[box type=”bio”] Learning Point of the Article: [/box]
Plain radiographs can fail to detect impending soft tissue damage secondary to comminuted calcaneal fractures.
Case Report | Volume 9 | Issue 2 | JOCR March – April 2019 | Page 11-14 | Tarek Taha, Karim Mahmoud, Ahmed Khalil Attia, Maged M Mekhaimar. DOI: 10.13107/jocr.2250-0685.1346
Authors: Tarek Taha[1], Karim Mahmoud[2], Ahmed Khalil Attia[2], Maged M Mekhaimar[2]
[1]Department of Medical Education, Weill Cornell Medicine – Qatar, Doha, Qatar,
[2]Department of Orthopaedic Surgery, Hamad Medical Corporation, Doha, Qatar.
Address of Correspondence:
Dr. Tarek Taha,
Department of Medical Education, Weill Cornell Medicine – Qatar, Qatar Foundation – Education City, P.O. Box 24144, Doha, Qatar.
E-mail: tat2012@qatar-med.cornell.edu
Abstract
Introduction: Calcaneal fracture is the most common foot fracture. It occurs due to an axial load and is associated with high morbidity, especially when the articular surface is involved. There are two types of calcaneal fractures: Joint depression type and tongue type. The latter has a high risk of skin necrosis and should be operated on promptly.
Case Report: This is a 37-year-old Bangladeshi man who sustained a comminuted calcaneal fracture and a Lisfranc fracture of the left foot. Initial radiograph showed a joint depression-type fracture, excluding a surgical emergency. Nevertheless, the patient developed skin necrosis over the posterior aspect of the heal that improved after open reduction and internal fixation of the calcaneus. Pre-operative computed tomography (CT) scan demonstrated a bony fragment that was displaced posteriorly causing the skin necrosis.
Conclusion: X-ray imaging is not sufficient to exclude surgical emergencies with calcaneal fractures. Highly comminuted fractures should be assessed more thoroughly with urgent CT scan.
Keywords: Calcaneus, Fracture, Skin necrosis.
Introduction
