[box type=”bio”] Learning Point for the Article: [/box]
Primary cutaneous leiomyosarcoma of the skin is extremely uncommon and accounts for about 2–3% of all superficial soft tissue sarcoma which tends to occur in lower limb having greater predilection for extensor surfaces. Diagnostic accuracy in discriminating benign from malignant soft tissue masses is considerably increased when morphological MRI features and signal characteristics of the lesion are supplemented by magnetic resonance spectroscopy and diffusion-weighted imaging.
Case Report | Volume 8 | Issue 4 | JOCR July – August 2018 | Page 7-10| Vandana V. Ahluwalia, Pratish Kumar Singh, Hari Singh, Sunanda Samanta. DOI: 10.13107/jocr.2250-0685.1134
Authors: Vandana V. Ahluwalia[1], Pratish Kumar Singh[1], Hari Singh[1], Sunanda Samanta[1]
[1]Department of Radiodiagnosis, Sarojini Naidu Medical College, Agra, Uttar Pradesh, India.
Address of Correspondence:
Dr. Pratish Kumar Singh,
Department of Radiodiagnosis, Sarojini Naidu Medical College, Moti Katra, Agra – 282 002, Uttar Pradesh, India.
E-mail: pratish.singh20@gmail.com
Abstract
Introduction: Primary cutaneous leiomyosarcoma of the skin is extremely uncommon superficial soft tissue sarcoma. The uniqueness of this case is the exceedingly rarity of the tumor and its potential to be clinically misdiagnosed as squamous cell carcinoma. We report an interesting and rare case of PCL with unusual clinical presentation.
Case Report: Our case documents the radiological approach and importance of newer magnetic resonance imaging sequences in helping the diagnosis of a rare case of primary en plaque cutaneous leiomyosarcoma of lower extremity in a 60-year-old male, farmer by occupation with superficial ulceration and local invasion presenting as chronic non-healing ulcerative lesion.
Conclusion: Contrast-enhanced MRI when coupled with advanced imaging sequence such as magnetic resonance spectroscopy and diffusion-weighted imaging further increases malignant probability of the lesion and guides the surgeon for a definite treatment plan.
Keywords: Primary cutaneous leiomyosarcoma, soft tissue sarcoma, advanced magnetic resonance imaging sequences, diffusion-weighted imaging, magnetic resonance spectroscopy.
Introduction
Leiomyosarcomas are rare aggressive smooth muscle malignant tumors representing 5–10% of all soft tissue tumors [1]. Primary cutaneous leiomyosarcoma (PCL) of the skin is extremely uncommon and accounts for about 2–3% of all superficial soft tissue sarcoma [2, 3]. It most commonly occurs in 50–70 years male population; however, it can be seen in any age and sex group. This tumor tends to occur in lower limb having greater predilection for extensor surfaces. Physical trauma and sun exposure are most commonly correlated predisposing factor, but exact cause is unknown. PCLs are subdivided into superficial dermal type and deep subcutaneous type originating from arrector pili muscle and vascular wall smooth muscle, respectively, with former being more common [4]. The role of magnetic resonance imaging (MRI) in characterization of various musculoskeletal masses is well documented due to its excellent soft tissue contrast resolution and inherent multiplanar capabilities. Magnetic resonance spectroscopy (MRS) mirrors the predominant chemical composition within imaged voxel of the lesion, thereby supplements conventional MRI in tumor characterization. The role of MRS in brain imaging has been studied extensively, but its role in musculoskeletal imaging is still in its nascent stage. Due to its inherent property to quantify random Brownian motion of water molecules within imaged tissue voxel, diffusion-weighted imaging (DWI) displays high signal in high cellular tissue.
