[box type=”bio”] Learning Point of the Article: [/box]
Use of 3D printed custom-made jigs in difficult shoulder arthroplasty.
Case Report | Volume 10 | Issue 2 | JOCR March – April 2020 | Page 25-28 | Bharath Thati, Chandrasekhar Bodanki, Vamshi Kiran Badam, M V Reddy, A V Gurava Reddy. DOI: 10.13107/jocr.2020.v10.i02.1682
Authors: Bharath Thati[1], Chandrasekhar Bodanki[2], Vamshi Kiran Badam[2], M V Reddy[2], A V Gurava Reddy[2]
[1]Department of Orthopaedics, ASRAM Medical College, Eluru, Andhra Pradesh, India,
[2]Department of Orthopaedics, Sunshine Hospitals, Secunderabad, Telangana, India.
Address of Correspondence:
Dr. Bharath Thati,
Department of Orthopaedics, ASRAM Medical College, Eluru, Andhra Pradesh – 534005, India.
E-mail: thati.bharath@gmail.com
Abstract
Introduction: Complications of open reduction and internal fixation (ORIF) in four-part proximal humerus fractures (PHFs) include non-union, malunion, avascular necrosis of humeral head, and glenoid defect due to implant failure. Reverse total shoulder arthroplasty is a salvage procedure for cases of failed fixation. In cases with significant abnormal glenoid anatomy, custom-made patient-specific 3D printed jigs play a major role in pre-operative planning and accurate positioning of the glenoid component, thereby improving the final outcome. We report a case of salvage reverse shoulder arthroplasty done using the patient-specific custom-made 3D printed jig.
Case Report: A 58-year-old female sustained bilateral PHF due to electrocution and was treated with bilateral ORIF in single stage in February 2018.At 4 months from the time of surgery, the fracture on the left side had united, but there was non-union on the right side with screw penetration eroding the glenoid. Reverse shoulder arthroplasty was planned as a salvage procedure. Intraoperative, the glenoid was found to be small (2.7cm × 1.72cm) and there was a posterior glenoid defect due to screw penetration. During drilling for central peg, an iatrogenic glenoid fracture occurred. The procedure was deferred. After 4 months of conservative treatment, the glenoid fracture had united and then a definitive procedure with the reverse shoulder prosthesis was planned. 3D glenoid bone model was made based on the computed tomography scan and custom-made jigs are designed and 3D printed, which are specific for the patient. Reverse shoulder arthroplasty was done, and surgery went uneventful. The patient achieved active forward elevation of 110°, lateral elevation of 90°, and an external rotation of 10° at 1-year follow-up.
Conclusion: Reverse shoulder arthroplasty can be considered as a salvage procedure for failed fixation of PHF with predictable outcomes. Custom-made patient-specific 3D printed jigs in reverse shoulder arthroplasty are useful in assessing the position and direction of central peg in case of small glenoid and glenoid bone defects. 3D bone models are useful in implant selection also.
Keywords: 3D glenoid bone model, failed open reduction and internal fixation, 3D printed jigs, patient-specific instrumentation, salvage reverse shoulder arthroplasty.
Introduction
Proximal humerus fractures (PHFs) are the third most common fracture in adults, representing almost 6% of all adult fractures and half of the fractures of the humerus. They are typically associated with minimal trauma in the elderly, particularly in osteoporotic individuals [1]. The surgical management in this age group is challenging due to osteoporosis and multiple comorbidities [2]. Operative treatment of displaced four-part fractures often involves open reduction and internal fixation (ORIF). However, this is associated with complication and reoperation rates of up to 35% [3, 4]. Comminution of the fracture, osteoporosis, and poor surgical technique is the main reasons for loss of fixation. The development of avascular necrosis of the humeral head, iatrogenic screw perforation, and non-union are other complications, leading to pain and loss of function [5]. Available techniques for a failed fixation of PHF are redo fixation and arthroplasty. Joint preserving treatment, including reosteosynthesis and partial or total hardware removal, is not consistently been successful in addressing pain or restoring shoulder function [6], especially if there is glenoid destruction due to screw cutout or avascular necrosis of the humeral head. Hemiarthroplasty or total shoulder arthroplasty has shown acceptable clinical and radiographic outcomes after proximal humeral fracture but leaves some patients with residual pain and poor function. The primary determinant of function after hemiarthroplasty involves reliable fixation and healing of the tuberosity fragments. Non-union, malunion, or resorption of these fragments compromise post-operative outcomes [7]. Reverse total shoulder arthroplasty (RTSA) can address glenoid bone defects and at least partially compensate for muscle imbalance, hence, considered as salvage procedure for failed ORIF of proximal humeral fractures [8].
