial laboratory studies revealed ESR 63, CRP 15.6 and white blood cell count 10,500. Vitamin D levels and PSA’s were within normal limits. AP and lateral radiographs of the right femur showed a completely displaced, short oblique mid-shaft femur fracture with 3 cm of shortening and posterior displacement of the distal fragment (Fig. 1). There were no obvious lytic or blastic lesions appreciated in the area of the fracture. In addition, computed tomography (CT) and magnetic resonance imaging (MRI) were performed on the right femur, which did not demonstrate any further osseous abnormalities. The patient also had a CT scan of the chest, abdomen, and pelvis to rule out occult malignancy; all were within normal limits. The patient was subsequently brought to the OR the following day for an open bone biopsy of the fracture site followed by placement of a reamed cephalomedullary nail with a distal locking screw. The patient was made weight-bearing as tolerated on his right lower extremity. Specimens of the biopsy along with the reamings were sent to pathology, which showed only devitalized bone fragments with the adjacent prominent fibrinoid material, blood, and mixed inflammation. The patient did suffer an iatrogenic fracture of the lateral cortex of the lateral femur as a result of the surgery, which did not change the treatment plan. In addition to the specimens being sent to pathology, they were additionally sent to microbiology for Gram stain, aerobic and anaerobic cultures, along with fungal cultures. The initial Gram stain, fungal and anaerobic cultures were negative. After 4 days of incubation, Streptococcus anginosus was grown on the aerobic cultures but failed to survive for sensitivity testing. The patient had already been discharged and was not seen again until initial follow-up visit at 2 weeks. At this point, he had developed a draining sinus tract from the incision site over the area of the fracture. Cultures were taken again in office, which demonstrated S. anginosus. Labs demonstrated a CRP of 28.1, ESR of 128, and WBC 9,600. Blood cultures were negative, and an echocardiogram was performed and did not suggest findings of endocarditis. Temperature was 98 degrees Fahrenheit and the pulse was 100. The patient was brought to the OR for the second time in which an irrigation and debridement was performed along with the use of a reamer irrigator aspirator (RIA) to thoroughly irrigate the intramedullary canal of the femur. A new cephalomedullary nail was then placed along with a distal locking screw. Additional cultures taken at the time of the second surgery grew S. anginosus, which again failed to thrive for sensitivity testing. With the recommendations of infectious disease, the patient was given a PICC line and prescribed 2 g of Rocephin daily for 8 weeks. He was weight-bearing as tolerated following the surgery.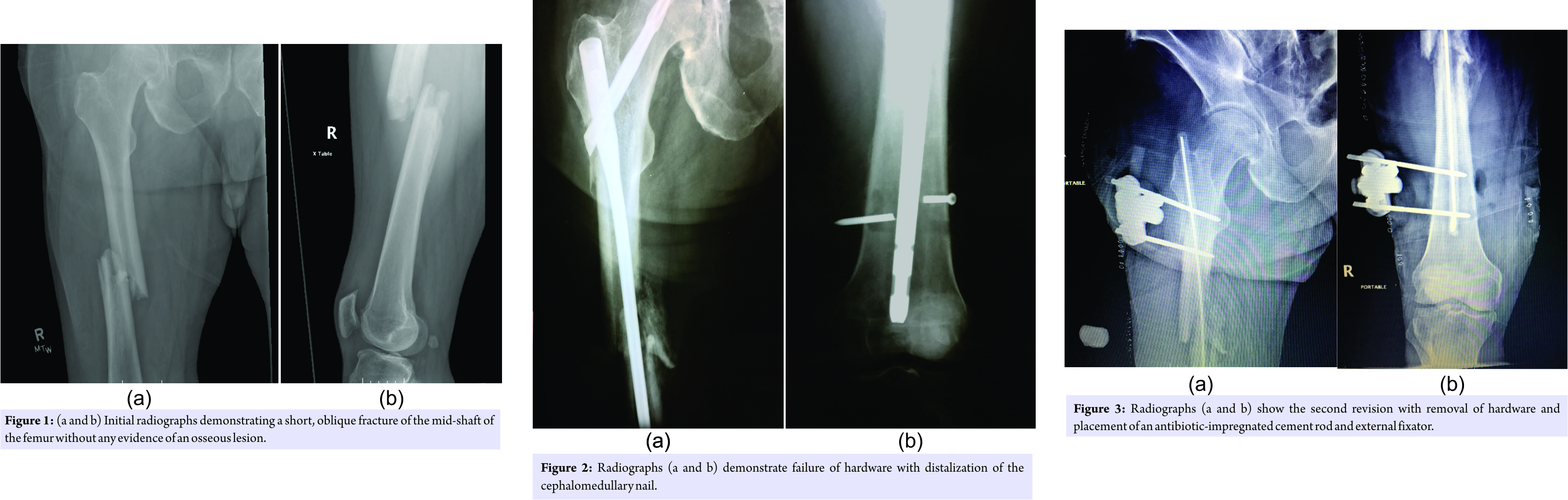
Approximately 1 month following the second surgery the patient presented for a follow-up appointment with pain in his right thigh. X-rays demonstrated failure of the cephalomedullary nail with distalization secondary to fracture of the distal locking screw with collapse at the fracture site (Fig. 2). The patient was brought back to the OR for removal of the nail along with irrigation and debridement of the femur with an RIA. Following this, a vancomycin and gentamicin antibiotic-impregnated cement rod were placed and an external fixator was applied (Fig. 3). The patient was made non-weight bearing on his right leg for 6 weeks. Infectious Disease recommended an additional 6 weeks of Rocephin 2 g daily. The patient was subsequently brought back to the OR 6 weeks later for an exchange of the external fixator. Imaging demonstrated that callus had begun to form at the fracture site. After another 6 weeks with the external fixator in place and intravenous Rocephin, the patient achieved union at the fracture site, and the cement rod and external fixator were removed with no evidence of residual infection.
