[box type=”bio”] Learning Point of the Article: [/box]
Aneurysmal bone cyst at rarest site rarest bone can be curable with surgical intervension with adjuvant treatment to prevent recurrence.
Case Report | Volume 9 | Issue 1 | JOCR January – February 2019 | Page 23-27| Sanjay Chhawra, Raman Jain, Rajiv Aggarawal, Ashish Pandey. DOI: 10.13107/jocr.2250-0685.1292
Authors: Sanjay Chhawra[1], Raman Jain[1], Rajiv Aggarawal[1], Ashish Pandey[1]
[1]Department of Orthopaedics, Jaipur Golden Hospital, 2 Institutional Area Sector 3 Rohini, New Delhi–110085, India.
Address of Correspondence:
Dr. Sanjay Chhawra,
A 144 Gayatri Vihar Bagh Mughaliya, Bhopal Madhya Pradesh– 462043, India.
E-mail: sanjaychhawra@yahoo.com
Abstract
Introduction: Aneurysmal bone cysts (ABCs) are benign aggressive bone lesions arising predominantly in the second decade of population in long bones at metaphyseal region which can cause local pain, swelling, and pathologic fracture. With two types, primary and secondary. diagnosis is made with various imaging modalities, although biopsy is important for diagnosis. Currently, the standard treatment is curettage or excision. Along with adjuvant therapy, chemical physical radiotherapy pharmacological to decrease recurrence was more in previous decades.
Case Report: A 40-year-old male presented with the complaint of pain swelling over the right elbow but no fever for the past10days with a history of trauma 15 days back. In the past, history of tuberculosis of the elbow treated 10 years back on antituberculosis therapy, antitubercular drugs, and surgery was done and recovered with satisfactory result. On investigation X-ray – pathological fracture of radial head with eccentric ballooned expanded radiolucency margin well circumscribed lesion bone cyst. Surgery aim was to excise diseased part and get good functional recovery. Wide excision of tumor was done via anterolateral approach with injection of phenol at excised tumor site Tumor bone soft tissues was send for biopsy after surgery .Post-operative recovery was satisfactory with good reasonable range of movement of elbow was achieved
Conclusion: A rare case of primary ABC at epiphyseal region rarest site less common bone involved radius has been reported with no reconstruction done due to it extensive extent with local predisposing factor apart from genetic. ABCs are aggressive benign lesions with high rates of recurrence challenging treatment, but it is curable when approached with multimodality treatment surgical along with radiotherapy pharmacological chemical physical.
Keywords: Aneurysmal bone cyst, Benign bone tumor, Epiphysis, Radius.
Introduction
Dr. Jaffe and Lichenstein described first aneurysmal bone cysts (ABCs) in pelvic and spine lesions in 1942.Non-neoplastic expansile lytic lesion consisting of blood filled spaces separated by connective tissue septa containing bone or osteoid and osteoclast giant cells also known as multilocular hematic cyst or giant cell reparative granuloma accounting1.4 % of all tumors is locally aggressive benign cyst lesion. Aetiology is unknown but develop due to vascular disturbance increase vascular pressure in venous network of bone tumor that result in dilatation of small vessel haemorrhage which causes erosion and resoprtion of bone matrix lead to uncommon expansile osteolytic lesion of bone consisting of a proliferation of vascular tissue that forms a lining around blood filled cystic lesion genetically, ABCs harbor translocation of TRE17/USP6, leading to its transcriptional up regulation. TRE17 encodes a ubiquitin-specific protease and a TBC domain that mediates binding to the Arf6 GTPase. However, TRE17 over expression contribute to tumor pathogenesis [4]. ABCs are commonly seen in childhood and young adulthood with 90% of lesions which are found before age 30 s decades of life. ABC is more common in female with a male:female sex ratio of 1:1.16.ABCs are more common in metaphysis of long bones 67% (femur tibia fibula upper extremity) pelvis 9% Spine 15% posterior element. Also seen in clavicle, foot, and fingers[5].ABCs are mostly solitary and are currently thought to arise either as a primary neoplasm 