Case Report
A 58-year-old female has sustained bilateral PHF in February 2018 due to electrocution. She was treated with ORIF with locking plate of both proximal humeri in a single stage. At 4-month follow-up, the left side fracture has united but on the right side, there was non-union with collapse of head and penetration of screw (Fig. 1). The patient is symptomatic with pain and inability to lift her right shoulder. The patient was advised computed tomography(CT) scan with 3D reconstruction of the right shoulder and nerve conduction studies to assess the deltoid function. After pre-operative evaluation, the patient was planned for reverse shoulder arthroplasty.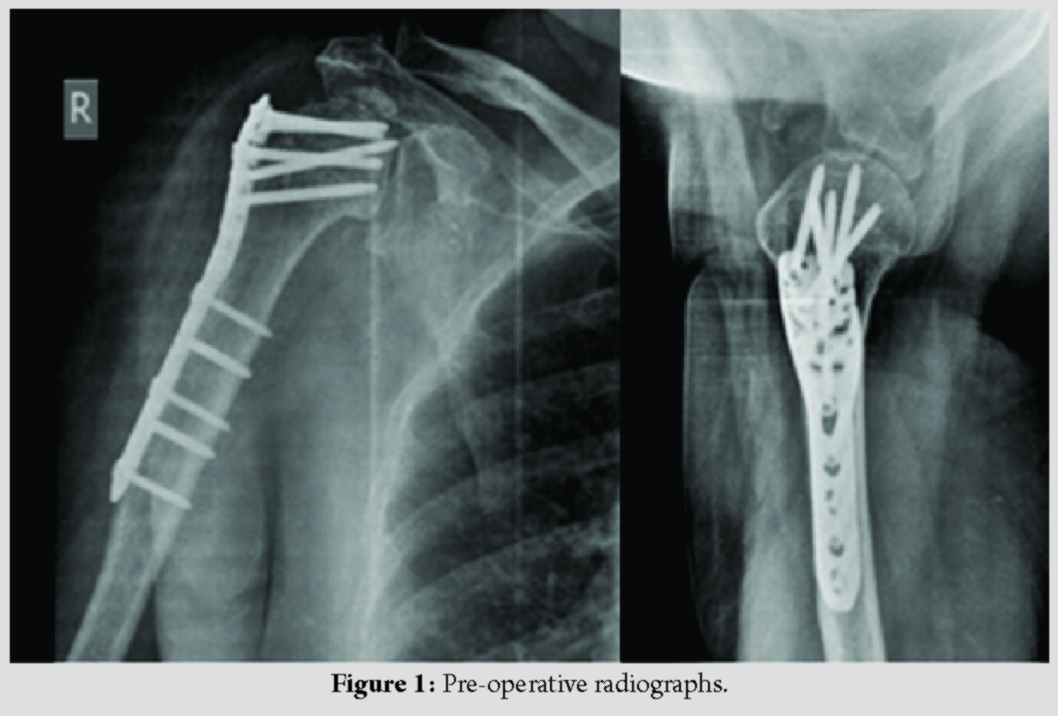
Under interscalene block, implant removal was done. There was posterior glenoid erosion due to screw penetration and glenoid was smaller than normal with a size of 2.7cm (superoinferior) × 1.72cm (anteroposterior). During drilling for the central peg, there was an iatrogenic glenoid fracture which was undisplaced. Due to the fracture, the procedure was abandoned, and we decided to treat the glenoid fracture conservatively with immobilization (Fig. 2). Reverse shoulder replacement was deferred till glenoid fracture union.