Discussion
Osteomyelitis is a well-known condition and typically requires an extended time of parenteral antibiotics and multiple surgical debridements for recovery. Most commonly in adults, it is caused by Staphylococcus aureus and is typically associated with an open fracture or spread by contiguous soft tissue infection [2, 3]. This case demonstrates an example of hematogenous spread of infection to the mid-shaft of the femur. The history suggests an aggressive destructive process that resulted in a pathologic fracture. There are only a handful of reports that were found in the literature of hematogenous osteomyelitis of the femur [2, 4, 5, 6]. In the setting of pathologic fracture, it is important to be cognizant of osteomyelitis as a possible cause. The differential diagnosis includes metastatic bone disease, multiple myeloma, lymphoma, primary malignant bone tumor, destructive benign bone lesion, and non-neoplastic conditions [1]. Imaging was not able to delineate a focal process occurring at the fracture site, which included radiographs, CT, and MRI. Inflammatory markers were elevated at the initial evaluation but would be expected to be elevated in the setting of a femur fracture. This case demonstrates the importance of bone biopsy along with routine cultures in the setting of an injury that is not concordant with the mechanism. Griffen et al. states that while a variety of sites in the human body claim S. anginosus as the etiology of infection, osteomyelitis in any anatomical location is distinctly unusual. In a review of 186 cases of S. anginosus group infection, for example, only a single instance of bone infection was documented [7]. S. anginosus was identified in multiple bone biopsies in our patient. It is a subgroup of Viridans streptococci and is a facultative anaerobe that resides in the oral cavity and bowel. S. anginosus should be considered a true pathogen whenever isolated from humans [8]. The vast majority of cases of osteomyelitis in adults are caused by S. aureus, followed by Pseudomonas and Enterobacteriaceae [9]. Examination of the area of acute osteomyelitis by microscopy reveals an acute suppurative inflammation in which bacteria or other microorganisms are embedded. Various inflammatory factors, and leukocytes themselves contribute to tissue necrosis and the destruction of bone trabeculae and bone matrix. Vascular channels are compressed and obliterated by the inflammatory process, and the resulting ischemia also contributes to bone necrosis [3, 10]. The resulting weak and diseased bone hampers the ability of bone to heal and greatly increases risk of failure of fixation. Thein et al. reported that the 2 patients treated for a pathologic fracture in their case series required an average of five surgical interventions [2]. Care must be taken to debride all necrotic tissue to clear the infection. Final fixation should not be placed until there is evidence that the infection has resolved [11]. It is paramount that the extremity is protected and non-weight bearing during the extensive period of time required for healing to occur in this setting. The patient had an extensive psychiatric history with the prolonged use of carbamazepine. It is known that carbamazepine, along with other antiepileptic drugs that are inducers of the cytochrome P450 enzyme system, is associated with altered bone metabolism and decreased bone density. Current theories suggest it involves an increase in bone turnover caused by a reduction of the bioavailable Vitamin D along with an altered response of osteocytes to parathyroid hormone [12]. We hypothesize that the patient likely seeded his right femur from prior bacteremia, which when combined with compromised bone from the use of long-term carbamazepine led to the unusual presentation of pathologic fracture.
