[box type=”bio”] Learning Point for this Article: [/box]
Activity modification may play a role in the progression of metal ion production and adverse local tissue reactions in patients with total hip arthroplasty and mixed-metal modular femoral necks.
Case Report | Volume 8 | Issue 1 | JOCR Jan – Feb 2018 | Page 44-47| Michael S Reich, Richard H Walker. DOI: 10.13107/jocr.2250-0685.992
Authors: Michael S Reich[1], Richard H Walker[1]
[1]Division of Orthopaedic Surgery, Scripps Clinic, USA.
Address of Correspondence:
Dr. Richard H Walker,
10666 N. Torrey Pines Rd., MS116, La Jolla, CA 92037, USA.
E-mail: walker.richard@scrippshealth.org
Abstract
Introduction: Femoral neck modularity in total hip arthroplasty (THA) affords the surgeon the ability to optimize femoral neck length, offset, and version, thereby theoretically improving restoration of patient anatomy and biomechanics. The effect of activity on serum metal ion levels in patients with a THA with a mixed-metal modular neck design has not yet been described.
Case Report: A 63-year-old male underwent THA utilizing a femoral stem with a mixed-metal modular femoral neck. After the stem was voluntarily recalled, he was indicated to be monitored for manifestations of modular junction corrosion and development of adverse local tissue reactions (ALTR). An association between activity levels and serial serum cobalt levels was demonstrated.
Conclusion: In this patient with a THA incorporating a mixed-metal modular femoral neck, modification of activity intensity may have played a role in altered corrosion generation, as indicated by serum metal ion levels. In turn, this may play a role in the progression of ALTR.
Keywords: Activity, adverse local tissue reactions, cobalt, modular femoral stem, total hip arthroplasty.
Introduction
Modularity at the total hip arthroplasty (THA) femoral neck was introduced to afford the surgeon the ability to optimize femoral neck length, offset, and version, thereby improving restoration of patient anatomy and biomechanics. However, two such modular implants with mixed-metal contact at such a modular junction (Rejuvenate and ABG II, Stryker Orthopaedics, Mahwah, New Jersey) were voluntarily recalled due to higher than acceptable early failures seen during post-market monitoring [1]. 2-year survival with the Rejuvenate stem was reported to be 69.3%, and the 3-year survival was 30.3% [2]. Reasons for implant failure focus on the development of adverse local tissue reaction (ALTR) [2, 3, 4], believed to be due to corrosion and fretting at the modular junction of the cobalt-chromium (CoCr) neck and titanium (Ti) stem [2, 3, 4, 5]. Elevated serum metal ion levels, preferentially Co over Cr, have been associated with the resultant ALTR [3, 4, 5]. Activity levels have been studied with respect to wear and corrosion in a variety of contexts. For metal- or ceramic-on-polyethylene THA articulations, some data suggests wear is related to activity [6, 7, 8, 9], whereas other studies contradict this premise [10, 11, 12]. Recent mechanically-assisted crevice corrosion (MACC) data for metal-on-polyethylene THA found no relationship between Co or Cr levels and activity [13]. The effects of activity on metal ion levels in THA patients, with hard on soft bearings, with mixed-metal modular femoral stems, have not been studied. Increased activity would, theoretically, correlate with increased hip forces, and, by extrapolation, increased risk of MACC at modular implant junctions. With other factors being equal, increased junction wear could reasonably result from increased activity cycles and forces. The effect of activity intensity on serum metal ion level, as a surrogate for corrosion, in patients with a THA with a modular neck design has not yet been elucidated. We present a case report of a patient with a Ti femoral stem with a CoCr modular neck whose initial serum Co levels decreased after specific and concerted effort to decrease activity level.