Calcaneal fractures are one of the common feet and ankle fractures. They represent 75% of foot fractures [2]. They usually occur after an axial load is exerted on the calcaneus after a fall from height or motor vehicle accident with the foot pressed over the pedal [1]. Due to its complex structure and its three joint facets articulation with the talus and tarsus, fractures of the calcaneus are notorious for difficulty in reduction and subsequent morbidity, especially in intra-articular displaced fractures [2]. In 1952, Essex-Lopresti was able to classify calcaneal fractures using lateral X-ray films into two main categories: Tongue fractures and joint depression type. Both of them share the same primary fracture line but differ in the secondary fracture line which exits to the posterior border of the tuberosity in the former and just behind the joint in the latter as shown in Fig. 1 [3]. This classification has been guiding the management of calcaneal fractures to this day with the majority of fractures being that of the joint depression type. Specifically, tongue-type fracture requires prompt reduction due to the risk of pressure skin necrosis by the superiorly displaced posterior fragment of the calcaneus [4]. This is a case report of secondary skin necrosis due to a calcaneal fracture that does not fall into the typical classification of tuberosity tongue-type fracture on lateral X-ray film.
Case Report
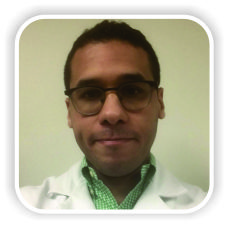
A 37-year-old Bangladeshi male sustained a fall during work. He fell off an 8–10 m high scaffold on his left foot and then on his left side. Subsequently, a heavy object fell on his left foot. He was complaining of severe pain in the left foot and inability to bear weight on it. He was brought by the ambulance to the emergency department. On arrival, the patient was conscious, oriented with Glasgow Coma Scale 15/15. Physical examination showed severe tenderness over the left foot with deformity. Neurovascular status of the foot was intact. There was moderate-to-severe swelling with soft compartments of the left foot. He was cleared by the trauma team and investigation showed isolated left foot comminuted intra-articular calcaneal fracture along with Lisfranc fracture with dislocation of the tarsometatarsal joints. X-ray of the left foot is shown in Fig. 2. 1 day after presentation to the emergency department, the patient under went open reduction and internal fixation (ORIF) of the left foot Lisfranc fracture and dislocation with cortical screws for the first to fourth metatarsal and 2 mm K-wire for the fifth metatarsal. 