[box type=”bio”] Learning Point of the Article: [/box]
Heterotopic ossification of the Tendoachilles is a rare clinical entity which can be managed conservatively and surgical removal if required gives a good result.
Case Report | Volume 9 | Issue 2 | JOCR March – April 2019 | Page 45-47 | Raju Vaishya, Celestine O Maduka, Amit Kumar Agarwal, Vipul Vijay, Abhishek Vaish. DOI: 10.13107/jocr.2250-0685.1364
Authors: Raju Vaishya[1], Celestine O Maduka[1], Amit Kumar Agarwal[1], Vipul Vijay[1], Abhishek Vaish[1]
[1]Department of Orthopaedics, Indraprastha Apollo Hospitals, Sarita Vihar – 110076, New Delhi, India.
Address of Correspondence:
Dr. Amit Kumar Agarwal,
Consultant Orthopaedic Surgeon, Indraprastha Apollo Hospitals, New Delhi – 110076, India.
E-mail: amitorthopgi@yahoo.co.in
Abstract
Introduction: Heterotopic ossification of tendo Achilles (HOTA) is an uncommon clinical condition with unknown etiology. However, there are noted factors associated with this condition including trauma, metabolic conditions, infections, and genetic predisposition. The diagnosis can be made clinically and radiologically. We are reporting a rare case of HOTA managed surgically.
Case Report: A 48-year-old healthy man with no history of trauma presented with pains and swelling of the posterior aspect of the left ankle and lower calf. The local examination revealed mass about 2 inches above the left ankle. A plain radiograph revealed a bony mass at the left TA region. The magnetic resonance imaging confirmed the presence of a bony mass within the substance of TA. All the clinical and biochemical laboratory tests were within normal limits. The heterotopic bone mass was removed, using a posterior longitudinal incision over the left TA, centering over the bony mass. At 6 months of follow-up, the patient had no pain, swelling, and a full range of ankle movements.
Conclusion: Conservative approach may suffice in most of the patients while surgery is reserved for failed conservative treatment.
Keywords: Tendon Achilles, Heterotopic Ossification, Calcification, Leg, Ankle.
Introduction
Heterotopic ossification of tendo Achilles (HOTA) is a rare clinical condition, with a male predilection[1, 2]. Although the exact cause of this disease is largely unknown, there are clinical conditions that are associated with it. These include trauma which may be accidental or surgical. Moreover, cases of repetitive trauma may have a predisposition to its development. The axial load on the TA is about 4 times and 8 times that of the body weight while standing and walking, respectively. Hence, the tendon is more prone to frequent and recurrent injuries than the other tendons in the body. The ossified mass in the HOTA may fracture