[box type=”bio”] Learning Point of the Article: [/box]
A high index of suspicion and timely diagnosis and management of femoral neck stress fractures is important for optimal outcomes.
Case Report | Volume 9 | Issue 2 | JOCR March – April 2019 | Page 90-93 | Himanshu Kanwat, Samarth Mittal, Vivek Trikha, Rajesh Malhotra. DOI: 10.13107/jocr.2250-0685.1388
Authors: Himanshu Kanwat[1], Samarth Mittal[1], Vivek Trikha[1], Rajesh Malhotra[1]
[1]Department of Orthopaedics, All India Institute of Medical Sciences, New Delhi, India.
Address of Correspondence:
Dr. Samarth Mittal,
Department of Orthopaedics, Jai Prakash Narayan Apex Trauma Center, All India Institute of Medical Sciences, New Delhi, India.
E-mail: samarthmittal@gmail.com
Abstract
Introduction: Stress fractures of the neck of femur are a rare injury mostly seen in athletes, military recruits, elderly patients, and patients with metabolic bone diseases. Such injury patterns are rare in otherwise healthy and non-athletic individuals. Bilateral presentation in such population is even rarer.
Case Report: We present a case of bilateral neck of femur stress fracture (compression type) in a healthy 50-year-old housewife treated with osteosynthesis with three cannulated screws on one side and total hip replacement on other sides. Follow-up at 1 year revealed optimum results.
Conclusion: This report highlights the importance of diagnosis and early intervention in such cases to prevent complications and morbidity.
Keywords: Stress fracture, neck of femur, arthroplasty, non-athletic.
Introduction
Femoral neck stress fracture (FNSF) is a rare injury firstreported by Blecher, in 1905 [1]. They account for 5% of total stress fractures and are usually reported in long-distance runners, military recruits, elderly patients, and patients with bone abnormalities such asosteoporosis, renal osteodystrophy, steroid use, and metabolic bone disease [1,2,3,4,5,6]. Very few cases have been reported in otherwise healthy non-athletic individuals with bilateral affections are rarer. We present an unusual case of bilateral compression type FNSF in a 50 years old otherwise healthy housewife in which one side progressed to complete displacement. We also outline issues faced in the management of such cases.
Case Report
A 50-year-old housewife presented in the emergency department of our level 1 trauma center with complaints of pain and immobility of the left hip joint and inability to bear weight for the past 20 days. She gave a history of bilateral anterior groin pain (left > right) for the past 4 months. She also had a history of limping, difficulty in sitting cross-legged, and squatting for the same period. The pain was insidious in onset and progressed over time to make her bedridden. On examination, there was tenderness over bilateral hip joints (left > right), external rotation deformity, and 1 cm shortening of the left lower limb. Movement of the left hip joint was extremely painful and was not encouraged. There was pain at extremes of motion of the right hip joint. The patient was able to do straight leg raise on the right side but not on the left side. Neurovascular examination was bilaterally unremarkable. The patient had no comorbidities and was not on any long-term medication. There was no history of trauma (trivial or overt), excessive physical activity, or