[box type=”bio”] Learning Point of the Article: [/box]
Although extremely rare superior gluteal artery lesion during intramedullary femoral nailing should the faced as a potential life threatening complication.
Case Report | Volume 9 | Issue 6 | JOCR November – December 2019 | Page 27-31 | Pedro Xavier Fernandes, Duarte Manuel Medeiros, Raquel C Teixeira, Andreia Mercier Nunes, Antonio Sousa Seco0, Afonso Cevadinha Caetano. DOI: 10.13107/jocr.2019.v09.i06.1574
Authors: Pedro Xavier Fernandes[1], Duarte Manuel Medeiros[2], Raquel C Teixeira[1], Andreia Mercier Nunes[1], Antonio Sousa Seco[3], Afonso Cevadinha Caetano[1]
[1]Department of Orthopaedic Surgery, Hospital de São Francisco Xavier, Centro Hospitalar de Lisboa Ocidental, Estrada do Forte do Alto do Duque, 1495-005 Lisbon, Portugal,
[2]Department of Vascular Surgery, Hospital de Egas Moniz,Centro Hospitalar de Lisboa Ocidental, R. da Junqueira 126, 1349-019 Lisbon, Portugal,
[3]Department of Orthopaedic Surgery, Hospital Lusiadas, R. Abílio Mendes 12, 1500-458 Lisbon, Portugal.
Address of Correspondence:
Dr. Pedro X. Fernandes,
Department of Orthopaedic Surgery, Hospital de São Francisco Xavier, Centro Hospitalar de Lisboa Ocidental, Estrada do Forte do Alto do Duque, 1495-005 Lisbon, Portugal.
E-mail: pmxfernandes@gmail.com
Abstract
Introduction: Proximal femoral fractures represent a health problem of global proportions. Iatrogenic vascular lesion in the treatment of these fractures is an unusual potentially lethal complication, reported in only 0.2% of trochanteric fractures treated with intramedullary implants. Superior gluteal artery injury is extremely rare, with only two cases reported in literature.
Case Report: A 66-year-old Caucasian woman, with metastatic disease, was admitted with a right pertrochanteric fracture. She underwent closed reduction and long intramedullary nail fixation. Five days post-operatively, a sudden hemoglobin drop occurred. A computed tomography demonstrated an extensive hematoma. Angiography confirmed an arterial bleeding from the superior gluteal artery and subsequent selective embolization was successfully performed.
Conclusion: The presence of anemia and thigh hematoma that progressively worsens post-operatively should raise the diagnostic suspicion of an iatrogenic vascular injury. To the best of our knowledge, this is only the third case reported of superior gluteal artery injury after intramedullary fixation of a proximal femoral fracture. We describe the post-operative course and management strategy and hope this will contribute to the global knowledge and increase awareness of these rare injuries.
Keywords: Vascular injury, trochanteric fractures, intramedullary fracture fixation, therapeutic embolization.
Introduction
Proximal femoral fractures represent a health problem of global proportions. They are among the most common orthopedic injuries, with more than 250,000 cases occurring annually in the United States [1]. The last available Portuguese data (2006) on proximal femoral features, described a total incidence of 9523 features per year [2]. Worldwide, it is expected that the number of these fractures will rise from 1.66 million in 1990 to 3.94 million in 2025 and 6.26 million by 2050 [3]. Most of these fractures occur in persons over the age of 65 years, with a peak of incidence around 80 years of age [1]. The highest rates are found among Caucasian women, with a female-male ratio of 3:1 [4]. In general, they result from a minimal or moderate trauma and approximately half occur in the trochanteric region [1, 5]. Proximal femoral nailing requires traction, adduction, and internal rotation of the injured limb, putting substantial pressure on soft tissues of the hip and thus potentially causing vascular lesions [6]. Vascular injury during intramedullary fixation of proximal femoral fractures is a rare, potentially limb- and life-threatening complication reported to occur in 0.2% of trochanteric fractures [7, 8]. In the majority of the cases, the injured vessel is a branch of the deep femoral artery [7, 8]. Superior gluteal artery injury is extremely rare, with only two cases described in literature [7, 8].
