[box type=”bio”] Learning Point for this Article: [/box]
Arthroscopic superior capsule reconstruction was not indicated for patients with deltoid muscle dysfunction, but it remained a viable option if the palsy was considered reversible and it could be performed effectively after palsy was been relieved.
Case Report | Volume 8 | Issue 2 | JOCR Mar – Apr 2018 | Page 100-103| Furuya Kanji, Nishinaka Naoya, Uehara Taishi, Tsutsui Hiroaki. DOI: 10.13107/jocr.2250-0685.1070
Authors: Furuya Kanji[1], Nishinaka Naoya[1],[2], Uehara Taishi[1], Tsutsui Hiroaki[3]
[1]Department of Orthopaedic Surgery, Showa University Fujigaoka Hospital1-30, Fujigaoka, Aoba-Ku, Yokohama, Japan.
[2]Showa University Research Institute for Sport and Exercise Sciences2-1-1, Fujigaoka, Aoba-Ku, Yokohama, Japan.
[3]Department of Orthopaedic Surgery, Showa University School of Medicine1-5-8, Hatanodai, Shinagawa-Ku, Tokyo, Japan.
Address of Correspondence:
Dr. Kanji Furuya,
Department of Orthopaedic Surgery, Showa University Fujigaoka Hospital1-30, Fujigaoka, Aoba-Ku, Yokohama 227-8501, Japan.
E-mail: k.ayuruf.5@gmail.com
Abstract
Introduction: This report describes a case of irreparable massive rotator cuff tear and axillary nerve palsy associated with shoulder dislocation successfully treated by arthroscopic superior capsule reconstruction (ASCR), with a favorable post-operative outcome.
Case Report: A 76-year-old man, injured from a fall while walking, presented to another hospital with right shoulder pain and a limited range of motion (ROM) 3 days after the injury. Given a diagnosis of right shoulder dislocation, he received manual reduction followed by immobilization with a sling. He continued to experience difficulty in performing active ROM exercises of the shoulder and underwent magnetic resonance imaging, which revealed an irreparable extensive rotator cuff tear involving the supraspinatus and infraspinatus muscles. He was then referred to our hospital 2 months after the injury. Examination revealed atrophy of the supraspinatus and infraspinatus muscles, atrophy of the deltoid muscle and hypoesthesia, likely due to axillary nerve palsy, and a marked limitation of active ROM with flexion, abduction and lateral rotation angles of 10°each. ASCR was considered for treating the irreparable rotator cuff tear. Since the technique is not indicated for patients with deltoid paralysis, the operation was delayed until signs of improved axillary nerve palsy were observed at 6 months after the injury. The patient started passive ROM training the day after the operation while wearing a shoulder abduction orthosis for 3 weeks, followed by immobilization with a sling for 2 weeks. Thereafter, he started active exercise. The axillary nerve palsy was almost completely resolved 3 months after the operation. He achieved a ROM comparable to that of the unaffected side at 1 year after operation. He has had an uneventful post-operative course for 2 years after operation.
Conclusion: We encountered a rare, difficult-to-treat case of irreparable extensive rotator cuff tear with axillary nerve palsy after a shoulder dislocation. ASCR, although not indicated for patients with deltoid muscle dysfunction, provided a favorable post-operative outcome when performed after confirmation of signs of improved palsy.
Keywords: Anterior dislocation, arthroscopic superior capsule reconstruction, axillary nerve palsy, irreparable rotator cuff tear.
Introduction
Of all the complications of shoulder dislocation, axillary nerve palsy and rotator cuff tear account for 9–10% [1] and 14–63% [2], respectively. Neviaser et al. reported that axillary nerve palsy occurred in 7.8% of the patients aged ≥35 years with a concurrent shoulder dislocation and rotator cuff tear [3]. The coexistence of these two conditions is referred to as “the terrible triad of the shoulder” and tends to be refractory to treatment [3, 4]. While various surgical procedures have been reported for the repair of chronic large tears or massive rotator cuff tear, there is no established procedure to achieve complete repair due to factors that preclude repair, such as degradation of a torn tendon, muscle atrophy, and fatty infiltration, and a high rate of post-operative re-tear [5, 6, 7]. This report describes a case of irreparable massive rotator cuff tear and axillary nerve palsy associated with shoulder dislocation successfully treated by arthroscopic superior capsule reconstruction (ASCR), with a favorable post-operative outcome.