Case Report
A 63-year-old male, whose medical history was notable only for mild left hip dysplasia, initially presented to our clinic with a 2-year history of progressively worsening left groin pain. Before his pain was intensifying, he routinely engaged in high-level fitness and recreational activities, including jogging and mountain hiking. In spite of non-operative treatments including nonsteroidal anti-inflammatory medications, activity restriction, and several intra-articular corticosteroid injections, his pain progressed and began interfering with routine activities of daily living. On exam, he was healthy appearing, with a body mass index of 23.5 kg/m2, and an antalgic gait. He demonstrated full strength with hip flexion and abduction, with a range of motion from 0 to 120° of flexion, 20° of internal rotation (which was painful), 30° of external rotation, and 30° of abduction. Radiographs and magnetic resonance imaging (MRI) demonstrated partial uncovering of the femoral head with end-stage degenerative changes of the left hip. Spine pathology was excluded. He, therefore, elected to undergo THA. At THA, acetabular components included a non-cemented hydroxyapatite-coated Ti acetabular shell with modular cross-linked polyethylene (Stryker Trident PSL cup, 54 mm diameter; X3 0° liner), a ceramic modular head (Stryker Biolox Delta, 40 mm diameter, +0 mm Ti trunnion adapter sleeve), a non-cemented hydroxyapatite-coated Ti femoral stem (Stryker Rejuvenate SPT stem, size #10), and a CoCr modular neck (Stryker Rejuvenate, V40 trunnion taper, 34 mm length, 0° version, 127° angle neck). A calcar cable was placed due to a limited vertical calcar fracture, and full weight-bearing was permitted. After routine post-operative care, including peri-operative antibiotics, deep vein thrombosis prophylaxis, and physical therapy, the patient was discharged home 2 days postoperatively after an uneventful hospitalization. An anteroposterior pelvis X-ray obtained in the post-anesthesia care unit is shown in Fig. 1.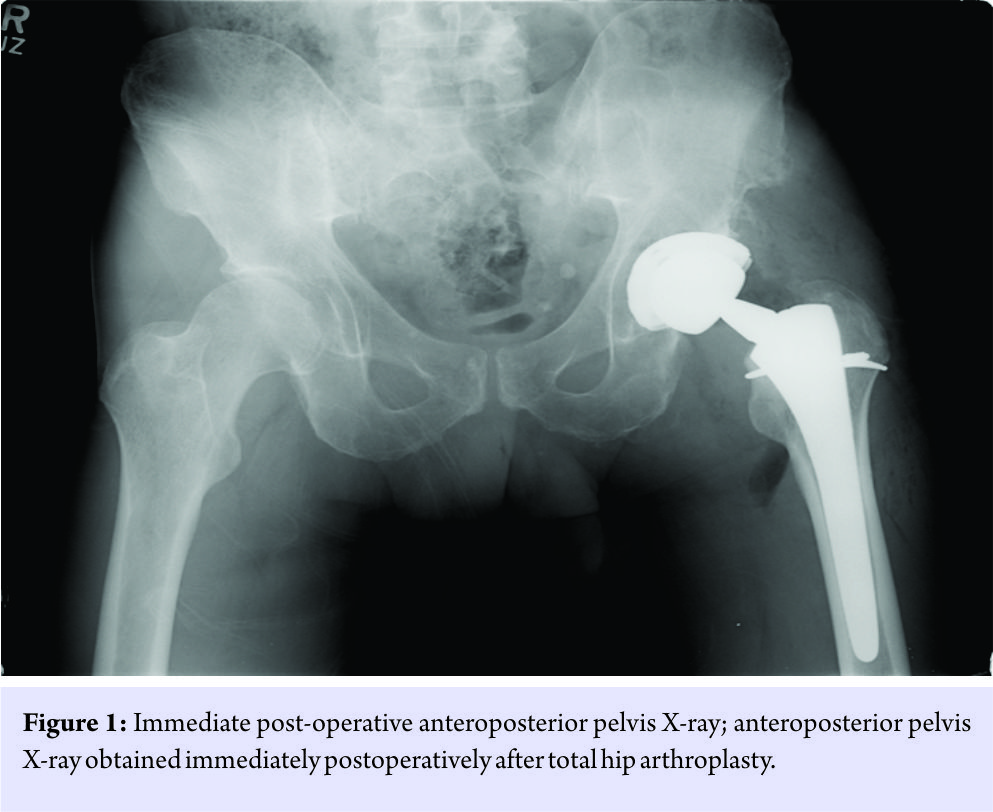
Routine post-operative monitoring was uneventful. At his 6-week follow-up, he was progressing well with stable radiographs. Per our usual THA recommendations, the patient was advised to progress with non-impact loading activities. At his 3-month follow-up, Harris hip score pain (HSS-P) question was 1 out of 6 (no pain), and UCLA activity score (UCLA-AS) was 9 out of 10 (sometimes participating in impact sports). The patient noted that he participated in impact-loading activities, including jogging and hiking. He was again advised of the optimal activity level for THA patients, emphasizing non-impact activities (e.g., bicycling