Case Report
The patient was a 66-year-old Caucasian overweight (body mass index [BMI] 26.7 kg/m2) woman, with medical history relevant for multiple myeloma, with complete therapeutic response since 2011; left hemicolectomy for sigmoid cancer in 2013; radical mastectomy for breast cancer in 2015; and abnormal liver function tests in the context of metastatic disease of unknown origin, detected in April 2016.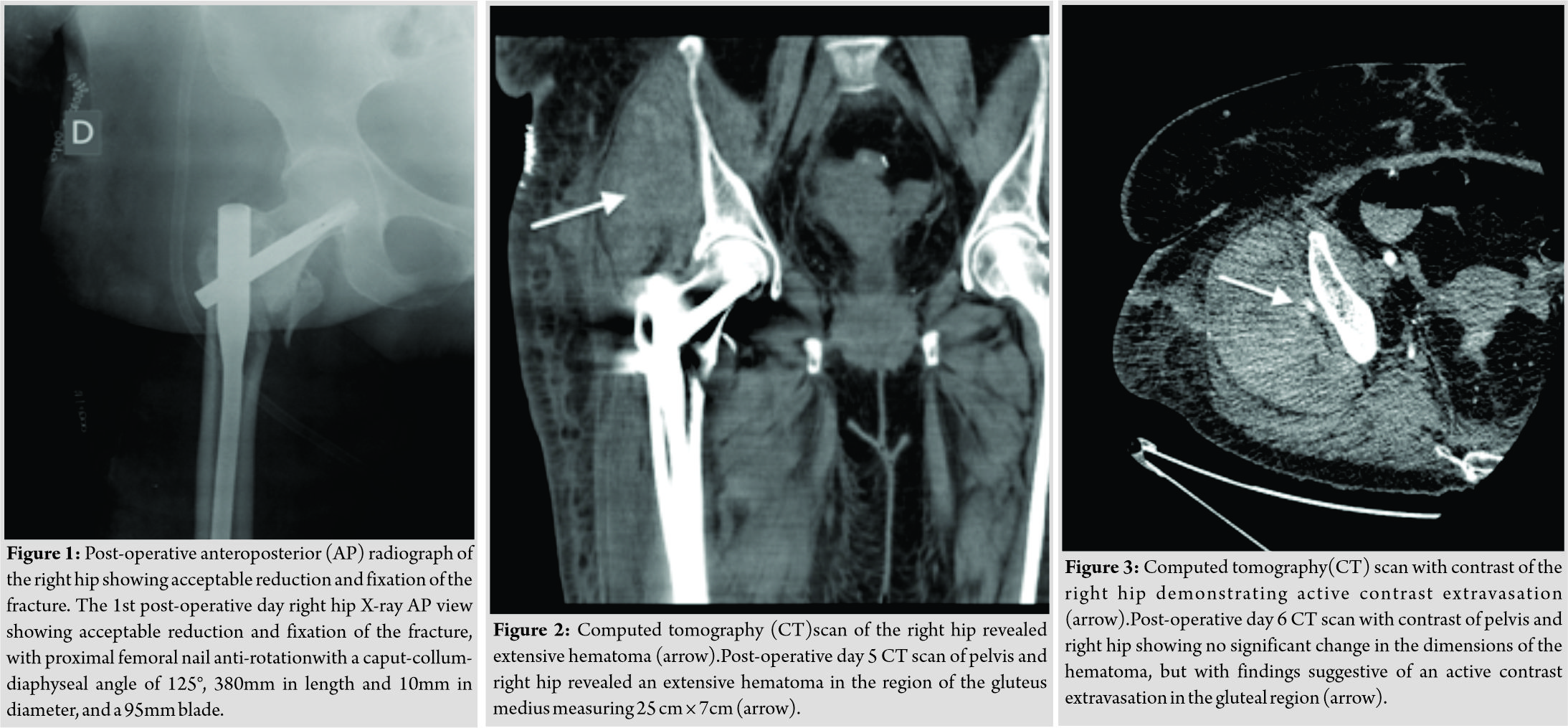
She was admitted with the diagnosis of the right TF (Arbeitsgemeinschaft für Osteosyn these fragen 31-A2) after a low-energy fall from a standing height. Laboratory studies showed abnormal coagulation (prothrombin time [PT] 20.5s, activated partial thromboplastin time [aPTT] 25.6s, and international normalized ratio [INR] 1.9) and normal platelet count (193 ×109/L). The patient was not under anticoagulation or antiplatelet therapy. From day 1, she received thromboprophylaxis with enoxaparin (40mg subcutaneously once daily) and compression stockings.