70% genetic as cause or secondary lesions 30% arising secondary to Osteoblastomas, Chondroblastoma’s, or Giant cell tumors(GCT) Osteosarcoma chondromyxoid fibroma, non-ossifying fibromas, or fibrous dysplasia[6]. These secondary ABCs account for nearly 30% of all ABCs, and they are not considered a neoplasm because no known translocation or genetic aberrancy is present [7]. Differential diagnosis of ABC are unicameral bone cyst GCT osteoblastoma telangiectatic osteosarcoma chondromyxoid fibroma. Clinically, patients present with pain due to the destruction of bone and pathological fracture # swelling at the involved extremity. In the spine, backache and neurological deficit may present and clinically present as (a) inactive,(b) active, and (c) aggressive types[8].Radiograph radiolucent lesion with expanded cortex arising in medullary canal of metaphysis aneurysmal expanded appearance of cortex is contained by periosteum and thin shell of bone marked cortical thinning and erosion with periosteal elevation. This lesion rarely penetrates the articular surface or growth plate; computed tomography (CT) scan look for fluid-fluid level(blood/serum CT scan shows a cystic lesion with intraosseous and extraosseous extend of lesion). Cortical thinning and multiple septal like structures were noted and not appreciated on the radiograph. Bone scan shows intense uptake in the margin of the lesion, with normal background or decreased uptake in its center. Magnetic resonance images (MRI)bright on T2 and fat suppression and intermediate or low signal on T1 double density fluid level, and septation are also suggestive of ABC expansile lytic eccentric septated lesion containing characteristic fluid-fluid level[9, 10]. Histopathology pathology lesion is formed by a thin shell of bone enclosing cystic blood-filled space with friable mass. Microbiology – spongy bone/marrow replaced by pools of blood enclosed in fibrous-osseous sacs which are filled fibroblast, multinucleated osteoclast type gaint cells and reactive woven bone rimmed by osteoblasts 30% cases have bone basophilic called blue bone[11] . Treatment gold standard is open surgery, resulting in good local control excision or curettage with local adjuvant treatment with some complication rate. Non-invasive methods such as embolization. Radiotherapy has also been used, but a major concern is the risk for secondary malignancies. More recently, the use of sclerotherapy has proved an easy and safe method which is associated with good local control and few side effects. Recently, medical treatments, denosumab, block the osteolytic pathway, which has given very promising result. Curettage and bone grafting with adjuvant therapy to decrease recurrence are the main stay of treatment. Curettage can be aggressive, and excision can be marginal or wide with or without bone grafting is preferable treatment. Curettage is associated with an acceptable rate of local control[12,13].Adjuvant treatment is chemical-physical radiotherapy pharmacological to decrease recurrence phenol, cryosurgery, arterial embolization, argon beam coagulation, polymethylmethacrylate (PMMA), liquid nitrogen, sclerotherapy, and high-speed burrmedical treatment – denosumab bisphosphonate doxycycline. Overall recurrence 5–35% in young average time before recurrence was 18.7 months[14]. En bloc excision, or complete resection, is surgical procedure with high morbidity with the lowest rates of recurrence which is subperiosteal resection of lesion. Cement following curettage, bone graft reconstruction is commonly done to promote osseous healing of the resultant cavity[15]. PMMA cement in pediatric benign bone lesions provides immediate stabilization for the resultant cavity, and it exothermic effect helps in reducing recurrence after cement hardens. Highspeed burr is done to augment curettage by mechanical disruption of the lesion [16]. Phenol carbolic acid helps by sterilizing or washing the lesion, removing remaining neoplastic cells following curettage. Selective arterial embolization N 2-butylcyanoacrylate can be used as an adjunct to surgery, but it has also been employed as a primary treatment in ABC lesions that are