and swimming). At his 12-month follow-up, HSS-P and UCLA-AS remained 1 and 9, respectively, and radiographs remained stable. Discussion regarding activity was the same as at the 3-month follow-up. Routine 5-year follow-up was planned. Voluntary recall of his femoral stem occurred 2 years postoperatively. He was informed of the risks of ALTR associated with this stem and invited for follow-up, HHS-P and UCLA-AS were again 1 and 9, respectively. Radiographs demonstrated a well-fixed THA in appropriate alignment without evidence of periprosthetic osteolysis, calcar femorale rounding, or polyethylene wear (Fig. 2). Baseline serum Co (4.8 mcg/L, reference normal <3.9), serum Cr (<1.0 mcg/L, normal ≤5.0), erythrocyte sedimentation rate (2 mm/hr, normal <20), and C reactive protein (<3.0 mg/L, normal <10.0) were obtained. Per protocol at our institution for evaluating asymptomatic patients with this recalled implant and with elevated serum Co, a cross-sectional anatomy study by ultrasound scan was obtained, demonstrating a 2.7 × 1.2 cm fluid collection anterior to the hip without other sequelae of ALTR. He was again advised against impact loading activities.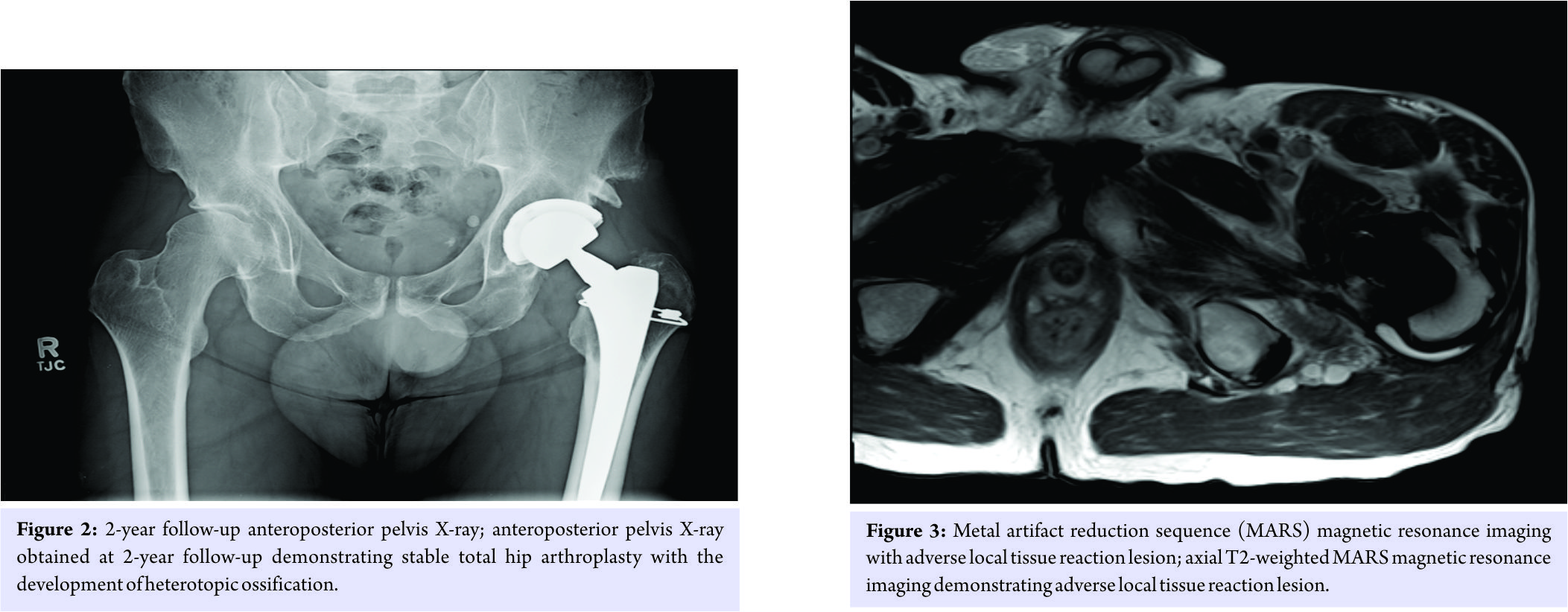
Annual follow-up was planned to monitor for any clinical deterioration or progression of ALTR. At 34-month follow-up, serum Co had increased to 6.2 mcg/L. HHS-P and UCLA-AS remained 1 and 9. Due to increase in Co level, MRI with metal artifact reduction sequence (MARS) was obtained and demonstrated a 3.6 × 0.7 cm fluid collection posterior to the hip (Fig. 3), but without other sequelae of ALTR. At 41-month follow-up, serum Co reached 7.6 mcg/L. HHS-P was now 2 (slight or occasional pain, with no compromise inactivity). The patient stated that he had participated in mountain hiking shortly before this Co level was obtained. Repeat MARS MRI demonstrated a 4.0 × 0.8 cm fluid collection posterior to the hip, without other sequelae of ALTR. After further counseling, the patient elected revision arthroplasty, but deferred surgery until his work calendar allowed. In the interim, he planned stationary bicycling and swimming for fitness activity. 45 months after index THA, the patient presented for pre-operative evaluation. He had eliminated high-impact activities. He wished pre-operative re-check of serum Co, which showed a decrease to 5.3 mcg/L. With continued satisfactory THA clinical outcome, the patient deferred revision surgery, opting to maintain non-impact-loading activity level and monitor serum Co. At his 4.5-years follow-up visit, he remained satisfied with his THA, with HHS 96, HHS-P 2, UCLA-AS 8 (very active, but no impact sports), and Co 2.2 mcg/L, and was bicycling and swimming for fitness. The patient wished to continue non-impact-loading activity level and monitor symptoms and serum Co. He recently had his Co level re-checked at 5.0 years postoperatively, and it was 1.2 mcg/L.