in some cases with associated partial or complete rupture of the tendon[3]. Other conditions associated with HOTA include metabolic diseases(e.g.,diabetes mellitus and Wilson disease),infectious diseases (e.g., chronic osteomyelitis, cellulitis, and Reiter’s disease), and genetic predisposition[4, 5]. The diagnosis can be made clinically and radiologically. Treatment is usually conservative, and the surgery is reserved for failed conservative measures. The histology of this disease includes ossification, calcification, or both. We are reporting a case of HOTA, in an adult male.
Case Report
A 48-year-old healthy man with no history of trauma presented with pains and swelling of the posterior aspect of the left ankle and lower calf. It had lasted for 1½years before presentation. Both pains and swelling had been progressive, and it was difficult to walk on the left leg for the past 3 months. He took analgesics with minimal relief. The local examination revealed a hard and tender mass at the lower calf region, about 2 inches above the left ankle. There was significant muscle wasting of the calf muscles, compared to the right leg. The ankle movements were restricted to terminal range only. Thompson’s test for ruptured TA was negative. A plain radiograph revealed a bony mass at the left Taregion (Figs. 1, 2). 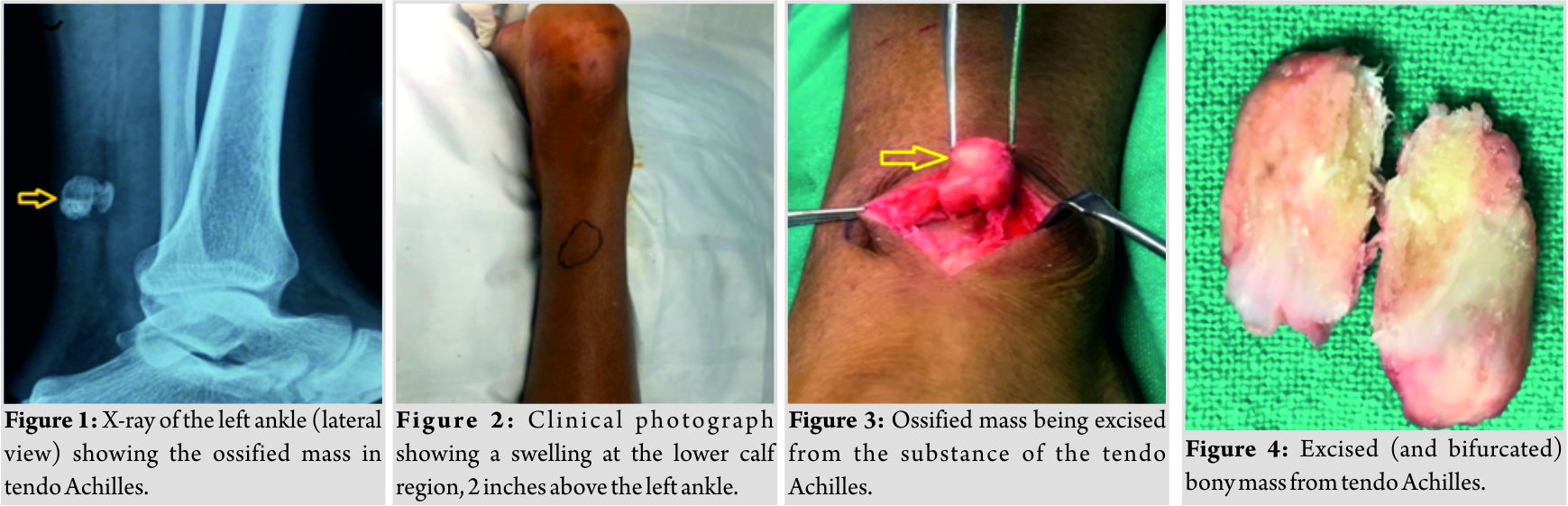 The magnetic resonance imaging (MRI) confirmed the presence of a bony mass within the substance of TA. All the clinical and biochemical laboratory tests, including serum calcium levels, were within normal limits. The heterotopic bone mass was removed, using a posterior longitudinal incision over the left Achilles tendon, centering over the bony mass. The TA was split carefully, and bony mass of 3 inches × 2 inches was removed (Figs. 3, 4). The split TA (Fig. 5) was repaired primarily (Fig. 6) using no. 2 Ethibond™ (Ethicon), and the wound was closed in layers. The histopathology of the excised bony mass (Fig. 7) revealed tendinous tissue showing the exuberant metaplastic bone formation of woven and lamellar types and is laid down as anastomosing thick trabeculae with focal osteoblastic rimming and separated by intertrabecular spaces containing chiefly mature adipose tissue. The trabeculae show evenly distributed osteocytes with lacunar spaces. These histopathological features were suggestive of HOTA. An above knee plaster slab was applied, with the ankle in plantar flexion. The plaster slab was removed after 4 weeks, and a Foam Pneumatic Walker™ (AIRCAST, USA) was given for 2 months more for walking. At 6 months of follow-up, the patient had no pain, swelling, and a full range of ankle movements. The TA was intact on clinical examination.