Case Report
A 60-year-old patient, farmer by occupation presented with solitary chronic non-healing giant ulcer in flexor aspect of mid leg exhibiting irregular margin and punctate bleeding areas in the floor. Bloody discharge was evident at the time of examination(Fig. 1). According to the patient, the ulcer had gradually increased in size and depth for 1 year accompanied by pain and offensive smell for which the patient had received no medical or surgical treatment till now. The patient recalled no history of trauma, which might have gone unnoticed as occupational hazard. 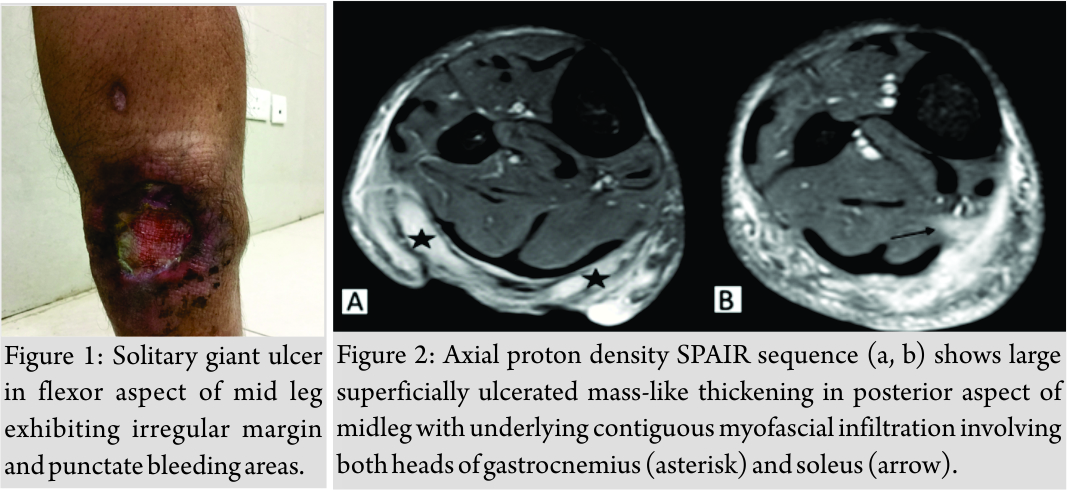 He was a chronic beedi (thin cigarette) smoker but not a drug user. There was no history of diabetes mellitus, hypertension, and tuberculosis. He could not remember any other significant medical history. His hemogram, complete blood count, liver, and kidney function tests were unremarkable. Systemic examinations of the cardiovascular, respiratory, and central nervous systems were within normal limits. Human immunodeficiency virus and hepatitis B surface antigen were non-reactive. There was no palpable inguinal lymphadenopathy. Contrast-enhanced MRI revealed a large superficially ulcerated mass-like thickening in posterior aspect of mid leg measuring approximately 8.5 cm (CC) × 3.5 cm (TR) × 1.6 cm (AP) (Fig. 2). The lesion shows intermediate to low signal intensity on T1-weighted images and high signal intensity on T2-weighted images. Avid heterogeneous post-contrast enhancement appreciated (Fig. 3).
He was a chronic beedi (thin cigarette) smoker but not a drug user. There was no history of diabetes mellitus, hypertension, and tuberculosis. He could not remember any other significant medical history. His hemogram, complete blood count, liver, and kidney function tests were unremarkable. Systemic examinations of the cardiovascular, respiratory, and central nervous systems were within normal limits. Human immunodeficiency virus and hepatitis B surface antigen were non-reactive. There was no palpable inguinal lymphadenopathy. Contrast-enhanced MRI revealed a large superficially ulcerated mass-like thickening in posterior aspect of mid leg measuring approximately 8.5 cm (CC) × 3.5 cm (TR) × 1.6 cm (AP) (Fig. 2). The lesion shows intermediate to low signal intensity on T1-weighted images and high signal intensity on T2-weighted images. Avid heterogeneous post-contrast enhancement appreciated (Fig. 3). 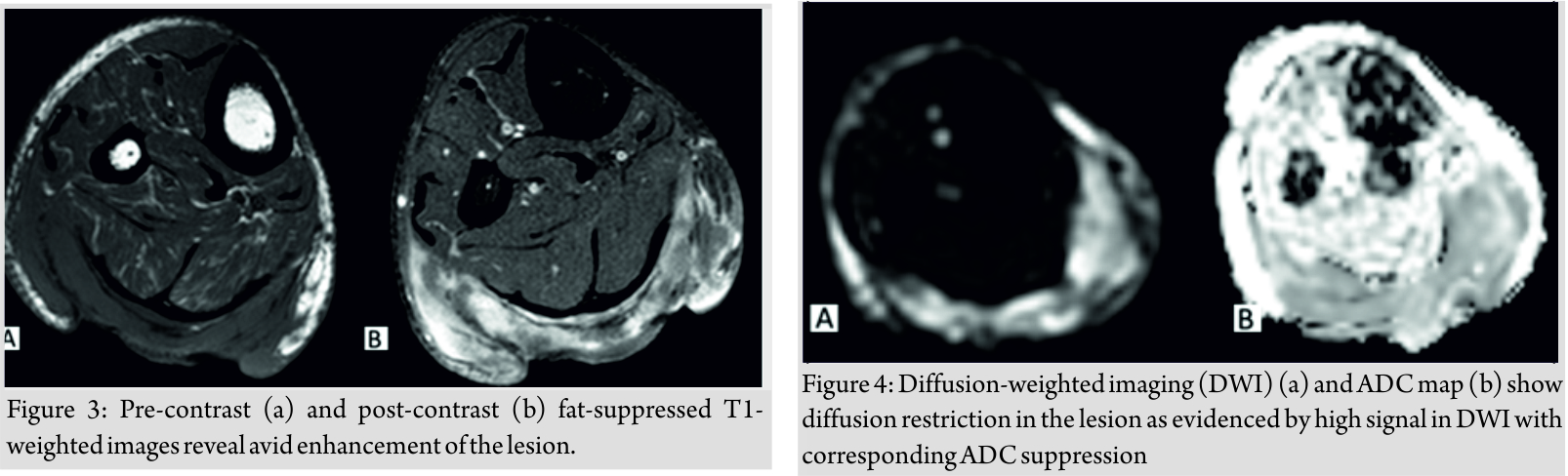 Underlying contiguous myofascial infiltration involving both heads of gastrocnemius including its aponeurosis is observed with their nodular post-contrast enhancement. Furthermore, adjoining infiltration of soleus is noted implied by its post-contrast enhancement. Underlying cortical surface shows neither focal osteolysis nor abnormal marrow signal intensity. Adjoining neurovascular bundles were not involved. The lesion shows diffusion restriction as evidenced by high signal in DWI sequences with corresponding ADC suppression (Fig. 4). Choline peak (3.2 ppm) was noted on multivoxel MRS from solid-enhancing component of the lesion.