After 4 months, a CT scan with 3D reconstruction of the right shoulder was done and glenoid fracture union was confirmed (Fig. 3). Definitive RTSA is planned. However, the anticipated problems were (1) small size glenoid and difficulty to find enough space for the central screw and at least two peripheral screws. (2) As the glenoid vault was narrow, precise placement of the central screw to have good bone purchase was a challenge.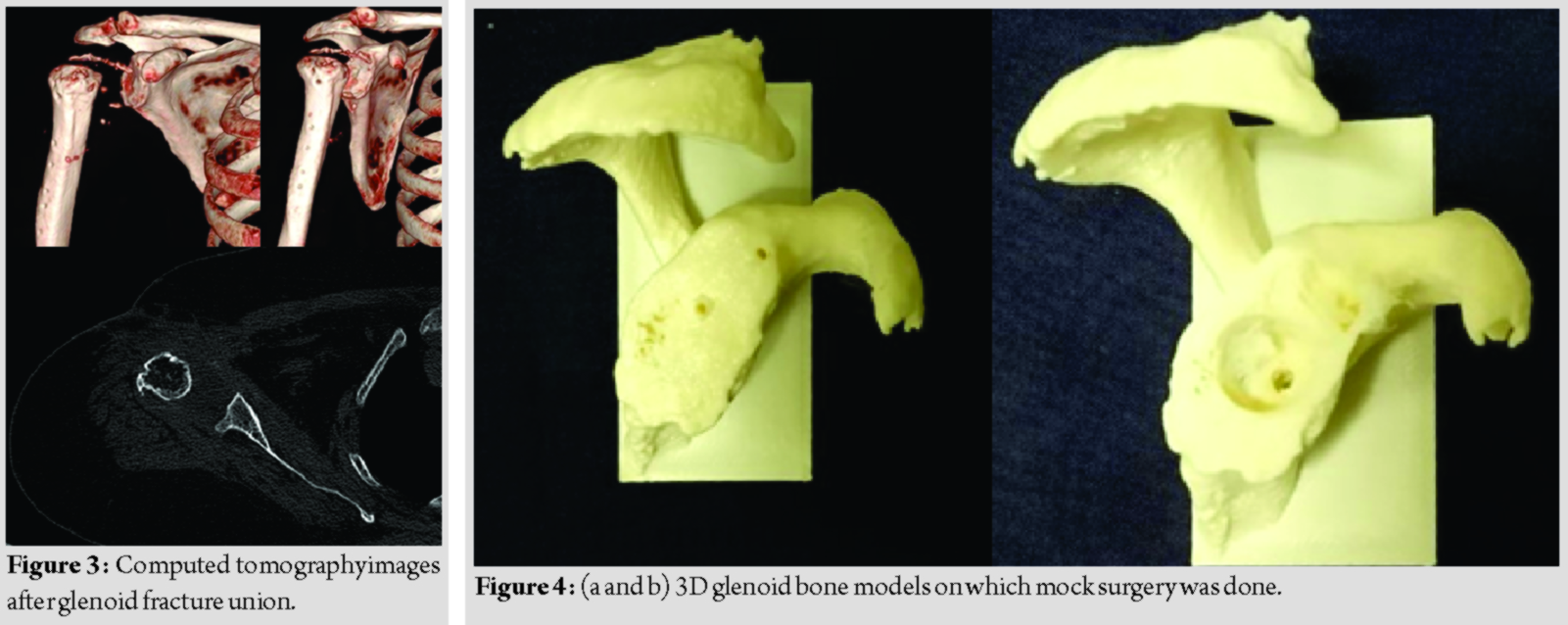
The patients glenoid is 3D printed for accurate assessment. Patient-specific jig is 3D printed based on required position and depth of central peg. Mock surgery was done with the 3D printed jig on the 3D printed glenoid to assess the accuracy of position, direction, and depth of the central peg (Fig. 4). Preoperatively, we templated base plate on the patient 3D glenoid bone model and decided to use BIOMET comprehensive reverse shoulder system with mini base plate.