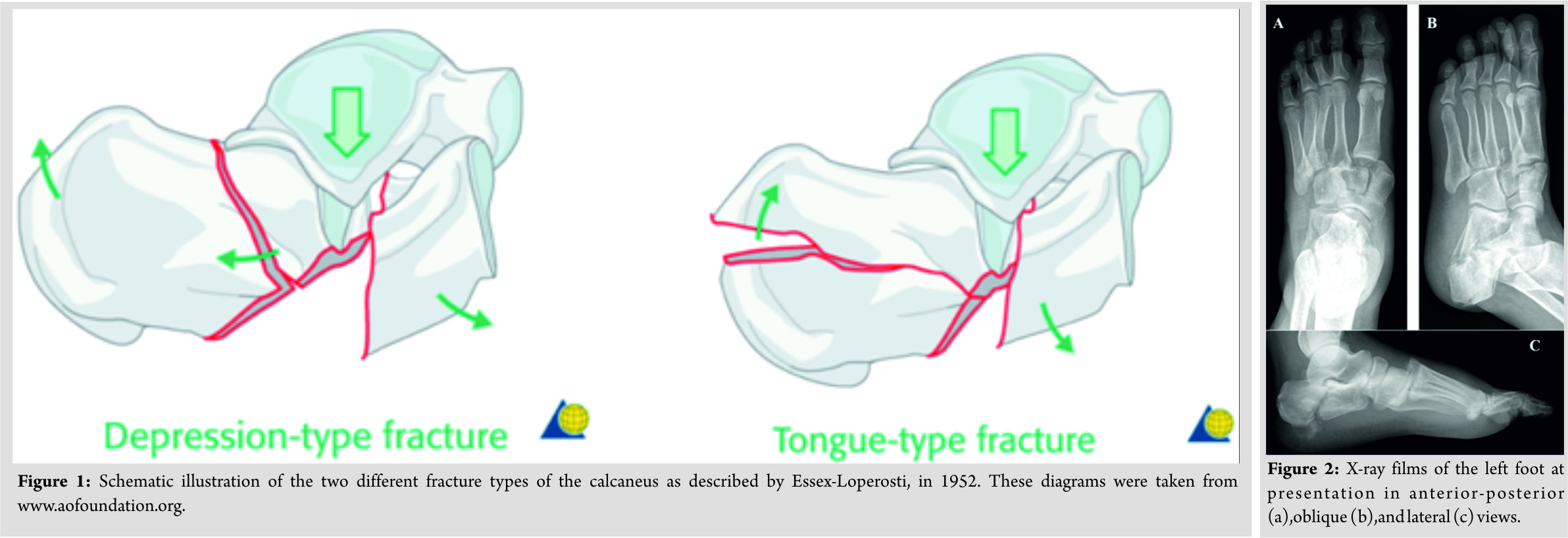 A below the knee back slab was then applied and the patient was admitted to the orthopedics ward. The post-operative course of the patient was unremarkable except for swelling over the left foot. However, on the 4thpost-operative day, the patient developed clear skin blisters over the posterior aspect of the calcaneus. The skin condition of the patient deteriorated to skin necrosis as shown in Fig. 3a. A computed tomography (CT) scan of the left foot was carried out in preparation for ORIF of the calcaneus. Cut sections of the CT scan demonstrating a fragment of the calcaneus pressing over the posterior soft tissue are shown along with other cuts in (Fig. 4).
A below the knee back slab was then applied and the patient was admitted to the orthopedics ward. The post-operative course of the patient was unremarkable except for swelling over the left foot. However, on the 4thpost-operative day, the patient developed clear skin blisters over the posterior aspect of the calcaneus. The skin condition of the patient deteriorated to skin necrosis as shown in Fig. 3a. A computed tomography (CT) scan of the left foot was carried out in preparation for ORIF of the calcaneus. Cut sections of the CT scan demonstrating a fragment of the calcaneus pressing over the posterior soft tissue are shown along with other cuts in (Fig. 4). 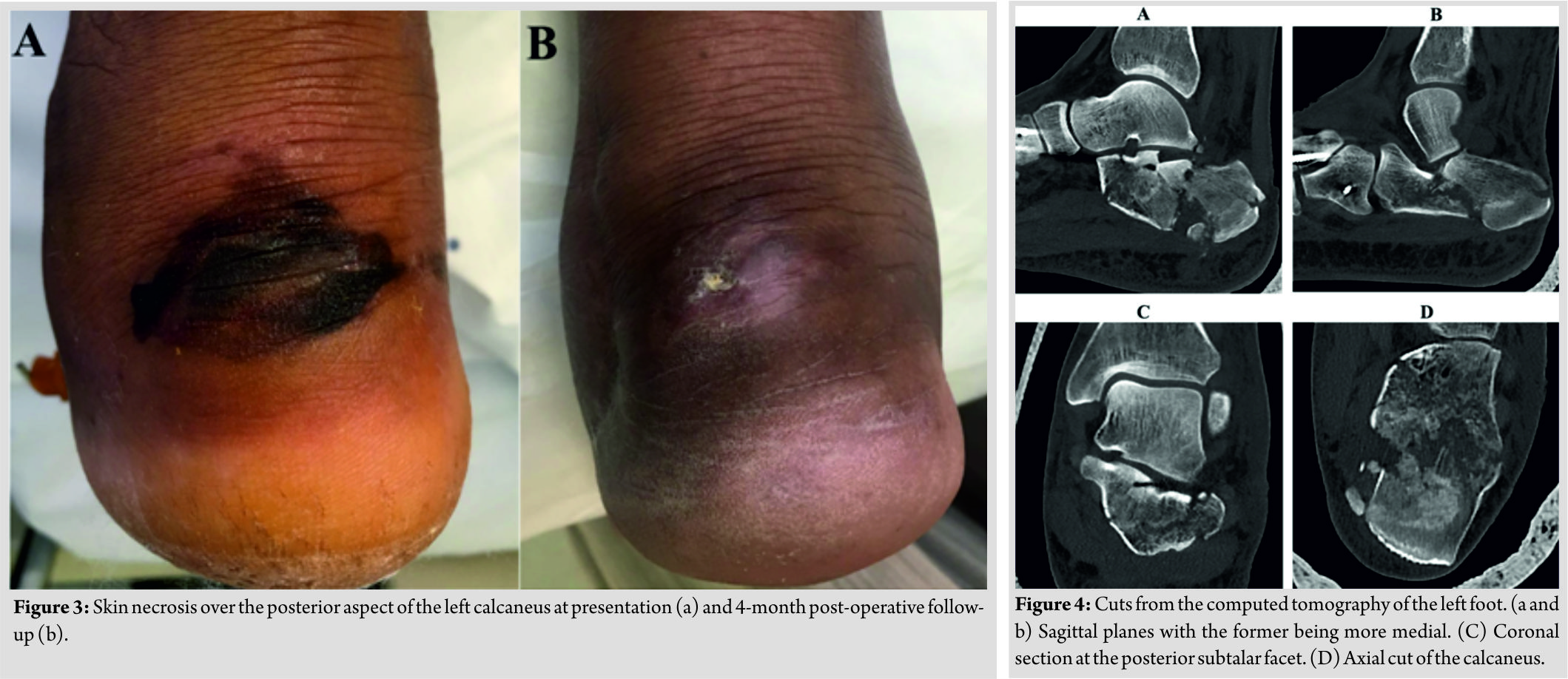 The patient then underwent ORIF utilizing an extended lateral approach. Using a 3.5 mm K-wire inserted posteriorly, the posterior fragment and the articular surface were reduced under fluoroscopy supervision. A medium calcaneal plate was then applied and held in place with screws locking and non-locking. A back slab was applied and the patient was discharged 2days after the operation. Outpatient follow-up 4months postoperatively shows healing skin over the posterior aspect of the calcaneus (Fig. 3b). At 1-year post-operative visit, the patient is back to complete daily activities with mild pain while running. Radiographs of the calcaneus and the Lisfranc fractures showed good fixation and healing (Fig. 5 and 6).
