[box type=”bio”] Learning Point for the Article: [/box]
We should be prepared to manage such type of periprosthetic fractures in future with increasing number of knee arthroplasties.
Case Report | Volume 8 | Issue 3 | JOCR May – June 2018 | Page 74-76| Neelam Ramana Reddy, Abhishek Bhalotia, Rajesh Podili. DOI: 10.13107/jocr.2250-0685.1118
Authors: Neelam Ramana Reddy[1], Abhishek Bhalotia[1], Rajesh Podili[1]
[1]Department of Orthopaedics, Star Hospitals, Hyderabad, Telangana, India.
Address of Correspondence:
Dr. Abhishek P Bhalotia,
Star Hospitals, Road no. 10, Banjara Hills, Hyderabad, Telangana, India.
E-mail: dr.abhishekbhalotia@gmail.com
Abstract
Introduction: Incidence of periprosthetic fractures is increasing with the rising number of total knee arthroplasties performed every year. The management of such fractures is challenging due to multiple factors. We reported a rare case with simultaneous bilateral distal femur and tibia periprosthetic fractures managed with open reduction and internal fixation (ORIF) and healed uneventfully.
Case Report: A 64-year-old female came with simultaneous bilateral distal femur (Bilateral Type IIB Rorabeck) and tibia (Bilateral Type IIIB Felix) periprosthetic fractures following road traffic accident. All fractures were managed with ORIF using locking plates. Bony union achieved in 4thpost-operative month without any complication.
Discussion: Management of such fractures can be challenging for orthopedic surgeons due to elderly patients with osteoporotic bone and poor healing potential. This injury is not reported in the literature previously and is quite challenging. At 1-year follow-up, the patient is walking comfortably without support and knee flexion range from 0 to 110° on both sides.
Conclusion: The presentation of such injuries will be increasing in future, and we should be prepared to overcome this challenge. We have managed this case with basic principles of orthopedics, and it healed without any complication.
Keywords: Periprosthetic fracture, total knee arthroplasty.
Introduction
Incidence of periprosthetic fracture following total knee arthroplasty (TKA) is gradually increasing, and management of such fractures can be challenging for orthopedic surgeons due to elderly patients with osteoporotic bone and poor healing potential [1]. The incidence ranges in the literature from 0.3% to 4.2% for primary TKA and from 1.6%to 38% for revisions [2]. Management options of such fractures vary from conservative management, open reduction internal fixation to revision arthroplasty. Management depends on the condition of the knee prosthesis (loose or well fixed), the fracture morphology, quality of bone, and general condition of the patient. Periprosthetic fractures around the knee can be seen in femur, tibia, and patella following TKA. Osteopenia, advanced age, chronic steroid use, female gender, neurological disorders, and stiff knee are the factors that increase the risk of periprosthetic fractures after TKA [3, 4]. The goal of treatment in these fractures is to achieve a painless and stable knee without significant residual malalignment. We present a patient with simultaneous bilateral distal femur and bilateral tibia periprosthetic fractures who was successfully treated with locking plates. Till date, with bilateral distal femur and bilateral tibia periprosthetic fractures is not reported in the literature and signify a management challenge.
Case Report
A 64-year-old female operated with bilateral primary TKA 3 years back came with ssimultaneous bilateral distal femur (Bilateral Type IIB Rorabeck) and tibia (Bilateral Type IIIB Felix) periprosthetic fractures following road traffic accident. The patient was admitted and evaluated with radiographs for further management. 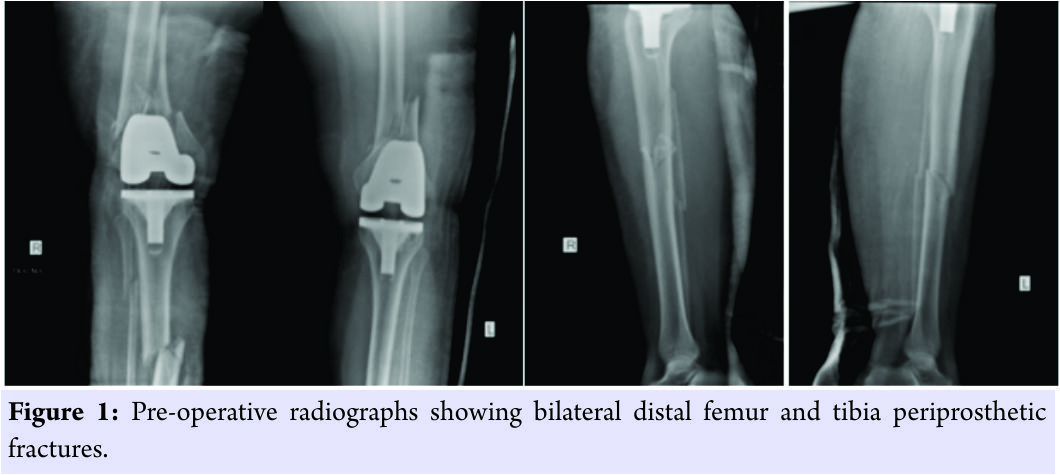 She is a known case of systemic hypertension under treatment and control. After necessary fitness, the patient was operated on both sides in two stages, at a time one limb was operated using swashbuckler approach for distal femur and anterolateral approach for tibia using locking plates due to osteoporosis. Bone graft was not required based on intraoperative findings and lack of comminution. Patient was given routine antibiotic and DVT prophylaxis and was mobilized from the 1stpost-operative day with static quadriceps and passive range of motion exercises. Calcium and Vitamin D3 supplementation given postoperatively and bisphosphonates were not considered. For the 1st6 weeks, the patient was non-weight-bearing following which weight-bearing as tolerated advised, at the end of 3 months as the radiographs show signs of healing patient was advised full weight-bearing. Bony union achieved in 4th post-operative month without any complication.