fragility fractures in the past. The patient was postmenopausal for2 years. The patient was actively mobile before the onset of symptoms. She consulted a local practitioner during initial stages of her discomfort who had prescribed her NSAIDs. However, there was no relief and pain progressed to such an extent that she was not able to bear weight. A 20 days earlier anteroposterior pelvis with bilateral hip radiograph (Fig. 1) showed sclerosis over bilateral inferomedial femoral neck with cortical breach in the right side and an undisplaced complete fracture line over the left side. The neck shaft angle was 130° on the right side and 114° on the left side. Plain radiographs were ordered on presentation which showed a displaced fracture neck of femur on the left side collapsed in varus and sclerosis over inferomedial aspect of the right femoral neck with cortical breach. A computed tomography scan confirmed the X-ray diagnosis (Fig. 2).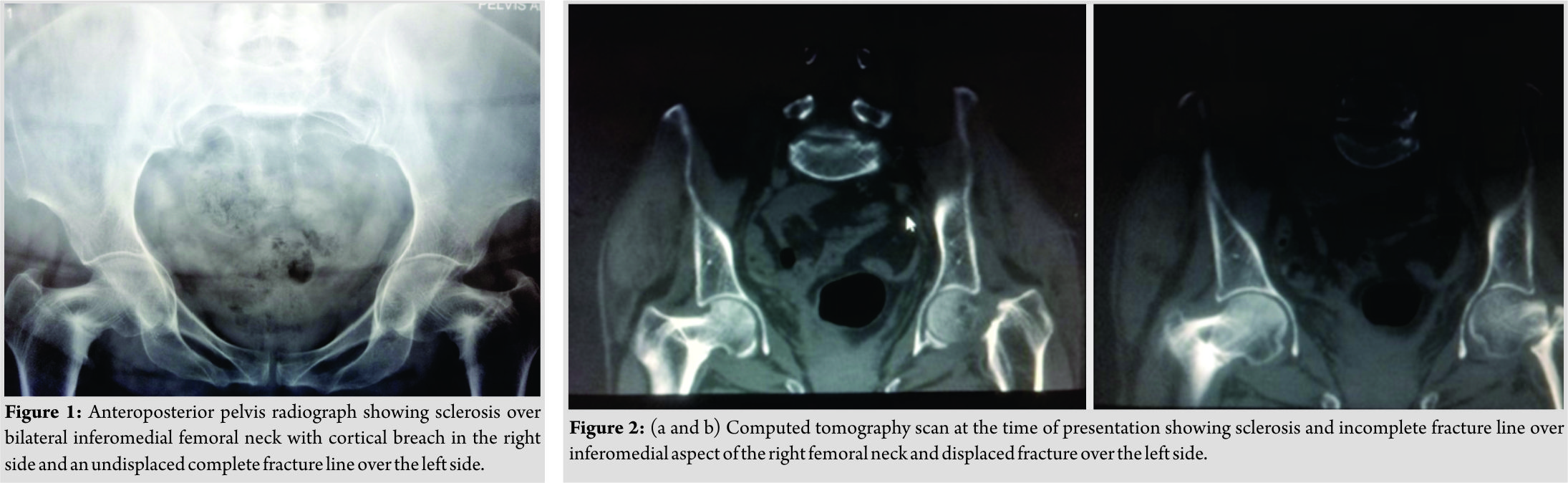 Blood investigations showed a normal calcium profile, Vitamin D, and serum parathyroid hormone levels. DEXA scan showed normal t- and z-scores in hip and spine. Whole spine radiographs revealed no abnormalities. Thus, a diagnosis of bilateral FNSFs was made and the patient was admitted for surgical stabilization. She underwent osteosynthesis with three cannulated screws on the right side and 2 days later underwent total hip arthroplasty for displaced fracture on the left side (Fig. 3). Postoperatively, she was allowed full weight-bearing mobilization on the left side and toe touch on the right side. There were no post-operative complications. Radiographs were repeated at 3 weeks, 6 weeks, 3 months, 6 months, and 1 year postoperatively which showed union at the right side with no further varus collapse or implant failure (Fig. 4). The left side with hip prosthesis was also normal. At 1-year follow-up, the patient was pain free, able to walk full weight-bearing without support and carry out her daily activities comfortably.
Blood investigations showed a normal calcium profile, Vitamin D, and serum parathyroid hormone levels. DEXA scan showed normal t- and z-scores in hip and spine. Whole spine radiographs revealed no abnormalities. Thus, a diagnosis of bilateral FNSFs was made and the patient was admitted for surgical stabilization. She underwent osteosynthesis with three cannulated screws on the right side and 2 days later underwent total hip arthroplasty for displaced fracture on the left side (Fig. 3). Postoperatively, she was allowed full weight-bearing mobilization on the left side and toe touch on the right side. There were no post-operative complications. Radiographs were repeated at 3 weeks, 6 weeks, 3 months, 6 months, and 1 year postoperatively which showed union at the right side with no further varus collapse or implant failure (Fig. 4). The left side with hip prosthesis was also normal. At 1-year follow-up, the patient was pain free, able to walk full weight-bearing without support and carry out her daily activities comfortably.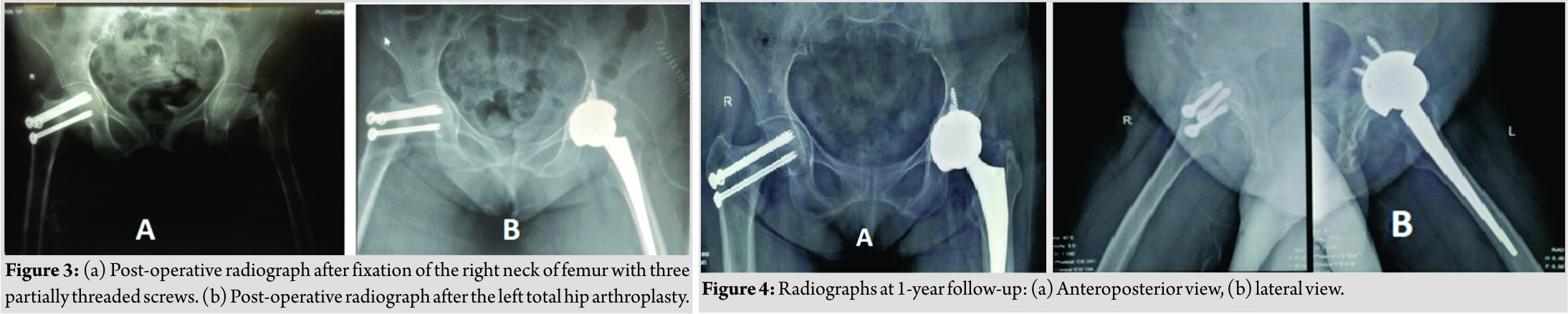
Discussion