Conclusion
We report a case of hematogenous femoral osteomyelitis presenting as a mid-shaft femur fracture. This presentation has never before been reported in the medical literature and illustrates the need to consider a broad differential diagnosis and obtain biopsy and cultures in treating a pathologic fracture. Furthermore, it supports the findings that femoral osteomyelitis is associated with a long course of recovery with multiple surgical interventions and long-term intravenous antibiotics.
Clinical Message
A thorough evaluation is required in the work-up of a patient with a pathologic fracture, including the appropriate lab studies, imaging, biopsy, and cultures. A long bone fracture secondary to hematogenous osteomyelitis represents a complex surgical dilemma in which the diseased bone has severely diminished structural integrity. External fixation in conjunction with an antibiotic-impregnated cement rod is a way to stabilize the fracture while the infection is treated with intravenous antibiotics.
References
1. Weber KL. Evaluation of the adult patient (aged >40 years) with a destructive bone lesion. J Am Acad Orthop Surg 2010;18:169-79.
2. Thein R, Tenenbaum S, Chechick O, Leshem E, Chechik A, Liberman B, et al. Delay in diagnosis of femoral hematogenous osteomyelitis in adults: An elusive disease with poor outcome. Isr Med Assoc J 2013;15:85-8.
3. Lew DP, Waldvogel FA. Osteomyelitis. Lancet 2004;364:369-79.
4. Roberts DE. Femoral osteomyelitis after tooth extraction. Am J Orthop (Belle Mead NJ) 1998;27:624-6.
5. Seybold U, Talati NJ, Kizilbash Q, Shah M, Blumberg HM, Franco-Paredes C, et al. Hematogenous osteomyelitis mimicking osteosarcoma due to community associated methicillin-resistant Staphylococcus aureus. Infection 2007;35:190-3.
6. Zalavras CG, Rigopoulos N, Lee J, Learch T, Patzakis MJ. Magnetic resonance imaging findings in hematogenous osteomyelitis of the hip in adults. Clin Orthop Relat Res 2009;467:1688-92.
7. Griffin AT, Timbrook T, Harting J, Christensen D. Streptococcus anginosus group and osteomyelitis: A single centre clinical experience. Postgrad Med J 2013;89:262-5.
8. Stratton CW. Infections Due to the Streptococcus anginosus (Streptococcus milleri) group. In: Sexton DJ, editors. Up To Date. Waltham: Mass; 2017. Available from: http://www.uptodate.com. [Last accessed on 2017 Mar 10].
9. Kosher S. Osteomyelitis. Medscape. Available From: http://www.emedicine.medscape.com/article/1348767-overview#a4. [Last published on 2016 Sep 13; Last accessed on 2017 Mar 11].
10. Parsons B, Strauss E. Surgical management of chronic osteomyelitis. Am J Surg 2004;188:57-66.
11. Lew DP, Waldvogel FA. Osteomyelitis. N Engl J Med 1997;336:999-1007.
12. Pack AM. The association between antiepileptic drugs and bone disease. Epilepsy Curr 2003;3:91-5.
 |
 |
 |
| Dr. Nathan M. Krebs | Mr. Ryan Krebs | Dr. Amjad Yaish |
| How to Cite This Article: Krebs NM, Krebs RC, Yaish AM. Femoral Osteomyelitis Presenting as a Pathologic Fracture in a 53 Year Old Male: A Rare Case Report. Journal of Orthopaedic Case Reports 2017 Nov-Dec; 7(6): 85-88 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