She is a known case of systemic hypertension under treatment and control. After necessary fitness, the patient was operated on both sides in two stages, at a time one limb was operated using swashbuckler approach for distal femur and anterolateral approach for tibia using locking plates due to osteoporosis. Bone graft was not required based on intraoperative findings and lack of comminution. Patient was given routine antibiotic and DVT prophylaxis and was mobilized from the 1stpost-operative day with static quadriceps and passive range of motion exercises. Calcium and Vitamin D3 supplementation given postoperatively and bisphosphonates were not considered. For the 1st6 weeks, the patient was non-weight-bearing following which weight-bearing as tolerated advised, at the end of 3 months as the radiographs show signs of healing patient was advised full weight-bearing. Bony union achieved in 4th post-operative month without any complication.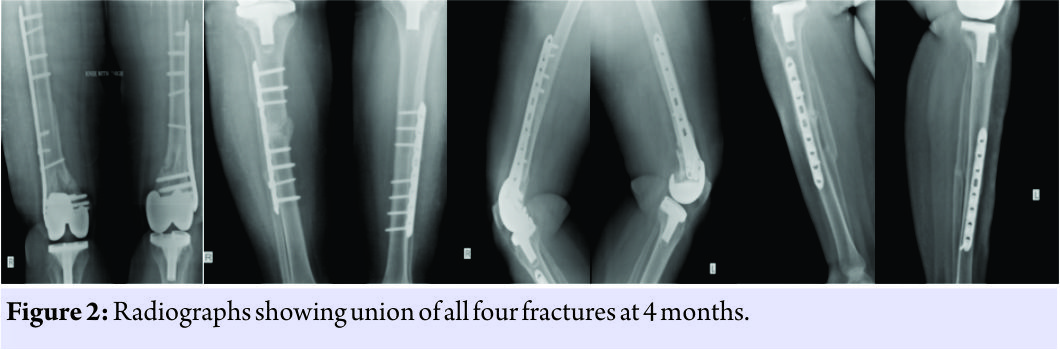
Discussion
The management of periprosthetic fracture is a challenge in terms of planning, recovery, and rate of complications. With few studies in the literature, non-union ranges from 9% to 20%; infection, from3% to 9%; loss of the reduction, from 4% to 27%; and the incidence of reoperations is around 13% [8, 9]. The choice of the treatment should be based on the patient’s age, the fracture displacement and morphology, bone quality, general health, and the status of the prosthetic components (loose, unstable, or misaligned). Currently, operative treatment has been shown to provide better results as a treatment for displaced fractures [3]. Moran et al. studied 29 distal femur periprosthetic fractures treated in three different groups and recommended closed treatment for non-displaced fractures and early open reduction and internal fixation for displaced fractures [10]. For type I and II distal femur fractures, there are two fixation options: Retrograde intramedullary nail and locking plates. Kregor et al. utilized less invasive stabilization system (LISS) in distal femur periprosthetic fractures and found improved maintenance of reduction, less infection rates, and reduced need of bone graft [11]. Althausen et al. compared different methods for the treatment of distal femur periprosthetic fractures and found LISS superior over others[12]. Ricci et al. studied locked plates using minimal invasive technique for distal femur periprosthetic fractures and found satisfactory results in non-diabetic patients and increased wound complications in diabetic patients [13]. Raab and Davis et al. studied locking condylar plates for distal femur periprosthetic fractures and found reliable healing and permit early motion in complex fractures [14]. Carvalho et al. reported a case of bilateral periprosthetic fracture of the distal femur following high-velocity injury treated with retrograde nail, which helped in the preservation of fracture hematoma in osteopenic patient, achieve stability, and recovering the patients functional status[15]. However, in our case, the distal fragment was small and the prosthesis did not allow using this modality. Locked plating permits stable fixation and early knee motion with minimal complications. Locking plates have been extremely useful for these injuries. Periprosthetic tibial fractures after TKA are rarely seen. In Mayo Clinic series, periprosthetic tibial fractures after TKA were observed 0.1% intraoperatively and 0.4% postoperatively [16]. We have managed tibia fracture in our case using locking compression plate as bone was osteoporotic and nailing could not be done with prosthesis in situ.