The magnetic resonance imaging (MRI) confirmed the presence of a bony mass within the substance of TA. All the clinical and biochemical laboratory tests, including serum calcium levels, were within normal limits. The heterotopic bone mass was removed, using a posterior longitudinal incision over the left Achilles tendon, centering over the bony mass. The TA was split carefully, and bony mass of 3 inches × 2 inches was removed (Figs. 3, 4). The split TA (Fig. 5) was repaired primarily (Fig. 6) using no. 2 Ethibond™ (Ethicon), and the wound was closed in layers. The histopathology of the excised bony mass (Fig. 7) revealed tendinous tissue showing the exuberant metaplastic bone formation of woven and lamellar types and is laid down as anastomosing thick trabeculae with focal osteoblastic rimming and separated by intertrabecular spaces containing chiefly mature adipose tissue. The trabeculae show evenly distributed osteocytes with lacunar spaces. These histopathological features were suggestive of HOTA. An above knee plaster slab was applied, with the ankle in plantar flexion. The plaster slab was removed after 4 weeks, and a Foam Pneumatic Walker™ (AIRCAST, USA) was given for 2 months more for walking. At 6 months of follow-up, the patient had no pain, swelling, and a full range of ankle movements. The TA was intact on clinical examination.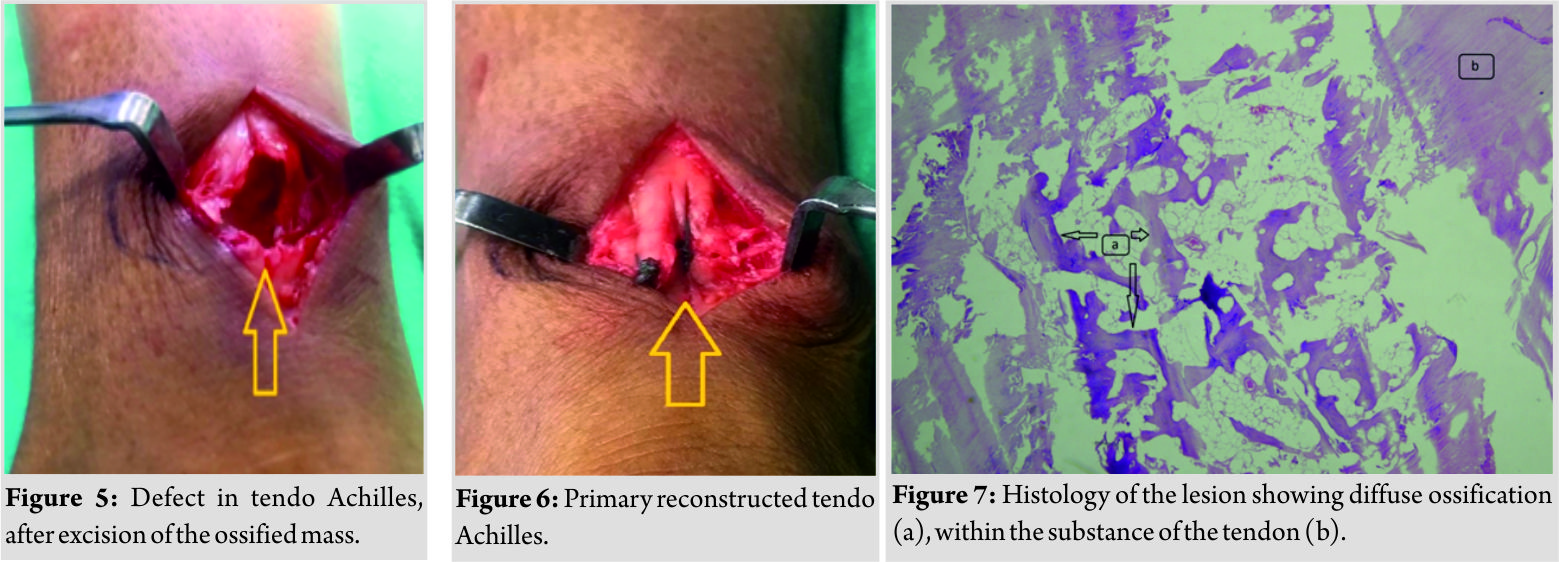
Discussion
HOTA is a rare disease globally and was first described by Horing in 1908 [1]. Males are affected twice as compared to females [1, 4] andmaybea unilateral or a bilateral condition. The exact etiology HOTA remains unknown [1, 2, 3, 5], but there are known predisposing factors associated with this condition. These include the following: Trauma which has been regarded as one of the most frequent factors [5]. Trauma can be in the form of accidental from falls, sports injuries, and road traffic accidents affecting the TA. Trauma can also result from surgery involving the tendon [4]. Repetitive trauma is known to have more influence than single trauma [1]. Other factors are infections such aschronic osteomyelitis of the tibia, gastrocnemius abscess, and syphilis. Metabolic and autoimmune disease including diabetes mellitus, Reiter’s disease, fluorosis, ochronosis, Wilson’s disease, diffuse idiopathic skeletal hyperostosis, and ankylosing spondylitis may be associated with HOTA [4, 5, 6, 7]. Clinical features of HOTA include pain, swelling, and restricted range of motion. There may be an affectation of the activities of daily living [1, 2, 4]. The examination will show the presence of mass or swelling at the posterior aspect of the ankle. The investigation includes X-rays which will show calcification, computed tomography (CT)-scan revealing the presence of solid bone with true trabeculae pattern, and MRI which shows the presence of ossification [3, 4] within TA substance. Ultrasonography may also be helpful in the diagnosis (8). The pathology of HOTA is not well elucidated. Histologic features of HOTA are ossification, calcification, or combination of both [6]. Ossification can be endochondral or intramembranous while calcification is usually dystrophi (9).Various hypotheses have been proposed for the etiopathogenesis of this condition. Some include abnormal bone formation from fibroblast within the tendon with deposition of calcium ions, resulting in osseous metaplasia [5]. Vascular insufficiency resulting from repetitive trauma which leads to collagen deposition and calcium deposition is also believed to cause HOTA. There is also a theory of pericyte transformation into chondrocytes and osteoblasts within the substance of the tendon leading to the formation HOTA. None of these theories have been proved, as yet[5]. Morris KL, classified HOTA into three types:
• Type 1: The lesion is at the tendinous insertion or the superior pole of the calcaneus.