Stress fractures occur due to repetitive loading which leads to mechanical failure of the bone [7]. Such injuries occur either due to abnormal stresses on a normal bone (fatigue fractures) or normal stresses on an abnormal bone (insufficiency fractures) [8]. FNSFs account for 5% of total stress fractures [2]. These injuries are most commonly encountered in long-distance runners, military recruits, elderly patients with osteoporosis, steroid use, renal abnormalities, and other metabolic bone diseases [1, 3, 4, 5, 6]. However, FNSFs are rare in otherwise healthy non-athletic individuals and bilateral affections are even rarer with only few cases and small series reported to the best of our knowledge [9]. Fullerton et al. in their series of 54 cases of the FNSFs in military recruits proposed a classification scheme [1]. They classified these injuries into three categories on the basis of biomechanics and displacement (Table 1). 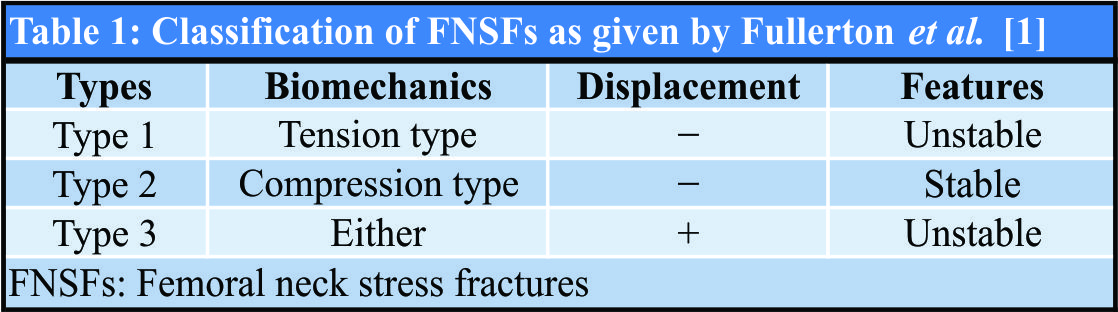 The tension-type FNSF is unstable and more likely to advance into a displaced fracture as compared to the compression type, whereas a displaced fracture is an emergency that has to be fixed to prevent complications [1]. The earliest and most frequent symptom is anterior groin pain and the most common sign is pain at extremes of hip movement [1]. However, ~75% of FNSFs may be undiagnosed by clinical examination alone [10]. Differential diagnoses may include trauma, infection, osteonecrosis, neoplastic, and inflammatory conditions [9]. A high index of suspicion is needed as this condition may not be initially evident on plain radiographs with sensitivity rates as low as 10–29% [9]. MRI is the investigation of choice for diagnosis and differentiation from tumor and infection which shows increased signal intensity on T2-weighted images and has a sensitivity and specificity of 100% [9]. In our case, the signs and symptoms pointed toward an FNSF and radiographs and CT scan confirmed it and no MRI was required. We also investigated and ruled out systemic or metabolic diseases that may point toward insufficiency fractures to support our diagnosis. Treatment of FNSFs has always been a debate. Fullerton et al. in their case series advocated conservative treatment for compression-type fractures due to their stable nature with bed rest and avoidance of weight-bearing and internal fixation for tension type, compression type with complete fracture line, and displaced FNSFs [1]. We did literature review regarding treatment modalities employed by various authors in cases of bilateral FNSFs (Table 2). In our case, we fixed the compression type FNSF on the right side and performed total hip replacement on the fully displaced fracture on the left side. We agree with Naik et al. [9] that all types of FNSF if bilateral must be stabilized because it is imperative that the patients need to be mobilized as early as possible, more so in our case who was a postmenopausal 50-year-old lady. Another rationale regarding operative management of compression-type FNSF in such age group is the risk of non-union as shown by Xiaozuo et al. [11] in which there was non-union at conservatively managed side in case of a bilateral FNSF in a 59-year-old lady. Displacement of FNSFs is the main determinant of outcome with a 60% risk of non-union and 30% risk of avascular necrosis (AVN) in displaced FNSFs [12]. Considering the age of our case, the risk of non-union and AVN is more as can be attributed to displacement alone. Therefore, we opted for total hip arthroplasty for the displaced femoral neck stress fracture.