Case Report
Presentation and diagnosis
The patient was 76-year-old male, right-handed, living by himself, and fully able to walk independently. His chief complaint was right shoulder pain, limited range of motion (ROM) in the right shoulder. He fell on his right shoulder while walking and injured it. He visited another hospital 3 days after the injury where he was diagnosed with dislocation of the right shoulder and received manual reduction followed by immobilization with a sling. Due to persistent pain and limited ROM of the right shoulder, plain magnetic resonance imaging (MRI)was performed and revealed a massive rotator cuff tear. He was then referred to our hospital 2 months after the injury. Physical findings on initial examination were markedly limited ROM and decreased abductor/external rotator muscle strength were observed, with an active flexion angle of 10°, active abduction angle of 10°, active external rotation angle of 0°, and manual muscle test (MMT) for abductor and lateral rotator (at a hanging position) muscle strength of 2 (Table 1).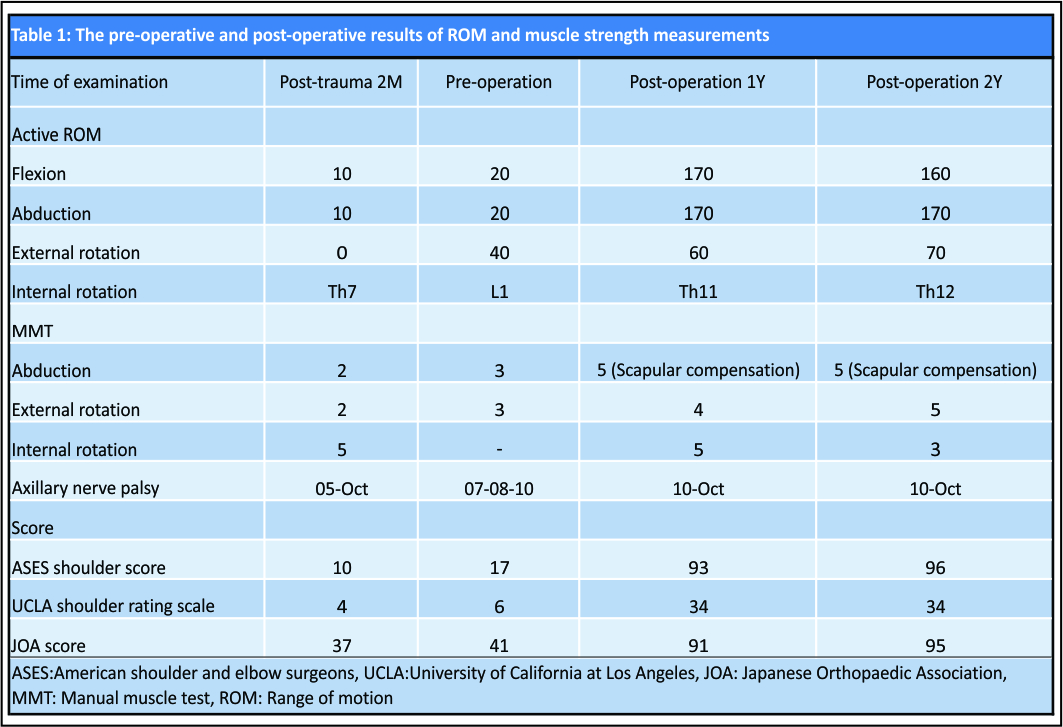 Visually discernible atrophy of the deltoid, supraspinatus and infraspinatus muscles and hypoesthesia (5/10) in the axillary nerve region were also observed. At this point, the patient was given an American shoulder and elbow surgeons (ASES) scoring system [8] of 10/100, University of California at Los Angeles (UCLA) shoulder scaling system [9] of 4/35, and Japanese Orthopaedic Association (JOA) scoring system [10] of 37/100. The plain X-ray findings were irregular glenohumeral joint surface and subacromial osteophytes, diagnosed as Grade 3 on the Hamada classification [11], were observed. The plain MRI findings were massive tear of the supraspinatus and infraspinatus muscles, which were withdrawn back to the glenoid fossa, diagnosed as Stage4 atrophy of supraspinatus muscle and Stage3 atrophy of infraspinatus muscle on the Goutallier classification was observed. The subscapular muscle was completely torn with bone fragment formation and diagnosed as Grade 3 on the ide classification [12] (Fig. 1).