Discussion
ALTR is a devastating complication of MACC, which has led to a high revision rate in patients who received the Stryker Rejuvenate femoral stem with a modular neck [2]. While a direct relationship between serum metal ion levels and the development of ALTR is lacking [3], metal ion level has been included as predictive factor. As such, algorithms which include serum ion levels have been published to guide the evaluation and treatment of at-risk patients [14, 15]. To our knowledge, this represents the first case describing a diminishing serum metal ion serum level with a willful decrease in activity level in a patient who received a modular femoral stem. Fortunately, despite developing increasing serum Co levels, this patient developed only limited signs of developing ALTR on MARS MRI while remaining relatively asymptomatic. He remains quite active, as noted by his HSS, UCLA-AS, and reported daily function level. Due to the patient’s lack of progression of symptoms and manifestation of ALTR, we are afforded unique insight into a potential relationship between serum Co level and activity. As noted in the previous literature for modular neck designs [3, 4, 5], Co levels were elevated over Cr levels (in fact, Cr level remained normal throughout follow-up evaluation). Of interest, the temporal relationship between the cessation of high-impact activities and decline in Co levels appear to be linked.
Conclusion
In that this case is only a single instance describing an association between activity intensity and Co levels in a patient with a THA femoral stem with modular neck design, we recognize that this single case cannot represent a conclusion of causality. This patient elected to delay revision surgery, serendipitously affording observation of the effect of diminishing a previously high activity level. We do not advocate this report as justification to manage patients non-operatively who have elevated ion levels, painful symptomatology, ALTR lesions, or any other manifestation of a failing THA. This single case report suggests the possibility that, in asymptomatic patients with a THA with a modular neck who are currently being observed, activity modification may play a role in the natural progression of metal ion generation and ALTR pathology. However, further study is warranted to elaborate on the phenomenon presented here, that being a potential correlation between activity level and MACC-related generation of serum metal ions.