Conclusion
The incidence of periprosthetic fractures will be increasing with the rising numbers of knee arthroplasty and poor bone quality. We have managed a rare and challenging injury with basic principles of orthopedics, and it healed without any complication. Hence, we should be prepared for such injuries in the future and to overcome the challenges associated with it.
Clinical Message
Management of periprosthetic fractures ischallenging due to fracture pattern and osteoporosis. Bilateral simultaneous distal femur and tibia periprosthetic fractures are uncommon,but with increasing number of arthroplasty, we should be well prepared to manage them.
References
1. Parvizi J, Jain N, Schmidt AH. Periprosthetic knee fractures. J Orthop Trauma 2008;22:663-71.
2. Meek RM, Norwood T, Smith R, Brenkel IJ, Howie CR. The risk of peri-prosthetic fracture after primary and revision total hip and knee replacement. J Bone Joint Surg Br 2011;93:96-101.
3. Johnston AT, Tsiridis E, Eyres KS, Toms AD. Periprosthetic fractures in the distal femur following total knee replacement: A review and guide to management. Knee 2012;19:156-62.
4. Maestro A, Rodriguez L, Lopis JA. Periprosthetic knee fractures. Rev Ortop Traumatol Ed Lat Am 2008; 52:179-87.
5. Hirsh DM, Bhalla S, Roffman M. Supracondylar fracture of the femur following total knee replacement. Report of four cases. J Bone Joint Surg Am 1981;63:162-3.
6. Berry DJ. Epidemiology: Hip and knee. Orthop Clin North Am 1999;30:183-90.
7. Ritter MA, Thong AE, Keating EM, Faris PM, Meding JB, Berend ME, et al. The effect of femoral notching during total knee arthroplasty on the prevalence of postoperative femoral fractures and on clinical outcome. J Bone Joint Surg Am 2005;87:2411-4.
8. Herrera DA, Kregor PJ, Cole PA, Levy BA, Jönsson A, Zlowodzki M, et al. Treatment of acute distal femur fractures above a total knee arthroplasty: Systematic review of 415 cases (1981-2006). Acta Orthop 2008;79:22-7.
9. Platzer P, Schuster R, Aldrian S, Prosquill S, Krumboeck A, Zehetgruber I, et al. Management and outcome of periprosthetic fractures after total knee arthroplasty. J Trauma 2010;68:1464-70.
10. Moran MC, Brick GW, Sledge CB, Dysart SH, Chien EP. Supracondylar femoral fracture following total knee arthroplasty. Clin Orthop Relat Res 1996;324:196-209.
11. Kregor PJ, Hughes JL, Cole PA. Fixation of distal femoral fractures above total knee arthroplasty utilizing the less invasive stabilization system (L.I.S.S.). Injury 2001;32 Suppl 3:SC64-75.
12. Althausen PL, Lee MA, Finkemeier CG, Meehan JP, Rodrigo JJ. Operative stabilization of supracondylar femur fractures above total knee arthroplasty: A comparison of four treatment methods. J Arthroplasty 2003;18:834-9.
13. Ricci WM, Loftus T, Cox C, Borrelli J. Locked plates combined with minimally invasive insertion technique for the treatment of periprosthetic supracondylar femur fractures above a total knee arthroplasty. J Orthop Trauma 2006;20:190-6.
14. Raab GE, Davis CM 3rd. Early healing with locked condylar plating of periprosthetic fractures around the knee. J Arthroplasty 2005;20:984-9.
15. Carvalho M, Fonseca R, Simões P, Bahute A, Mendonça A, Fonseca F, et al. Bilateral distal femoral nailing in a rare symmetrical periprosthetic knee fracture. Case Rep Orthop 2014;2014:745083.
16. Felix NA, Stuart MJ, Hanssen AD. Periprosthetic fractures of the tibia associated with total knee arthroplasty. Clin Orthop Relat Res 1997;345:113-24.
 |
 |
 |
| Dr. Neelam Ramana Reddy | Dr. Abhishek Bhalotia | Dr. Rajesh Podili |
| How to Cite This Article: Reddy N R, Bhalotia A, Podili R. Simultaneous Bilateral Distal Femur and Tibia Periprosthetic Fractures after Total Knee Arthroplasty: A Rare Case Report. Journal of Orthopaedic Case Reports 2018. May- June; 8(3): 74-76. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