Underlying contiguous myofascial infiltration involving both heads of gastrocnemius including its aponeurosis is observed with their nodular post-contrast enhancement. Furthermore, adjoining infiltration of soleus is noted implied by its post-contrast enhancement. Underlying cortical surface shows neither focal osteolysis nor abnormal marrow signal intensity. Adjoining neurovascular bundles were not involved. The lesion shows diffusion restriction as evidenced by high signal in DWI sequences with corresponding ADC suppression (Fig. 4). Choline peak (3.2 ppm) was noted on multivoxel MRS from solid-enhancing component of the lesion.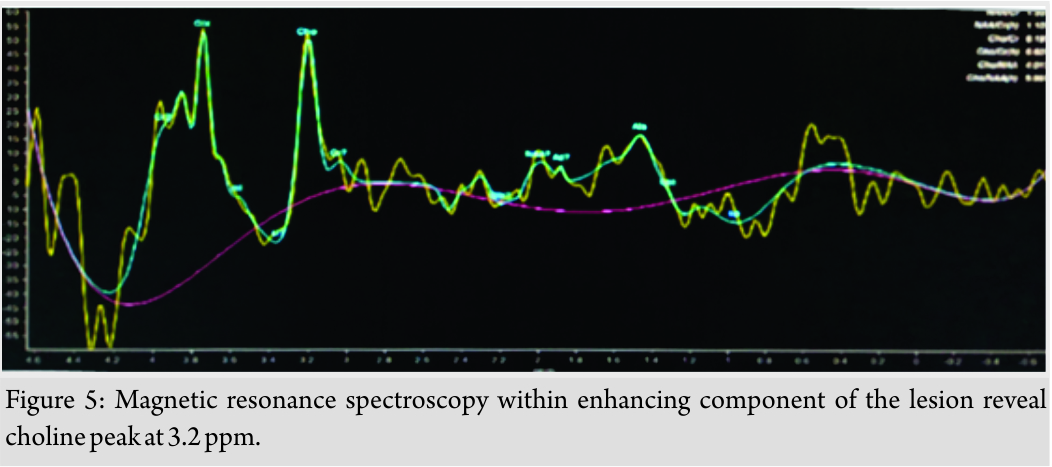
Pathological findings
Examined microscopic sections are revealed dermally located tumor. The tumor cells were spindle shaped, arranged in intersecting fascicles. The nuclei were oval to cigar shaped with eosinophilic cytoplasm. Moderate cellular pleomorphism with frequent mitotic figures was evident.
Immunohistochemistry
The tumor cells were immunoreactive for smooth muscle actin while being negative for CD34 and desmin.