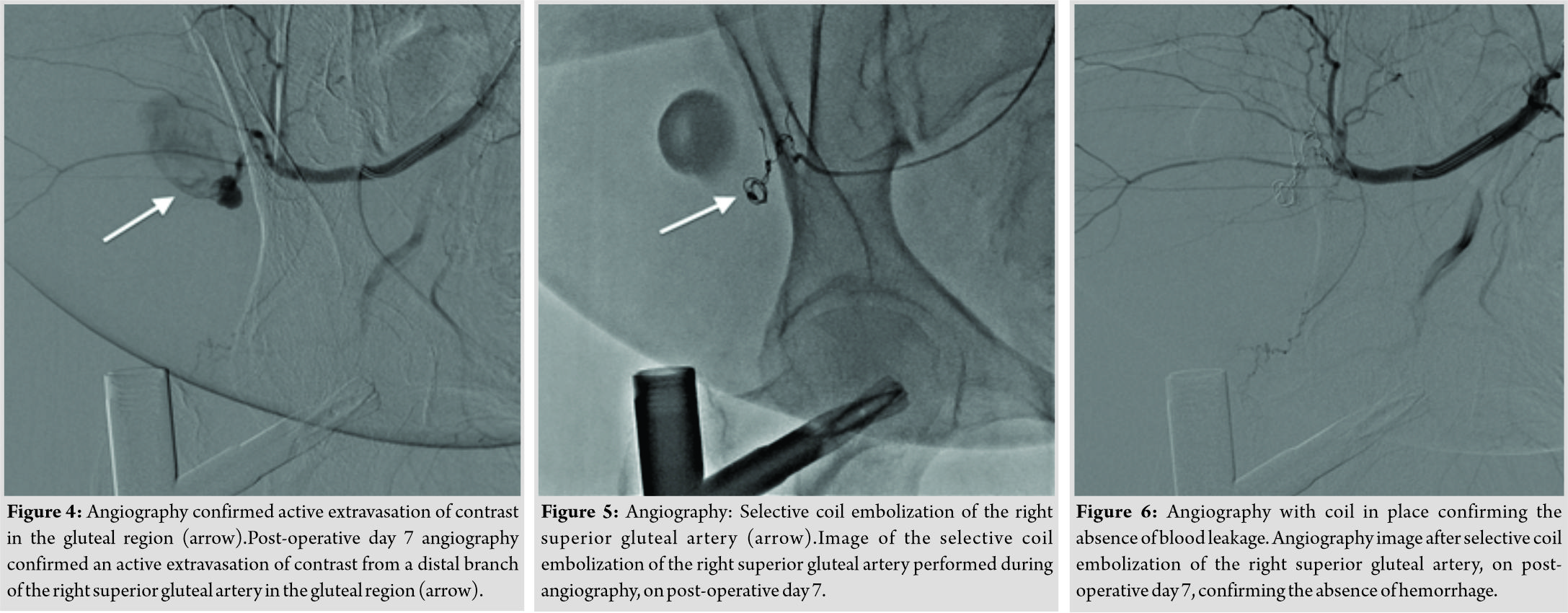
Eleven days post-injury and after clinical stabilization, the patient underwent a closed reduction and long intramedullary nail fixation (coagulation tests were PT 13.8s, aPTT31.9s, and INR 1.3). For the closed reduction, we made moderate traction to the injured limb until length was restored, with approximately 15° of internal rotation and 20° of adduction. After confirming the appropriate reduction of the fracture, the torso was abducted 15° to the unaffected side. Afterward, we proceeded with disinfection and applied the following surgical protocol. First, 5cm longitudinal skin incision was made approximately 3cm proximal to the greater trochanter, and the fascia lata and abductor muscles were subsequently split in line with their fibers, from caudaltocranial with scalpel, through 8cm incision, centered on the skin cut. After insertion of the guide wire and reaming of the medullary canal upto 11.5mm under imaging control and with the aid of a soft tissue protector, an anterograde long femoral nail (proximal femoral nail anti-rotation; Synthes®Oberdorf, Switzerland), with a caput-collum-diaphyseal angle of 125°, 380mm in length, and 10mm in diameter, was implanted. A 95mm blade and two distal locking screws (40mm and 42mm) were used. Acceptable reduction and fixation were attained (Fig. 1). No significant bleeding was documented. Intraoperative bone biopsy was obtained during the proximal reaming and sent to pathology. Total operative time was 66 min and the estimated blood loss was 200cc. On the 1stpost-operative day, the patient developed an extensive ecchymosis of the thigh, attributed to the normal evolution of the fracture hematoma. She was transfused with two units of packed red blood cells (PRBCs), with an appropriate rise of hemoglobin level from 5.6g/dL to 9.2g/dL. She remained hemodynamically stable and began rehabilitation 2 days after surgery. Surgical dressings remained clean and dry. Two supplementary units of PRBCs were administered for persistent anemia on post-operative day 3, without evidence of increased swelling or ecchymosis. The patient general condition was stable. However, pain and diffuse swelling of the thigh were not alleviated and, on post-operative day 5, there was an abrupt drop in hemoglobin level to 5g/dL, without evidence of gastrointestinal or urinary tract bleeding, neurological signs, or abdominal pain. She was transfused with two additional units of PRBCs and transferred to the intermediate care unit for monitoring. The thigh was recognized to be swollen but not tense. The patient underwent a computed tomography (CT) scan of the right hip, which demonstrated an extensive hematoma in the region of the gluteus medius, measuring 25 ×7cm (Fig. 2). On the following day, a CT scan with contrast showed no significant change in the dimensions of the hematoma but revealed findings suggestive of an active contrast extravasation in the gluteal region (Fig. 3). Angiography was subsequently performed, on post-operative day 7, and confirmed an active extravasation of contrast from the right superior gluteal artery that was coiled and embolized (Fig. 4, 5, 6). During the remnant of her hospital stay, the patient did not require further transfusions and remained hemodynamically stable. She resumed her physiotherapy rehabilitation 2 days post-angiography. Pathology confirmed the diagnosis of bone metastases from breast carcinoma. The patient was discharged on post-operative day 25, after the treatment of urinary tract infection caused by Klebsiella extended-spectrum beta-lactamases. After discharged clinical deterioration occurred and the patient died of metastatic cancer 3 months after surgery.