Visually discernible atrophy of the deltoid, supraspinatus and infraspinatus muscles and hypoesthesia (5/10) in the axillary nerve region were also observed. At this point, the patient was given an American shoulder and elbow surgeons (ASES) scoring system [8] of 10/100, University of California at Los Angeles (UCLA) shoulder scaling system [9] of 4/35, and Japanese Orthopaedic Association (JOA) scoring system [10] of 37/100. The plain X-ray findings were irregular glenohumeral joint surface and subacromial osteophytes, diagnosed as Grade 3 on the Hamada classification [11], were observed. The plain MRI findings were massive tear of the supraspinatus and infraspinatus muscles, which were withdrawn back to the glenoid fossa, diagnosed as Stage4 atrophy of supraspinatus muscle and Stage3 atrophy of infraspinatus muscle on the Goutallier classification was observed. The subscapular muscle was completely torn with bone fragment formation and diagnosed as Grade 3 on the ide classification [12] (Fig. 1).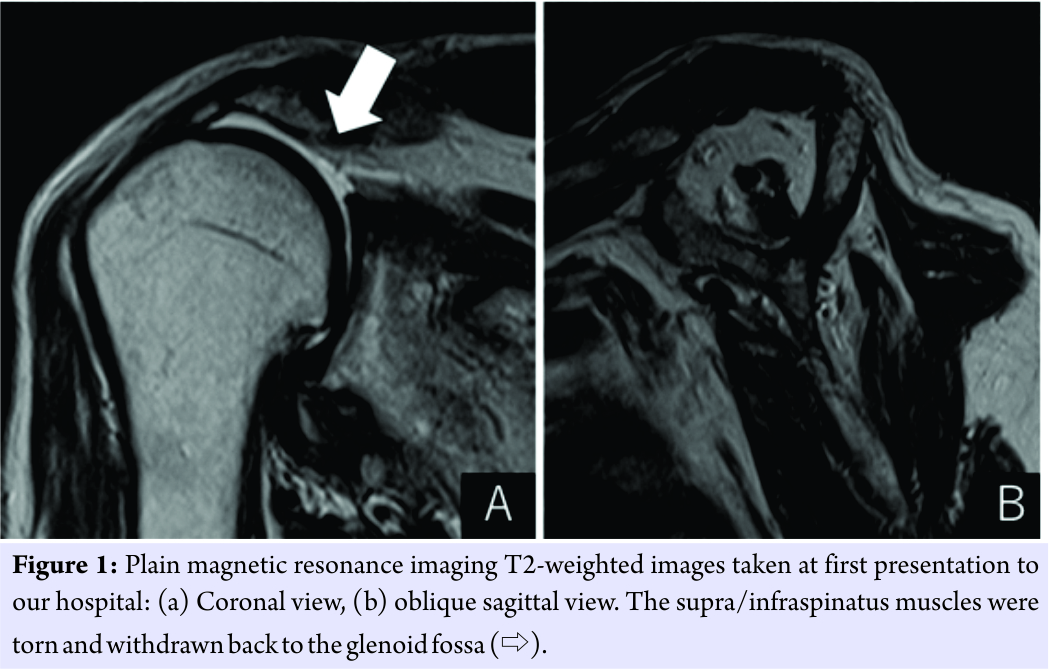 Electromyography was performed at the neurology department of our hospital to evaluate the degree of axillary nerve palsy. A motor nerve conduction study of the axillary nerve showed a marked decrease in compound muscle action potential in the deltoid muscle. An electromyogram showed a denervation potential suggestive of neurogenic changes in muscles innervated by the axillary nerve, leading to a diagnosis of axillary nerve palsy, leading to a diagnosis of neuropraxia in axillary nerve. However, muscle contraction was maintained in the axillary nerve region, suggesting the possibility of restoration. Therefore, a treatment plan was developed to conduct an outpatient rehabilitation program to improve the ROM and enhance the muscle strength of the shoulder until the palsy is improved, and then perform the surgical treatment. Hypoesthesia improved to 7–8/10 with a reduced affected area. Furthermore, noted was an improved ROM, with active flexion, abduction, and external rotation angles of 20°, 20°, and 40°, respectively, and gradual improvement in muscle strength, with an abductor and external rotator (at a hanging position) muscle strength of 2 and 3 by MMT, respectively (Fig. 2 and Table 1). Given these findings, ASCR was performed 6 months after injury.