The tension-type FNSF is unstable and more likely to advance into a displaced fracture as compared to the compression type, whereas a displaced fracture is an emergency that has to be fixed to prevent complications [1]. The earliest and most frequent symptom is anterior groin pain and the most common sign is pain at extremes of hip movement [1]. However, ~75% of FNSFs may be undiagnosed by clinical examination alone [10]. Differential diagnoses may include trauma, infection, osteonecrosis, neoplastic, and inflammatory conditions [9]. A high index of suspicion is needed as this condition may not be initially evident on plain radiographs with sensitivity rates as low as 10–29% [9]. MRI is the investigation of choice for diagnosis and differentiation from tumor and infection which shows increased signal intensity on T2-weighted images and has a sensitivity and specificity of 100% [9]. In our case, the signs and symptoms pointed toward an FNSF and radiographs and CT scan confirmed it and no MRI was required. We also investigated and ruled out systemic or metabolic diseases that may point toward insufficiency fractures to support our diagnosis. Treatment of FNSFs has always been a debate. Fullerton et al. in their case series advocated conservative treatment for compression-type fractures due to their stable nature with bed rest and avoidance of weight-bearing and internal fixation for tension type, compression type with complete fracture line, and displaced FNSFs [1]. We did literature review regarding treatment modalities employed by various authors in cases of bilateral FNSFs (Table 2). In our case, we fixed the compression type FNSF on the right side and performed total hip replacement on the fully displaced fracture on the left side. We agree with Naik et al. [9] that all types of FNSF if bilateral must be stabilized because it is imperative that the patients need to be mobilized as early as possible, more so in our case who was a postmenopausal 50-year-old lady. Another rationale regarding operative management of compression-type FNSF in such age group is the risk of non-union as shown by Xiaozuo et al. [11] in which there was non-union at conservatively managed side in case of a bilateral FNSF in a 59-year-old lady. Displacement of FNSFs is the main determinant of outcome with a 60% risk of non-union and 30% risk of avascular necrosis (AVN) in displaced FNSFs [12]. Considering the age of our case, the risk of non-union and AVN is more as can be attributed to displacement alone. Therefore, we opted for total hip arthroplasty for the displaced femoral neck stress fracture.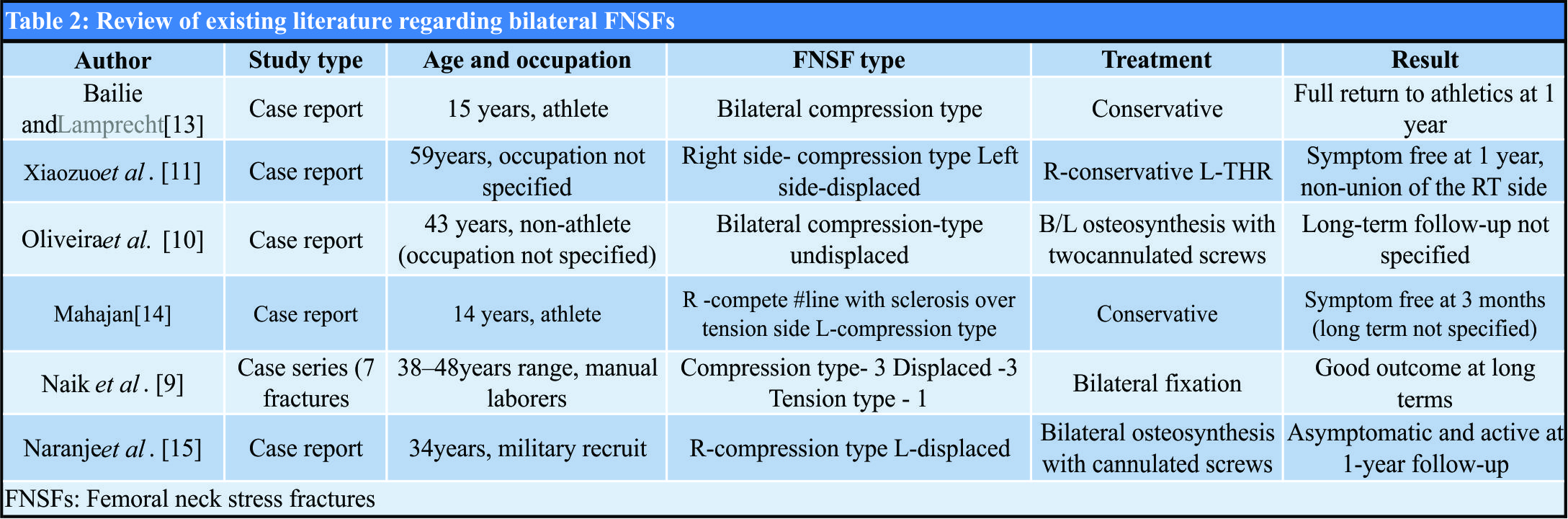
Conclusion
Our case was unique in the sense that FNSFs in a healthy, non-athletic individual are rare and bilateral affection is even rarer. Second, we also infer that compression-type FNSF can also propagate into displaced fractures if neglected contrary to the belief of them being stable. This highlights the importance of having a high index of suspicion of the FNSFs in this unusual population. It also draws attention toward the need for early diagnosis and intervention to prevent full displacement of these fractures which is fraught with serious complications.