Discussion
Vascular injuries associated with the treatment of trochanteric fractures are a very rare complication [7, 8]. When they occur, they involve more frequently extrapelvic vessels (91.20%), compared with intrapelvic vessels (8.24%), with only one case of combined injury [8]. In the extrapelvic group, the deep femoral artery and its branches are the most affected (78.31%) followed by the superficial femoral vessels (10.84%). Rarely, there is an involvement of other arteries of the hip and thigh [8]. The main reasons described for lesions of deep femoral artery include: Direct damage caused by bone fragments; over-penetration of drill bits; prolonged irritation of the artery wall due to protruding screws; and injuries caused by retractors poorly placed [6, 8]. To the best of our knowledge, only two cases of injury to the superior gluteal artery during intramedullary fixation of a proximal femur fracture have been described in literature [7,8], one case reported in a subtrochanteric and the other in a trochanteric fracture. Arterial injury can occur at the time of fracture, during surgery or after it, early during post-operative mobilization or late, weeks, months, or even years after surgery [8]. Normally, it presents as a hemorrhagic syndrome with anemia, tachycardia, hypotension, or even shock [8]. If vascular injury, presenting with mild signs, is suspected, as in our case, the patient should be worked up initially with non-invasive studies such as ultrasonography, CT, or magnetic resonance imaging with contrast [7, 8]. Based on the information obtained from these studies, an appropriate treatment plan can be formulated. If vascular injury is confirmed, angiography would be the next best approach as it identifies the location and extension of the lesion and allows the treatment by selective embolization [6, 8]. A long proximal femoral nail was used given the pathological fracture nature. Intramedullary fixation has been known to be the best treatment option in these cases, as it can be used to protect the entire femur [9]. Injury to the superior gluteal artery throughout intramedullary fixation of a trochanteric fracture is extremely rare. Unlike other cases reported in literature [7, 8], which argue that the damage followed retractor or guide wire insertion, we believe that, in this case, the injury may have occurred during the caudal-to-cranial scalpel split of the fascia lata and abductor muscles. No substantial bleeding other than the expected in the context of intramedullary reaming and abnormal coagulation was showed. The increased BMI may have contributed to the injury, as we had to perform a relatively larger surgical incision. Nevertheless, it cannot be excluded that traction and angulation applied during surgery can cause damage to the endothelium of arteries, especially in the presence of multiple medical comorbidities, including atherosclerosis, with eventual progression to vascular injury once patient’s mobilization started [8]. It is conceivable, as surgery occurred 11 days post-injury, that the normal evolution of bone healing and fibrosis of the surrounding tissues might have hampered fracture reduction, leading indirectly to more distress in an already impaired endothelium and, therefore, contributing to the vessel injury. It is possible that bleeding from the injured vessel reduced or ceased secondary to clot formation shortly after the initial insult, only to resume with probable clot dislodgement on patient mobilization [7]. We do not believe coagulation abnormalities nor the thromboprophylaxis with enoxaparin had a relevant impact in hemorrhage from the superior gluteal artery.