difficult to access (i.e., pelvis and sacrum) or are at considerable risk for hemorrhage. Sclerotherapy acts by damaging the endothelium of vessels, triggering the coagulation cascade, and resulting in thrombosis. By inducing sclerosis of the ABC vascular network, local control of the lesion can be achieved. (a) Polidocanalinjection sclerorant,(b) doxycylineinjection, and (c)Ethiblocareradiopaque alcoholic solutions that cause local fibrogenic and thrombogenic effects on contact with ABCs which havegoodresult[17,18]. Cryosurgery is the use of liquid or aerosolized nitrogen to generate freezing temperatures that have a cytotoxic effect on the ABC lesion following curettage. Radiotherapy consists of external beam radiation to induce cellular death as an adjuvant therapy in cases of recurrence, and in inoperable ABC lesions, it is emerging treatment for lesion that is not amenable to other treatment but adverse side effects [19]. Radionuclide ablation involves the intralesional injection of radioisotopes, which emit ionizing radiation that ablate adjacent tissue. Argon beam coagulation produces a unipolar electrical current through tissue to induce desiccation and coagulation. Directing argon beam therapy at an ABC lesion following curettage has been shown to reduce recurrence rates[20]. Pharmacological treatment is very effective in tumor. In bone cell receptor-activator of nuclear kappa B ligand (RANKL) signalling pathway is mediator in bone homeostasis by promoting osteoclast activation, bone resorption and remodelling. In various benign and malignant bone neoplasms, the role of RANKL expression is there [21].ABCs have higher than normal levels of RANKL expression. RANKL signaling is inhibited by denosumab in which a human monoclonal antibody is used in osteoporosis, GCT of bone, in metastasis and recently has being started in ABC with promising result. Doxycycline is an antibiotic inhibition of matrix metalloproteinase angiogenesis and anti-neoplastic properties play a role in inhibiting ABC expansion within bone[22]. Bisphosphonates are pyrophosphate analogs that inhibit osteoclast-mediated bone resorption with antineoplastic characteristics possibly by inducing apoptosis, inhibiting tumor cell adhesion and invasion by inhibiting angiogenesis so help in pain relief. So both drugs doxycycline Bisphosphonates used in ABC [23, 24, 25].
Case Report
A 40-year-oldmale presented with the complaint of pain swelling over the right elbow but no fever for the past 10 days with a history of trauma 15 days back. In the past, a history of tuberculosis (TB) of elbow treated 10 years back on antituberculosis therapy, antituberculardrugs, and surgery synovectomy debridement of elbow joint through lateral approach later patient recovered well with satisfactory result. On physical examination, there was tenderness over lateral aspect of the elbow with restricted movement of elbow and wasting of forearm muscle. Swelling over elbow with no sign of inflammation or infection skin was normal. On investigation X-ray – pathological fracture of Radial head with eccentric ballooned expanded Radiolucency margin well circumscribed lesion Bone cyst (Fig. 1). MRI – mildly expansile lesion at proximally epiphysis-metaphysis adjacent to diaphyseal location of radius extending upto sub articular location abutting articular cartilage. Surgery was planned; the aim was to excise diseased part and get good functional recovery wide excision of tumor through anterolateral approach with injection of phenol (Fig. 2).  Tumor bone soft tissues send for biopsy including Radial head which was involved up to articular cartilages, (Fig. 3)Radial head reconstruction was not done because ABC extended from metaphysic – diaphysis junction to epiphysis cartilage of radial head. Post-operative recovery was satisfactory with good reasonable range of movement of the elbow (Fig. 4).
Tumor bone soft tissues send for biopsy including Radial head which was involved up to articular cartilages, (Fig. 3)Radial head reconstruction was not done because ABC extended from metaphysic – diaphysis junction to epiphysis cartilage of radial head. Post-operative recovery was satisfactory with good reasonable range of movement of the elbow (Fig. 4).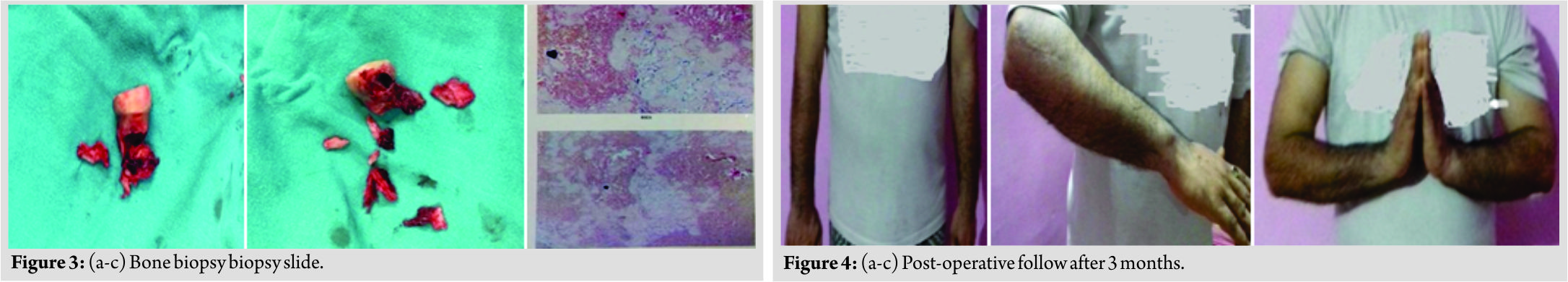