Clinical Message
FNSFs although common in athletes and osteoporotic bone can also be found in otherwise healthy individuals and one should be on a lookout to prevent missing such a presentation since an early intervention is associated with favorable outcome.
References
1. Fullerton LR Jr., Snowdy HA. Femoral neck stress fractures. Am J Sports Med 1988;16:365-77.
2. Clement DB, Ammann W, Taunton JE, Lloyd-Smith R, Jesperson D, McKay H, et al. Exercise-induced stress injuries to the femur. Int J Sports Med 1993;14:347-52.
3. Gurdezi S, Trehan RK, Rickman M. Bilateral undisplaced insufficiency neck of femur fractures associated with short-term steroid use: A case report. J Med Case Rep 2008;2:79.
4. Karapinar H, Ozdemir M, Akyol S, Ulkü O. Spontaneous bilateral femoral neck fractures in a young adult with chronic renal failure. Acta Orthop Belg 2003;69:82-5.
5. Chadha M, Balain B, Maini L, Dhal A. Spontaneous bilateral displaced femoral neck fractures in nutritional osteomalaciaa case report. Acta Orthop Scand 2001;72:94-6.
6. Haddad FS, Mohanna PN, Goddard NJ. Bilateral femoral neck stress fractures following steroid treatment. Injury 1997;28:671-3.
7. Knapp TP, Garrett WE Jr. Stress fractures: General concepts. Clin Sports Med 1997;16:339-56.
8. Markey KL. Stress fractures. Clin Sports Med 1987;6:405-25.
9. Naik MA, Sujir P, Tripathy SK, Vijayan S, Hameed S, Rao SK, et al. Bilateral stress fractures of femoral neck in non-athletes: A report of four cases. Chin J Traumatol 2013;16:113-7.
10. Oliveira US, Labronici PJ, João Neto A, Nishimi AY, Pires RE, Silva LH, et al. Bilateral stress fracture of femoral neck in non-athlete case report. Rev Bras Ortop 2016;51:735-8.
11. Xiaozuo Z, Kai K, Jiangtao D, Shijun G. Bilateral stress fractures of the femoral neck in adults: A case report. Int J Clin Exp Med 2016;9:16840-6.
12. Johansson C, Ekenman I, Törnkvist H, Eriksson E. Stress fractures of the femoral neck in athletes. The consequence of a delay in diagnosis. Am J Sports Med 1990;18:524-8.
13. Bailie DS, Lamprecht DE. Bilateral femoral neck stress fractures in an adolescent male runner. A case report. Am J Sports Med 2001;29:811-3.
14. Mahajan A. Simultaneous bilateral femoral neck stress fractures in a young female runner: A case report and review of literature. Saudi J Sports Med 2017;17:60-3.
15. Naranje S, Sezo N, Trikha V, Kancherla R, Rijal L, Jha R, et al. Simultaneous bilateral femoral neck stress fractures in a young military cadet: A rare case report. Eur J Orthop Surg Traumatol 2012;22 Suppl 1:103-6.
 |
 |
 |
 |
| Dr. Himanshu Kanwat | Dr. Samarth Mittal | Dr. Vivek Trikha | Dr. Rajesh Malhotra |
| How to Cite This Article: Kanwat H, Mittal S, Trikha V, Malhotra R. Unusual Bilateral Neck of Femur Stress Fracture in a Healthy, Non-athletic Individual – A Case Report and Literature Review. Journal of Orthopaedic Case Reports 2019 Mar-Apr; 9( 2): 90-93. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