The patient then underwent ORIF utilizing an extended lateral approach. Using a 3.5 mm K-wire inserted posteriorly, the posterior fragment and the articular surface were reduced under fluoroscopy supervision. A medium calcaneal plate was then applied and held in place with screws locking and non-locking. A back slab was applied and the patient was discharged 2days after the operation. Outpatient follow-up 4months postoperatively shows healing skin over the posterior aspect of the calcaneus (Fig. 3b). At 1-year post-operative visit, the patient is back to complete daily activities with mild pain while running. Radiographs of the calcaneus and the Lisfranc fractures showed good fixation and healing (Fig. 5 and 6).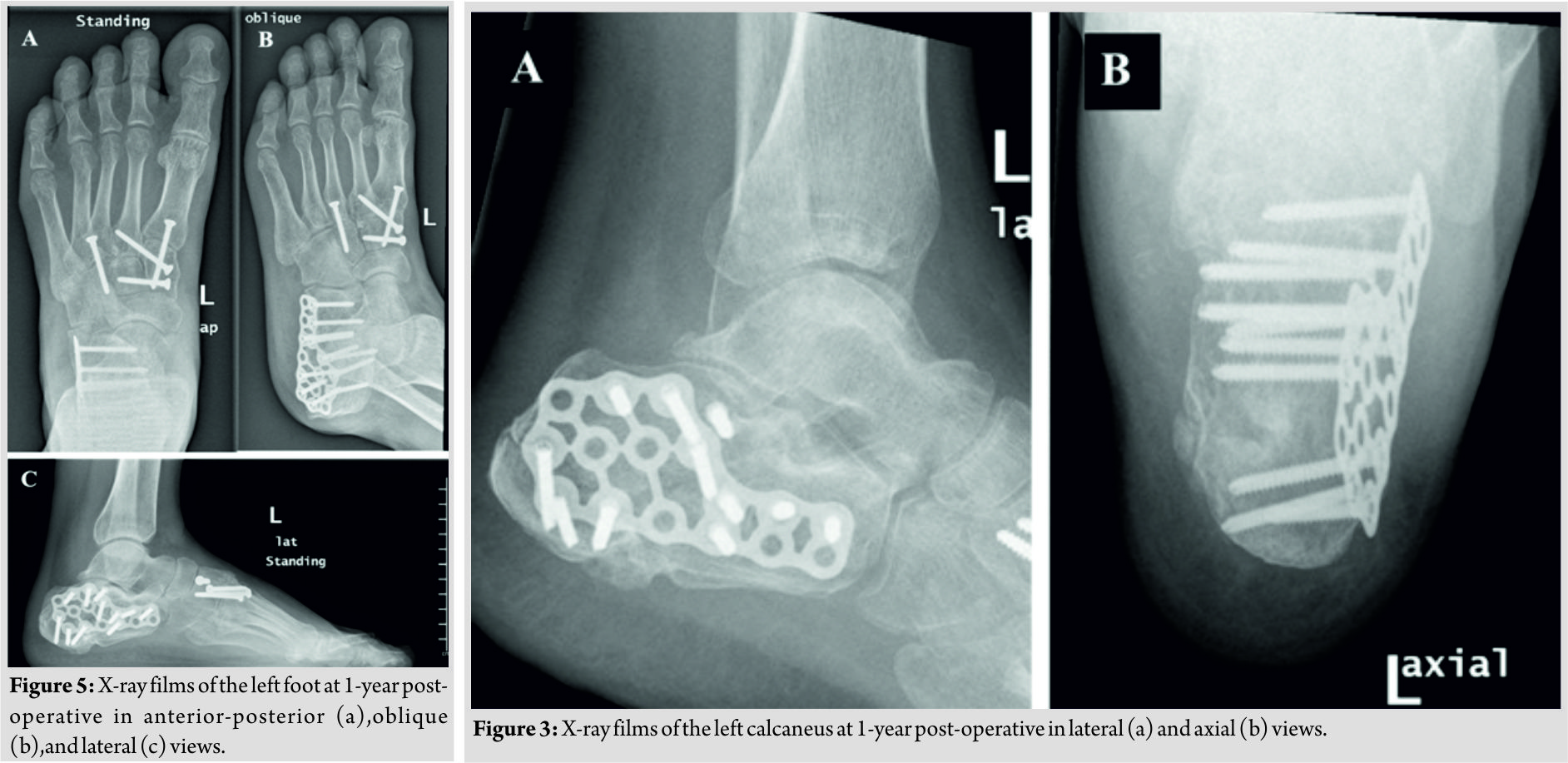
Discussion
In many aspects, this case is similar to the common presentation of a calcaneal fracture. It is caused by an axial load from a fall of height. This axial load is transferred by the lateral process of the talus to the calcaneus which leads to the primary fracture line shown in Fig. 2c dividing the bone to anterior and posterior fragments as described by Essex-Lopresti in his original paper. CT scan shows lateral bulge of the bone due to compression forces and the relatively thin cortex of the calcaneus lateral wall [1]. Moreover, the coronal section of the posterior face of the subtalar joint (Fig. 4c) shows two fracture lines with depressed central fragment which makes this fracture classified as Type IIIAB in Sander’s classification [6]. This makes the prognosis of this patient relatively low and highly depended on the success of achieving anatomical reduction of the articular surface. While this would be considered a joint depression fracture based on lateral X-ray, it was complicated by skin necrosis unexpectedly. On the lateral view radiograph (Fig. 2c), this fracture does not resemble the typical tongue fracture with a visible secondary fracture line exiting to the posterior surface and a superiorly elevated fragment [5]. Therefore, this was treated as a joint depression-type fracture with no eminent threat to the skin overlying the posterior surface of the heal. Nevertheless, a close examination of the sagittal cuts on the CT scan shows that although there is a fracture line exiting behind the posterior subtalar facet (Fig. 4a), there is also another fracture line exiting on the posterior surface of the tuberosity (Fig. 4b). This led to the formation of a posterior fragment abutting the skin and induced skin pressure, leading to necrosis. Soft tissue complications secondary to calcaneal fractures pose a great challenge in management. Even with ORIF, their prevalence was reported to be as high as 20% of cases [11]. There have been many attempts for classification to guide the management of such complications. Management ranges from simple conservative measure as wound debridement and care to more definitive procedures such as flap transfers and below the knee amputations[7,9]. Although there has been dramatic improvement in the management of such secondary soft tissue injuries, the key point of management is careful assessment of the injury through comprehensive history, careful examination, and diagnostic studies to guide management [10]. While in cases like ours prompt surgical intervention was important, in other scenarios, conservative management might be superior in avoiding soft tissue injury. This case shows the importance of a high index of suspicion toward