Electromyography was performed at the neurology department of our hospital to evaluate the degree of axillary nerve palsy. A motor nerve conduction study of the axillary nerve showed a marked decrease in compound muscle action potential in the deltoid muscle. An electromyogram showed a denervation potential suggestive of neurogenic changes in muscles innervated by the axillary nerve, leading to a diagnosis of axillary nerve palsy, leading to a diagnosis of neuropraxia in axillary nerve. However, muscle contraction was maintained in the axillary nerve region, suggesting the possibility of restoration. Therefore, a treatment plan was developed to conduct an outpatient rehabilitation program to improve the ROM and enhance the muscle strength of the shoulder until the palsy is improved, and then perform the surgical treatment. Hypoesthesia improved to 7–8/10 with a reduced affected area. Furthermore, noted was an improved ROM, with active flexion, abduction, and external rotation angles of 20°, 20°, and 40°, respectively, and gradual improvement in muscle strength, with an abductor and external rotator (at a hanging position) muscle strength of 2 and 3 by MMT, respectively (Fig. 2 and Table 1). Given these findings, ASCR was performed 6 months after injury.
Treatment and follow-up
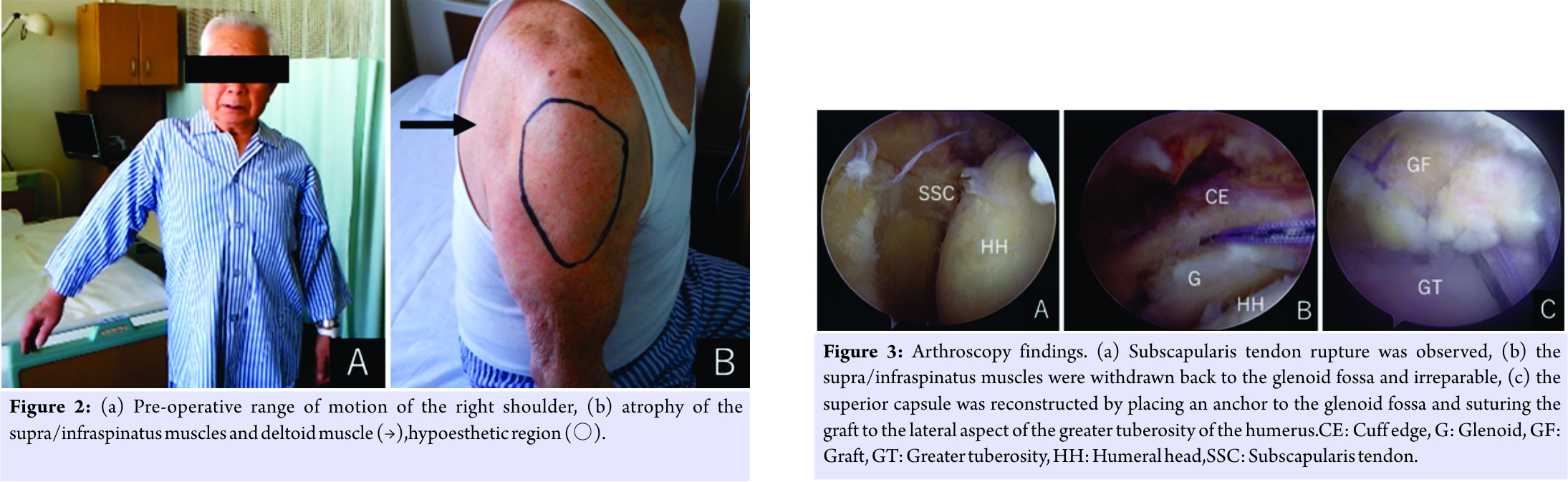
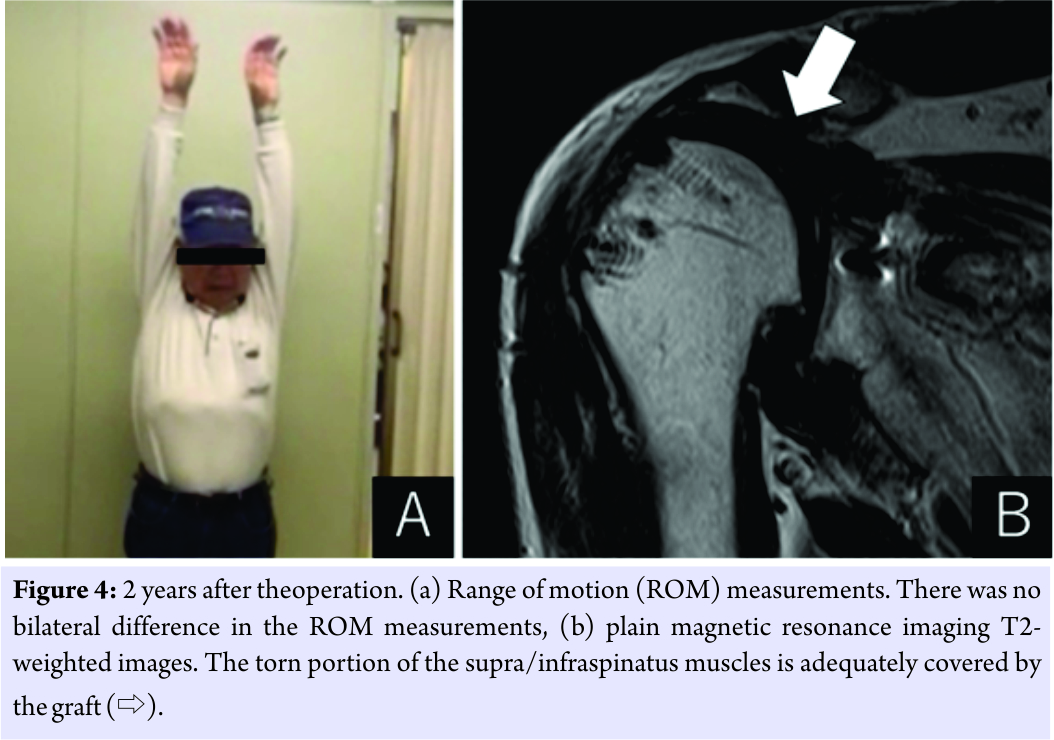
The operation was started with the patient placed in a beach chair position under general anesthesia. Two portals were made in the posterior and lateral aspects of the shoulder,and the posterior portal was used to perform intra-articular locking. Arthroscopy revealed no injury in the tendon of the long head of the biceps brachii muscle, but its origin was detached along with the labrum. The rotator cuff was extensively torn, involving the tendons of the subscapular, supraspinatus, and infraspinatus muscles, with the stumps withdrawn back to the glenoid fossa. Osteoarthritic changes were observed in the joint surface but were mild in severity. Mild injury of the glenoid labrum was observed, but it was not associated with joint dislocation under anesthesia. The subscapular muscle tear was repaired as it was considered reparable. In contrast, the supra/infraspinatus muscle tear was considered irreparable; therefore, the contralateral fascia lata was collected, folded in half and used as a graft for ASCR. Although it was initially planned to repair the humeral head side of the graft using a bridging suture, it was difficult to place four anchors due to poor bone quality. Therefore, the graft was fixed using single-row interrupted sutures. Finally, to complete the operation, the graft was attached to the residual teres minor muscle by interrupted sutures (Fig. 3). After surgery, the patient wore a shoulder abduction pillow for 3 weeks, followed by immobilization with a sling for 2 weeks. On the day after the operation, the patient started shoulder girdle relaxation, passive ROM, and periscapular muscle training. An ultrasonography performed 4 weeks after operation showed coverage of the torn portion by the graft. External