Conclusion
We present only the third case of superior gluteal artery laceration during intramedullary fixation of a trochanteric fracture. The damage may have occurred as a result of the caudal-to-cranial blade orientation; thus, the authors recommend that thru the proximal incision for intramedullary fixation, the scalpel should not be positioned in the caudal-to-cranial orientation and that the abductor muscles should be split with blunt dissection. Further, attention should be made to traction performed in patients with medical comorbidities not to distress an already impaired vessel. Surgical procedures can be complicated by both known and previously unknown problems, prompting the surgeon to be vigilant at all times. When the patient presents with diffuse swelling and pain of the thigh and unexplained anemia following surgery, a CT scan with contrast should be performed. If any extravasation is shown, a subsequent angiography allows the identification and treatment of the injured artery [6, 7, 8]. With this case, we expect to contribute to the worldwide knowledge and increase awareness of this rare injury.
Clinical Message
Trochanteric fractures are among the most common orthopedic injuries. Although these can be safely and reliably treated with proximal femoral nailing, serious intraoperative complications have to be considered.
References
1. Mavrogenis AF, Panagopoulos GN, Megaloikonomos PD, Igoumenou VG, Galanopoulos I, Vottis CT, et al. Complications after hip nailing for fractures. Orthopedics 2016;39:e108-16.
2. Direção-Geral de Saúde. Orientação Técnica Sobre Suplemento de Cálcio e Vitamina D em Pessoas Idosas; 2008. p. 3-5. Available from: https://www.dgs.pt/directrizes-da-dgs/orientacoes-e-circulares-informativas/circular-informativa-n-13dscsdpcddsqc-de-01042008-pdf.aspx.(accessed on 15 March 2017)
3. Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: A world-wide projection. Osteoporos Int 1992;2:285-9.
4. Innocenti M, Civinini R, Carulli C, Matassi F. Proximal femural fractures: Epidemiology. Clin Cases Miner Bone Metab2009;6:117-9.
5. Singh AP, Kochar V. Intramedullary nail versus dynamic hip screw; intramedullary nail (advantages and disadvantages). Trauma Int 2015;1:17-20. Available from: http://www.traumainternational.co.in/intramedullary-nail-versus-dynamic-hip-screw-intramedullary-nail-advantages-disadvantages.(accessed on 22 March 2017)
6. Yoon HK, Oh HC, Park J, Oyunbat C, Kim T. Rupture of the deep femoral artery during proximal femoral nailing following an intertrochanteric fracture: A Case report. Hip Pelvis 2016;28:54-9.
7. Ward JP, Strauss EJ, Tejwani NC. Injury to the superior gluteal artery during intramedullary fixation of an atypical subtrochanteric stress fracture a case report. Bull Hosp Jt Dis (2013) 2013;71:297-300.
8. Barquet A, Gelink A, Giannoudis PV. Proximal femoral fractures and vascular injuries in adults: Incidence, aetiology and outcomes. Injury 2015;46:2297-313.
9. Choy WS, Kim KJ, Lee SK, Yang DS, Jeung SW, Choi HG, et al. Surgical treatment of pathological fractures occurring at the proximal femur. Yonsei Med J 2015;56:460-5.
 |
 |
 |
 |
 |
 |
| Dr. Pedro Xavier Fernandes | Dr. Duarte Manuel Medeiros | Dr. Raquel C Teixeira | Dr. Andreia Mercier Nunes | Dr. Antonio Sousa Seco | Dr. Afonso Cevadinha Caetano |
| How to Cite This Article: Fernandes P X, Medeiros D M, Teixeira R C, Nunes A M, Seco A S, Caetano A C.Injury to the Superior Gluteal Artery during Intramedullary Fixation of a Proximal Femoral Fracture – A Case Report. Journal of Orthopaedic Case Reports 2019 Nov-Dec;9(6): 27-31. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