this type of fractures and the insufficiency of lateral view radiograph in excluding threat to the overlying soft tissue. CT is the current gold standard for assessing calcaneal fractures [2] and should be not delayed in cases with suspicion of the risk of delayed necrosis to the skin. Although displaced tuberosity type of calcaneus fractures constitutes a minority of calcaneal fracture, they are more common in high-energy injuries with comminuted fractures [8]. Therefore, we recommend urgent CT scan for fractures associated with high-energy impacts like our case to assess the threat to surrounding soft tissue. We advise to read the CT scan carefully and to be aware that any protruding fragment toward the skin that could cause skin necrosis and should be dealt with urgency as displaced tuberosity fractures.
Conclusion
This is a case report of a comminuted calcaneal fracture due to a fall from height. The fracture is considered a joint depression type on lateral X-ray. Nevertheless, it was complicated with skin necrosis and CT imaging revealed a bone fragment compressing the posterior soft tissue. This highlights the insufficiency of lateral X-ray films in excluding threat to surrounding soft tissues.
Clinical Message
Plain radiographs can fail to detect impending soft tissue damage secondary to comminuted calcaneal fractures. We recommend using emergent CT imaging to assess soft tissue status for any high-energy calcaneal fracture, even if lateral X-ray shows a depression-type fracture.
References
1. Rammelt S, Zwipp H. Calcaneus fractures: Facts, controversies and recent developments. Injury 2004;35:443-61.
2. Razik A, Harris M, Trompeter A. Calcaneal fractures: Where are we now? Strategies Trauma Limb Reconstr 2018;1:1-11.
3. Essex‐Lopresti P. The mechanism, reduction technique, and results in fractures of the oscalcis. Br J Surg 1952;39:395-419.
4. Gardner MJ, Nork SE, Barei DP, Kramer PA, Sangeorzan BJ, Benirschke SK. Secondary soft tissue compromise in tongue-type calcaneus fractures. J Orthop Trauma 2008;22:439-45.
5. Chhabra N, Sherman SC, Szatkowski JP. Tongue-type calcaneus fractures: A threat to skin. Am J Emerg Med 2013;31:1151-e3.
6. Sanders R, Fortin P, DiPasquale T, Walling A. Operative treatment in 120 displaced intraarticular calcaneal fractures results using a prognostic computed tomography scan classification. ClinOrthopRelat Res 1993;290:87-95.
7. Levin LS, Nunley JA. The management of soft-tissue problems associated with calcaneal fractures. ClinOrthopRelat Res 1993;290:151-6.
8. Snoap T, Jaykel M, Williams C, Roberts J. Calcaneus fractures: A possible musculoskeletal emergency. J Emerg Med 2017;52:28-33.
9. Heintzman SE, Lund EA, Bubla JW, Whiting PS. A novel casting technique for tongue-type calcaneus fractures with soft tissue compromise. Foot Ankle Orthop 2017;2:1-6.
10. Watson TS. Soft tissue complications following calcaneal fractures. Foot Ankle Clin 2007;12:107-23.
11. Folk JW, Starr AJ, Early JS. Early wound complications of operative treatment of calcaneus fractures: Analysis of 190 fractures. J Orthop Trauma 1999;13:369-72.
 |
 |
 |
 |
| Dr. Tarek Taha | Dr. Karim Mahmoud | Dr. Ahmed Khalil Attia | Dr. Maged M Mekhaimar |
| How to Cite This Article: Taha T, Mahmoud K, Attia A K, Mekhaimar M M. Delayed Soft Tissue Necrosis in an Atypical Closed Calcaneal Fracture: A Case Report. Journal of Orthopaedic Case Reports 2019 Mar-Apr; 9(2): 11-14. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