fixation was removed 5 weeks after the operation,and active ROM training was started. Hypoesthesia in the axillary nerve region was almost completely resolvedat 3 months after operation, with no bilateral difference. Pain and deltoid muscle atrophy were resolved by 4.5 months after operation. During the first 2 years after operation, improvements were observed in both the ROM and muscle strength of the shoulder, with an ASES shoulder score of 96, UCLA shoulder rating scale of 34, and JOA score of 95. An MRI performed 2 years after operation also showed adequate coverage of the torn portion by the graft (Fig. 4 and Table 1).
Discussion
The ASCR technique was first reported by Mihata et al. in 2013, where the fascia lata is used to reconstruct the superior joint capsule to enhance the stability of the glenohumeral joint and thereby maintain the humeral head in the centripetal position for the functional restoration of the shoulder [13]. They have also reported that the stability of the glenohumeral joint can be further enhanced by side to side suturing of the graft to the teres minor muscle [14]. After ASCR, the perishoulder muscles, including the deltoid muscle, serve as the power source for raising the upper arm. In many cases, the post-operative shoulder function depends on the strength of these muscles. Thus, this technique is not indicated for patients with deltoid muscle dysfunction. In contrast, Martin and Limbird have recommended that treatment for massive rotator cuff tear with axillary nerve palsy should be started as soon as possible after any sign of improved axillary nerve function has been observed [4]. Simonich and Wright recommend that rotator cuff repair should be performed immediately after the tear has been diagnosed [15]. In the present case, where ASCR was not indicated, we waited for any sign of improved axillary nerve function before starting the operation, so that the post-operative rehabilitation program could be conducted smoothly. In the present case, with massive rotator cuff tear and axillary nerve palsy associated with anterior dislocation of the shoulder, we performed ASCR with a favorable post-operative outcome. We selected ASCR because achieving functional restoration was considered important for the patient to perform daily activities, as he was living by himself and the injured hand was his dominant hand; he was well aware of the importance of post-operative rehabilitation programs; arthrosis related changes were mild in severity; pain was resolved whereas limited ROM remained up to 6 months after injury, suggesting that continuing conservative treatment may lead to residual contracture of the shoulder joint; and axillary nerve palsy was improving. The outcome of the operation was favorable. Although reverse total shoulder arthroplasty is another possible option, the technique had not been approved in Japan by the time of the present operation. Moreover, given that arthrosis related changes were mild in severity, it was considered most appropriate to perform ASCR after waiting for any sign of improved axillary nerve palsy.