The custom-made jigs were ETO (Ethylene Oxide) sterilized and used intraoperatively for making the central hole in the glenoid to find a good position and direction of central peg to accommodate a good length of the 6.5mm central screw (Fig. 5). Glenoid reaming was done and a 25mm mini base plate with peg of outer diameter 11mm and length of 8mm was used. A 6.5mm central screw with 35mm length was used. Two peripheral screws of 4.75mm size with length of 25mm and 20mm, respectively, were used to fix the base plate. The remaining part of surgery went uneventful (Fig. 6). 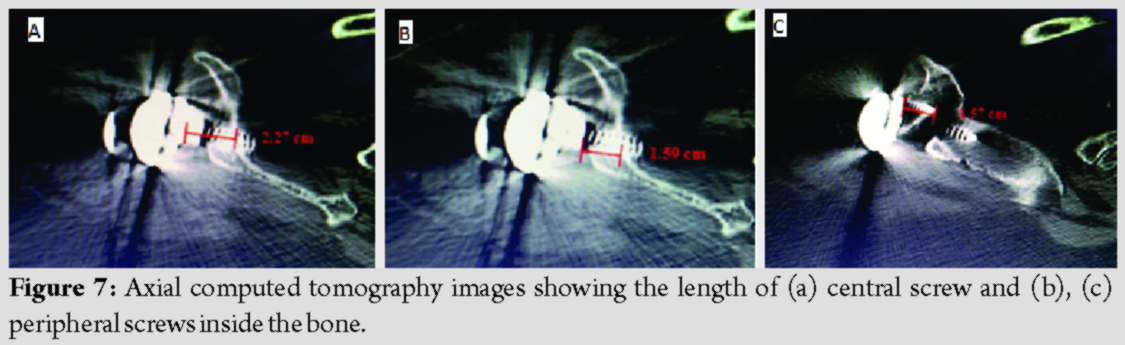
The stability and range of motion were assessed to be satisfactory intraoperatively. CT scan with 3D reconstruction was done in immediate post-operative period and at 3-month follow-up. It is found that 2.27 cm length of the central screw (Fig. 7a), and 1.57 cm and 1.59 cm length of the two peripheral screws (Fig. 7b, 7c) were inside the glenoid vault and are in the exact position as desired. On regular follow-up, the patient has a stable shoulder with active forward elevation of 110°, lateral elevation of 90°, and an external rotation of 10° at 1-year follow-up (Fig. 8).
Discussion
The design of the RTSA provides a stable and fixed fulcrum for elevation while increasing the moment arm and the resting tone of the deltoid muscle. As a result, it allows improved arm elevation and abduction despite a non-functional rotator cuff [9]. RTSA has been popularized for addressing a wide variety of shoulder conditions which include glenohumeral arthritis, rotator cuff arthropathy, failed conventional total shoulder arthroplasty, fracture sequelae, rheumatoid arthritis with irreparable rotator cuff tears, proximal humerus tumors, and PHF [10]. Biomechanical and clinical studies have shown that glenoid component positioning is important for good clinical outcome in RTSA [11]. However, pathologic glenoid with bone deformities and bone defects makes it difficult for the surgeon to identify anatomical landmarks, which can compromise accurate positioning of the central peg screw [11]. The glenoid 3D model can be a useful tool for pre-operative planning in RSA, particularly when dealing with bone loss so that the appropriate position, direction, and depth of the central peg screw can be decided. In our patient, even though the bone defect or the deformity was not very significant, the glenoid itself was very small to use the standard jigs or freehand technique to identify the exact placement of central peg of the base plate. Thus, we have used custom-made patient-specific 3D printed jigs. The use of custom 3D printed models of patient bone will help us in pre-operative planning, surgical simulation, intraoperative guidance, and implant development [12]. Patient-specific instrumentation (PSI) is a newer technique in the shoulder (first commercialized in 2013), and many major prosthesis companies have by now developed their own philosophy and promoted this solution. Developments in this area have resulted in a custom-made guide for the positioning of the glenoid component. PSI is an example of the evolution toward personalized treatment that occurs in all fields of medicine. PSI when compared with standard instrumentation improves glenoid component positioning during shoulder arthroplasty [13].
Conclusion
The use of custom-made jigs in reverse shoulder arthroplasty is useful in precise positioning and direction of central peg screw in case of small glenoid. This case report shows satisfactory outcome following reverse shoulder arthroplasty with 3D printed custom-made jigs. In salvage procedures, where there will be abnormal glenoid anatomy, custom-made patient-specific 3D printed jigs are useful in avoiding intraoperative complications and precise placement of base plate in reverse shoulder arthroplasty.