Discussion
This case is reported with rarity in percentage and rarity in the location of site and bone. The epiphyseal ABC is rare to present with location over proximal radius head which is only 3%. The ABC common site presentation is long bones humerus femur tibia with location over metaphyseal region here in this case epiphyseal location rare to see. In this case apart from genetic cause recent trauma and 10 years back, the treated case of TB elbow may be predisposing factor which is something unusual different. The treatment of ABC is surgery curettage – excision, reconstruction and adjuvant procedure to prevent recurrence such as liquid nitrogen, phenol or PMMA injection at the site of tumor arterial embolization. Recent denosumab injection therapy had decreased recurrence of tumor. In this case, wide excision done with phenol injection was given, but no reconstruction was done due to epiphyseal radial head involvement and its extension to metaphyseal region reconstruction not done to prevent recurrence. Post-operative patient gained a reasonable range of movement with stability. Recurrence is 10–60% which is observed more in young children if surgery is done alone curettage with no adjuvant treatment. Hence, now, treatment protocol is surgical excision with various adjuvant treatments to prevent recurrence with minimum complication and morbidity.
Conclusion
A rare case of primary ABC at epiphyseal region rarest site less common bone radius is involved has been reported. Surgery has being done to excise tumor without reconstruction of radius head because of it extensive extent with local predisposing factor apart genetic. ABCs are aggressive benign lesions with high rates of recurrence challenging treatment, but it is curable when approached with multimodality treatment surgical along with chemical-physical radiotherapy pharmacological. The standard treatment remains curettage or excision with grafting to fill the bone void, with different adjuvant or alternative treatment methods to reduce recurrence. ABCs in anatomic locations where surgery would cause significant morbidity are most often treated with embolization or radiotherapy, and recently, medical management with denosumab has given a promising result.
Clinical Message
ABC is rare tumor challenging in its presentation in bone with it site percentage and approach of treatment. The mainstay of treatment is surgical excision or curettage with adjuvant treatment chemical-physical radiotherapy pharmacological treatment to prevent recurrence with regular follow-up which gives the best curable result with less complication and morbidity.
References
1. Lichtenstein L. Aneurysmal bone cyst; Further observations. Cancer 1953;6:1228-37.
2. Mankin HJ, Hornicek FJ, Ortiz-Cruz E, Villafuerte J, Gebhardt MC. Aneurysmal bone cyst: A review of 150 patients. J Clin Oncol 2005;23:6756-62.
3. Campanacci M, Cervellati C, Donati U, Bertoni F. Aneurysmal bone cyst (a study of 127 cases, 72 with longterm follow up). Ital J Orthop Traumatol 1976;2:341-53.
4. Lau AW, Pringle LM, Quick L, Riquelme DN, Ye Y, Oliveira AM, et al. TRE17/ubiquitin-specific protease 6 (USP6) oncogene translocated in aneurysmal bone cyst blocks osteoblastic maturation via an autocrine mechanism involving bone morphogenetic protein dysregulation. J Biol Chem 2010;285:37111-20.
5. Leithner A, Windhager R, Lang S, Haas OA, Kainberger F, Kotz R, et al. Aneurysmal bone cyst. A population based epidemiologic study and literature review. Clin Orthop Relat Res 1999;363:176-9.
6. Capanna R, Springfield DS, Biagini R, Ruggieri P, Giunti A. Juxtaepiphyseal aneurysmal bone cyst. Skeletal Radiol 1985;13:21-5.
7. Martinez V, Sissons HA. Aneurysmal bone cyst. A review of 123 cases including primary lesions and those secondary to other bone pathology. Cancer 1988;61:2291-304.
8. Ameli ON, Abbassion K, Saleh H, Eplamdoost A. Aneurysmal bone cysts of the spine. J Neurosurg 1985;63:685-90.
9. Dabska M, Buraczewski J. Aneurysmal bone cyst. Pathology, clinical course and radiologic appearances. Cancer 1969;23:371-89.