• Type 2: Intratendinous lesion is located 1–3cm proximal to the TA insertion.
• Type 3: The lesion is found proximally to the insertion zone, upward of 12 cm.
• Type 3a: Partial tendinous ossification.
• Type 3b: Complete tendinous insertion.
Treatment of HOTA can be conservative or surgical(11). Non-surgical measures include the use of analgesics such as non-steroidal anti-inflammatory drugs, opioid analgesics, and physical therapy. After a failed conservative treatment, the surgical treatment is recommended, which includes excision of the heterotopic bone and reconstruction of the transected tendon. Reconstruction may be possible with a primary repair. However, sometimes, the gap in the tendon is bridged using various tendon autografts (e.g., plantaris, tensor fascia lata, peroneus brevis, gastrocnemius, and soleal grafts) [5]. Overall, the reported prognosis after this surgical treatment is good, and the recurrence is minimal.
Conclusion
HOTA is a rare clinical condition. The exact cause is unknown, although there are documented predisposing factors. Clinical manifestation includes pain and swelling at the back of the ankle and restricted range of movement and affectation of activity of daily living. The mainstay of diagnosis is radiological using X-rays, CT-scan, or MRI. Treatment is usually conservative, but surgery is required in cases with a failed conservative approach. Prognosis is good, and there is a low recurrence rate.
Clinical Message
HOTA is a rare clinical condition presenting with pain and swelling around back of the heel and can be managed conservatively, but surgical intervention may be required in selected cases.
References
1. Arora AJ, Arora R. Ossification of the bilateral Achilles tendon: A rare entity. Acta Radiol Open 2015;4:2058460115599184.
2. Cortbaoui C, Matta J, Elkattah R. Could ossification of the Achilles tendon have a hereditary component? Case Rep Orthop 2013;2013:539740.
3. Quijano VJ. Successful Treatment of an Ossified Achilles Tendon with Human Dermal Regenerative Matrix. Am Board of Lower Extremity Trauma; 2015. Available from: https://www.ables.org/successful-treatment-of-an-ossified-achilles-tendon-oat/.
4. Hatori M, Matsuda M, Kokubun S. Ossification of Achilles tendon-report of three cases. Arch Orthop Trauma Surg 2002;122:414-7.
5. Richards PJ, Braid JC, Carmont MR, Maffulli N. Achilles tendon ossification: Pathology, imaging and aetiology. Disabil Rehabil 2008;30:1651-65.
6. Joshi N, Diaz E, Massona J. Achilles tendon ossification. Acta Orthop Belg 1994;60:432-3.
7. Siddiq MA, Jahan I. Asymmetrical Achilles tendon ossification and rare heel pain. Australas Med J 2017;10:222-5.
8. Tamam C, Yildirim D, Tamam M, Mulazimoglu M, Ozpacaci T. Bilateral Achilles tendon ossification: Diagnosis with ultrasonography and single photon emission computed tomography/computed tomography. Case report. Med Ultrason 2011;13:320-2.
9. Fenwick S, Harrall R, Hackney R, Bord S, Horner A, Hazleman B, et al. Endochondral ossification in Achilles and patella tendinopathy. Rheumatology (Oxford) 2002;41:474-6.
10. Morris KL, Giacopelli JA, Granoff D. Classifications of radiopaque lesions of the tendo Achilles. J Foot Surg 1990; 29: 533–542
11. Longo UG, Ronga M, Maffulli N. Achilles tendinopathy. Sports Med Arthrosc Rev 2009;17:112-26.
 |
 |
 |
 |
 |
| Dr. Raju Vaishya | Dr. Celestine O Maduka | Dr. Amit Kumar Agarwal | Dr. Vipul Vijay | Dr. Abhishek Vaish |
| How to Cite This Article: Vaishya R, Maduka CO, Agarwal AK, Vijay V, Vaish A. Heterotopic Ossification of Tendo Achilles: An Uncommon Clinical Entity. Journal of Orthopaedic Case Reports 2019 Mar-Apr; 9(2): 45-47. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