Clinical Message
Custom-made 3Dprinted jigs can be useful in patients with small glenoid, deformed glenoid, or glenoid with bone defects. This can be done by the individual surgeon with knowledge of 3D planning and printing or with the help of the implant companies providing specific instrumentation.
References
1. Dixit A, Cautela FS, Cooper CS, Beyer GA, Messina JC, Mait JE, et al. ORIF versus arthroplasty for open proximal humerus fractures: Nationwide inpatient sample data between 1998 and 2013. J Orthop Traumatol 2018;19:12.
2. Calvo E, Morcillo D, Foruria AM, Redondo-Santamaría E, Osorio-Picorne F, Caeiro JR, et al. Nondisplaced proximal humeral fractures: High incidence among outpatient-treated osteoporotic fractures and severe impact on upper extremity function and patient subjective health perception. J Shoulder Elbow Surg 2011;20:795-801.
3. Konrad G, Bayer J, Hepp P, Voigt C, Oestern H, Kääb M, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Surgical technique. J Bone Joint Surg Am 2010;92:85-95.
4. Owsley KC, Gorczyca JT. Fracture displacement and screw cutout after open reduction and locked plate fixation of proximal humeral fractures [corrected]. J Bone Joint Surg Am 2008;90:233-40.
5. Clavert P, Adam P, Bevort A, Bonnomet F, Kempf JF. Pitfalls and complications with locking plate for proximal humerus fracture. J Shoulder Elbow Surg 2010;19:489-94.
6. Jost B, Spross C, Grehn H, Gerber C. Locking plate fixation of fractures of the proximal humerus: Analysis of complications, revision strategies and outcome. J Shoulder Elbow Surg 2013;22:542-9.
7. Ferrel JR, Trinh TQ, Fischer RA. Reverse total shoulder arthroplasty versus hemiarthroplasty for proximal humeral fractures: A systematic review. J Orthop Trauma 2015;29:60-8.
8. Hussey MM, Hussey SE, Mighell MA. Reverse shoulder arthroplasty as a salvage procedure after failed internal fixation of fractures of the proximal humerus: Outcomes and complications. Bone Joint J 2015;97-B:967-72.
9. Holschen M, Franetzki B, Witt KA, Liem D, Steinbeck J. Is reverse total shoulder arthroplasty a feasible treatment option for failed shoulder arthroplasty? A retrospective study of 44 cases with special regards to stemless and stemmed primary implants. Musculoskelet Surg 2017;101:173-80.
10. Westermann RW, Pugely AJ, Martin CT, Gao Y, Wolf BR, Hettrich CM. Reverse shoulder arthroplasty in the United States: A comparison of national volume, patient demographics, complications, and surgical indications. Iowa Orthop J 2015;35:1-7.
11. Rodríguez JA, Entezari V, Iannotti JP, Ricchetti ET. Pre-operative planning for reverse shoulder replacement: The surgical benefits and their clinical translation. Ann Joint2019;4:4.
12. Eltorai AE, Nguyen E, Daniels AH. Three-dimensional printing in orthopedic surgery. Orthopedics 2015;38:684-7.
13. Villatte G, Muller AS, Pereira B, Mulliez A, Reilly P, Emery R. Use of patient-specific instrumentation (PSI) for glenoid component positioning in shoulder arthroplasty. A systematic review and meta-analysis. PLoS One 2018;13:e0201759.
 |
 |
 |
 |
 |
| Dr. Bharath Thati | Dr. Chandrasekhar Bodanki | Dr. Vamshi Kiran Badam | Dr. M V Reddy | Dr. A V Gurava Reddy |
| How to Cite This Article: Thati B, Bodanki C, Badam VK, Reddy MV, Reddy AVG. Custom 3D Printed Jigs in Salvage Reverse Shoulder Arthroplasty for Failed Four-Part Proximal Humerus Fracture Fixation: A Case Report. Journal of Orthopaedic Case Reports 2020 Mar-Apr;10(2): 25-28. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