10. Beftran J, Simon CD, Levy M, Herman L, Weis L, Mueller FC. Aneurysmal bone cysts: MR. Imaging at 1.5T. J Radiol 1986;158:689-90.
11. Creager AJ, Madden CR, Bergman S, Geisinger KR. Aneurysmal bone cyst: Fine-needle aspiration findings in 23 patients with clinical and radiologic correlation. Am J Clin Pathol 2007;128:740-5.
12. Peeters SP, Van der Geest IC, de Rooy JW, Veth RP, Schreuder HW. Aneurysmal bone cyst: The role of cryosurgery as local adjuvant treatment. J Surg Oncol 2009;100:719-24.
13. Schreuder HW, Veth RP, Pruszczynski M, Lemmens JA, Koops HS, Molenaar WM, et al. Aneurysmal bone cysts treated by curettage, cryotherapy and bone grafting. J Bone Joint Surg Br 1997;79:20-5.
14. Garg S, Mehta S, Dormans JP. Modern surgical treatment of primary aneurysmal bone cyst of the spine in children and adolescents. J Pediatr Orthop 2005;25:387-92.
15. Flont P, Kolacinska-Flont M, Niedzielski K. A comparison of cyst wall curettage and en bloc excision in the treatment of aneurysmal bone cysts. World J Surg Oncol 2013;11:109.
16. Wang EH, Marfori ML, Serrano MV, Rubio DA. Is curettage and high-speed burring sufficient treatment for aneurysmal bone cysts? Clin Orthop Relat Res 2014;472:3483-8.
17. Bitzan P, Windhager R, Lang S, Richling B, Kotz R. Incidence of recurrence of aneurysmal bone cysts following surgical treatment and adjuvant therapy with phenol. Z Orthop Ihre Grenzgeb 1995;133:422-8.
18. Varshney MK, Rastogi S, Khan SA, Trikha V. Is sclerotherapy better than intralesional excision for treating aneurysmal bone cysts? Clin Orthop Relat Res 2010;468:1649-59.
19. Feigenberg SJ, Marcus RB Jr., Zlotecki RA, Scarborough MT, Berrey BH, Enneking WF, et al. Megavoltage radiotherapy for aneurysmal bone cysts. Int J Radiat Oncol Biol Phys 2001;49:1243-7.
20. Steffner RJ, Liao C, Stacy G, Atanda A, Attar S, Avedian R, et al. Factors associated with recurrence of primary aneurysmal bone cysts: Is argon beam coagulation an effective adjuvant treatment? J Bone Joint Surg Am 2011;93:e1221-9.
21. Yamagishi T, Kawashima H, Ogose A, Ariizumi T, Sasaki T, Hatano H, et al. Receptor-activator of nuclear kappaB ligand expression as a new therapeutic target in primary bone tumors. PLoS One 2016;11:e0154680.
22. Fife RS, Rougraff BT, Proctor C, Sledge GW Jr. Inhibition of proliferation and induction of apoptosis by doxycycline in cultured human osteosarcoma cells. J Lab Clin Med 1997;130:530-4.
23. Lange T, Stehling C, Fröhlich B, Klingenhöfer M, Kunkel P, Schneppenheim R, et al.Denosumab: Apotential new and innovative treatment option for aneurysmal bone cysts. Eur Spine J 2013;22:1417-22.
24. Duivenvoorden WC, Hirte HW, Singh G. Use of tetracycline as an inhibitor of matrix metalloproteinase activity secreted by human bone-metastasizing cancer cells. Invasion Metastasis 1997;17:312-22.
25. Morgan G, Lipton A. Antitumor effects and anticancer applications of bisphosphonates. Semin Oncol 2010;37 Suppl 2:S30-40.
 |
 |
 |
 |
| Dr. Sanjay Chhawra | Dr. Raman Jain | Dr. Rajiv Aggarawal | Dr. Ashish Pandey |
| How to Cite This Article: Chhawra S, Jain R, Aggarawal R, Pandey A. A Rare Case of Radius Head Epiphyseal Aneurysmal Bone Cyst with Predisposing Factor as Trauma Tuberculosis of Elbow apart from Genetic. Journal of Orthopaedic Case Reports 2019 Jan-Feb; 9(1): 23-27. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