Clinical Message
In asymptomatic patients with a total hip replacement with a mixed-metal modular femoral neck design, activity modification may play a role in the natural progression of metal ion generation and adverse local tissue reaction pathology.
References
1. Stryker Initiates Voluntary Product Recall of Modular-Neck Stems. Action Specific to Rejuvenate and ABG II Modular-Neck Stems: Food and Drug Administration. New York, NY: US Department of Health and Human Services; 2012.
2. Nawabi DH, Do HT, Ruel A, Lurie B, Elpers ME, Wright T, et al. Comprehensive analysis of a recalled modular total hip system and recommendations for management. J Bone Joint Surg Am 2016;98:40-7.
3. Liow MH, Urish KL, Preffer FI, Nielson GP, Kwon YM. Metal ion levels are not correlated with histopathology of adverse local tissue reactions in taper corrosion of total hip arthroplasty. J Arthroplasty 2016;31:1797-802.
4. Walsh CP, Hubbard JC, Nessler JP, Markel DC. Revision of recalled modular neck Rejuvenate and ABG femoral implants. J Arthroplasty 2015;30:822-6.
5. Cooper HJ, Urban RM, Wixson RL, Meneghini RM, Jacobs JJ. Adverse local tissue reaction arising from corrosion at the femoral neck-body junction in a dual-taper stem with a cobalt-chromium modular neck. J Bone Joint Surg Am 2013;95:865-72.
6. Schmalzried TP, Shepherd EF, Dorey FJ, Jackson WO, dela Rosa M, Fa’vae F, et al. The John Charnley award. Wear is a function of use, not time. Clin Orthop Relat Res 2000;381:36-46.
7. Feller JA, Kay PR, Hodgkinson JP, Wroblewski BM. Activity and socket wear in the Charnley low-friction arthroplasty. J Arthroplasty 1994; 9(4):341-5.
8. Ollivier M, Frey S, Parratte S, Flecher X, Argenson JN. Does impact sport activity influence total hip arthroplasty durability? Clin Orthop Relat Res 2012; 470:3060-6.
9. Devane PA, Horne JG, Martin K, Coldham G, Krause B. Three-dimensional polyethylene wear of a press-fit titanium prosthesis: Factors influencing generation of polyethylene debris. J Arthroplasty 1997;12:256-66.
10. Sechriest VF 2nd, Kyle RF, Marek DJ, Spates JD, Saleh KJ, Kuskowski M. Activity level in young patients with primary total hip arthroplasty. J Arthroplasty 2007;22:39-47.
11. Goldsmith AA, Dowson D, Wroblewski BM, Siney PD, Fleming PA, Lane JM. The effect of activity levels of total hip arthroplasty patients on socket penetration. J Arthroplasty 2001;16:620-7.
12. Lubbeke A, Garavaglia G, Barea C, Stern R, Peter R, Hoffmeyer P. Influence of patient activity on femoral osteolysis at five and ten years following hybrid total hip replacement. J Bone Joint Surg Br 2011;93:456-63.
13. McGrory BJ, Payson AM, MacKenzie JA. Elevated intra-articular cobalt and chromium levels in mechanically assisted crevice corrosion in metal-on-polyethylene total hip arthoplasty. J Arthroplasty 2017;32:1654-8.
14. Kwon YM. Evaluation of the painful dual taper modular neck stem total hip arthroplasty: Do they all require revision? J Arthroplasty 2016;31:1385-9.
15. Elmallah RK, Cherian JJ, Meneghini RM, Hozack WJ, Westrich GH, Mont MA. How to approach a recalled dual modular hip implant: An update. J Arthoplasty 2016;31:2646-52.
 |
 |
| Dr. Michael Reich | Dr. Richard Walker |
| How to Cite This Article: Reich MS, Walker RH. Activity-related Changes in Cobalt Levels in a Total Hip with a Modular Femoral Stem: A Case Report. Journal of Orthopaedic Case Reports 2018 Jan-Feb; 8(1): 44-47 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