Discussion
Clinical and imaging features of skin and subcutaneous malignancies can be a diagnostic dilemma to clinicians and radiologists alike due to significant overlapping of various entities. Multimodality imaging can increase diagnostic accuracy in most instances. Epithelial malignancies comprising basal cell carcinoma, squamous cell carcinoma, and melanoma represent the most common skin malignancies in descending order [5]. Rest minor group comprises cutaneous and subcutaneous mesenchymal malignancies with cutaneous leiomyosarcoma representing scarce variety. The usual presentation of cutaneous leiomyosarcoma is well-circumscribed nodule in post-trauma or sun-exposed regions [6]. The common dictum in clinical practice is that progressive chronic non-healing ulcerative lesion is regarded as squamous cell carcinoma provided chronic venous ulcer is excluded. Malignant transformations of long-lasting chronic venous ulcers are well documented. There are various instances where primary ulcerating skin carcinomas were misdiagnosed as chronic venous ulcers. Knowledge of this unique clinical and radiological presentation of cutaneous leiomyosarcoma as en plaque chronic progressive infiltrative ulceration is essential in avoiding misdiagnosis, as was the case in our patient. Familiarity about the multimodality imaging features of malignant skin neoplasms is crucial in adequate staging, pre-operative surgical planning, and post-treatment response, although histopathology remains the reference standard for the diagnosis of skin malignancies. Degree of underlying subcutaneous fat and muscle infiltration along with tumor depth is confidently evaluated by MRI due to its inherent multiplanar image capabilities apart from its high spatial and contrast resolution. Contrast-enhanced MRI increases accuracy in degree of local tumor infiltration with detection of non-enhancing internal necrotic component. Diagnostic accuracy in discriminating benign from malignant soft tissue masses is considerably increased when morphological MRI features and signal characteristics of the lesion are supplemented by MRS and DWI. Choline at 3.2 ppm peak is specific marker for malignancy on MRS, whereas high diffusion restriction of the lesion correlates with high cellular content. The use of advanced MRI sequences clears the dilemma of radiologists in differentiating between infective and neoplastic disease processes. The only effective treatment option of PCL is wide local excision, with a 3–5 cm lateral margin [7] and adjuvant radiotherapy or chemotherapy have only limited response [8]. Different studies have reported conflicting local recurrence rates ranging from 14% [9,10] to 42% [11].
Conclusion
Our case presented with atypical clinical and radiological features of rare skin malignancy -PCL. Multiplanar contrast-enhanced MRI is indispensable in local tumor staging and further surgical management. Furthermore, MRS and DWI along with signal intensity and morphological MRI characteristics of the lesion enormously favored its malignant nature.
Clinical Message
Clinical and imaging features of skin and subcutaneous malignancies can be a diagnostic dilemma to clinicians and radiologists alike due to significant overlapping of various entities. Contrast-enhanced MRI, when coupled with advanced imaging sequence such as MRS and DWI further, increases malignant probability of the lesion and guide the surgeon for a definite treatment plan.
References
1. Gustafson P, Willén H, Baldetorp B, Fernö M, Akerman M, Rydholm A, et al. Soft tissue leiomyosarcoma. A population-based epidemiologic and prognostic study of 48 patients, including cellular DNA content. Cancer 1992;70:114-9.
2. Enzinger FM, Weiss SW, Leiomyosarcoma In: Soft Tissue Tumours. 4th ed. St Louis, Missouri: Mosby; 2001. p. 491-8.
3. Weedon D, Williamson RM, Patterson JW. Smooth and skeletal muscle tumours. In: Leboit PF, Gunter B, Weedon D, Sarasin A editors. World Health Organization Classification of Tumours. Pathology and Genetics, Skin tumours. Lyon: IARC; 2006. p. 229-62, 251-2.
4. Angeloni M, Muratori F, Magarelli N, Chalidis BE, Ricci R, Rossi B, et al. Exophytic growth of a neglected giant subcutaneous leiomyosarcoma of the lower extremity. A case report. Int Semin Surg Oncol 2008;5:11.
5. Hong H, Sun J, Cai W. Anatomical and molecular imaging of skin cancer. Clin CosmetInvestig Dermatol 2008;1:1-7.
6. Juan YH, Saboo SS, Tirumani SH, Khandelwal A, Shinagare AB, Ramaiya N, et al. Malignant skin and subcutaneous neoplasms in adults: Multimodality imaging with CT, MRI, and 18F-FDG PET/CT. Am JRoentgenol2014;202:W422-38.
7. Fish FS. Soft tissue sarcomas in dermatology. Dermatol Surg 1996;22:268-73.
8. Fields JP, Helwig EB. Leiomyosarcoma of the skin and subcutaneous tissue. Cancer1981;47:156-69.
9. Jensen ML, Jensen OM, Michalski W, Nielsen OS, Keller J. Intradermal and subcutaneous leiomyosarcoma: A clinicopathological and immunohistochemical study of 41 cases. JCutanPathol1996;23:458-63.
10. Bernstein SC, Roenigk RK. Leiomyosarcoma of the skin. Treatment of 34 cases. Dermatol Surg 1996;22:631-5.
11. Fields JP, Helwig EB. Leiomyosarcoma of the skin and subcutaneous tissue. Cancer1981;47:156-69.
 |
 |
 |
 |
| Dr. Vandana V. Ahluwalia | Dr. Pratish Kumar Singh | Dr. Hari Singh | Dr. Sunanda Samanta |
| How to Cite This Article: Ahluwalia V V, Singh P K, Singh H, Samanta S. Advanced Magnetic Resonance Imaging in the Evaluation of a Chronic Non-healing ulcer – A Case Report of Rare Primary Cutaneous Leiomyosarcoma. Journal of Orthopaedic Case Reports 2018 Jul-Aug; 8(4): 7-10. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