Conclusion
We performed ASCR on a patient with irreparable massive rotator cuff tear and axillary nerve palsy associated with dislocation of the shoulder, with a favorable post-operative outcome. ASCR was not indicated for patients with deltoid muscle dysfunction, but it remained a viable option if the palsy was considered reversible and it could be performed effectively after palsy was been relieved.
Clinical Message
This report describes a case of irreparable massive rotator cuff tear and axillary nerve injury associated with shoulder dislocation successfully treated by ASCR, with a favorable post-operative outcome. ASCR was not indicated for patients with deltoid muscle dysfunction, but it remained a viable option if the palsy was considered reversible and it could be performed effectively after palsy was been relieved
References
1. Robinson CM, Shur N, Sharpe T, Ray A, Murray IR. Injuries associated with traumatic anterior glenohumeral dislocations. J Bone Joint Surg Am 2012;94:18-26.
2. Cutts S, Prempeh M, Drew S. Anterior shoulder dislocation. Ann R Coll Surg Engl 2009;91:2-7.
3. Neviaser RJ, Neviaser TJ, Neviaser JS. Concurrent rupture of the rotator cuff and anterior dislocation of the shoulder in the older patient. J Bone Joint Surg Am 1988;70:1308-11.
4. Martin SS, Limbird TJ. The terrible triad of the shoulder. J South Orthop Assoc 1999;8:57-60.
5. Bedi A, Dines J, Warren RF, Dines DM. Massive tears of the rotator cuff. J Bone Joint Surg Am 2010;92:1894-908.
6. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 1994;304:78-83.
7. Melis B, Wall B, Walch G. Natural history of infraspinatus fatty infiltration in rotator cuff tears. J Shoulder Elbow Surg 2010;19:757-63.
8. Burkhart SS, Barth JR, Richards DP, Zlatkin MB, Larsen M. Arthroscopic repair of massive rotator cuff tears with stage 3 and 4 fatty degeneration. Arthroscopy 2007;23:347-54.
9. Ellman H, Hanker G, Bayer M. Repair of the rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg Am 1986;68:1136-44.
10. Ide J, Takagi K. Early and long-term results of arthroscopic treatment for shoulder stiffness. J Shoulder Elbow Surg 2004;13:174-9.
11. Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res 1990;254:92-6.
12. Ide J, Tokiyoshi A, Hirose J, Mizuta H. Classification of full-thickness tears of the subscapularis. Katakansetsu2008;32:433-5.
13. Mihata T, Lee TQ, Watanabe C, Fukunishi K, Ohue M, Tsujimura T, et al.Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy 2013;29:459-70.
14. Mihata T, McGarry MH, Kahn T, Goldberg I, Neo M, Lee TQ, et al. Biomechanical role of capsular continuity in superior capsule reconstruction for irreparable tears of the supraspinatus tendon. Am J Sports Med 2016;44:1423-30.
15. Simonich SD, Wright TW. Terrible triad of the shoulder. J Shoulder Elbow Surg 2003;12:566-8.
 |
 |
 |
 |
| Dr. Furuya Kanji | Dr. Nishinaka Naoya | Dr. Uehara Taishi | Dr. Tsutsui Hiroaki |
| How to Cite This Article: Kanji F, Naoya N, Taishi U, Hiroaki T. Arthroscopic Superior Capsule Reconstruction for Irreparable Rotator Cuff Tear and Axillary Nerve Palsy Associated with Anterior Dislocation of the Shoulder. Journal of Orthopaedic Case Reports 2018. Mar- Apr; 8(2): 100-103. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




