[box type=”bio”] Learning Point of the Article: [/box]
Leprosy disease may involve large joints also like hip joint and therefore staged total hip arthroplasty can be considered as a treatment option.
Case Report | Volume 10 | Issue 3 | JOCR May – June 2020 | Page 71-75 | Romit Agrawal, Vijay Singh, Ayush Sharma, Nilesh Mangale. DOI: 10.13107/jocr.2020.v10.i03.1756
Authors: Romit Agrawal[1], Vijay Singh[1], Ayush Sharma[1], Nilesh Mangale[1]
[1]Department of Orthopaedic Surgery, Dr. B.R Ambedkar Central Railway Hospital, Byculla, Mumbai, Maharashtra, India.
Address of Correspondence:
Dr. Romit Agrawal,
Department of Orthopaedic Surgery, Dr. B.R Ambedkar Central Railway Hospital, Byculla, Mumbai, Maharashtra, India.
E-mail: romitagrawal2588@gmail.com
Abstract
Introduction: Leprosy is a chronic granulomatous infection, classically presents with cutaneous and neurological manifestations. Joint involvement in leprosy can present as acute symmetrical or chronic polyarthritis with or without tenosynovitis resembling rheumatoidarthritis.
Case Report: We report a rare case of lepromatous hip arthritis in a 32-year-old male, known case of leprosytenosynovitis and symmetrical polyarthritis of hands and feet 3 weeks after appearance of typical cutaneous lesion. The patient was started on anti-leprosy and steroid treatment. After 9 months of treatment and recurrent exacerbation of symptoms, the patient developed bilateral hip pain. Hip pain was diagnosed as bilateral avascular necrosis hip on magnetic resonance imaging which progressed to the left hip arthritis later on. The patient underwent staged total hip arthroplasty (THA) for the left hip arthritis, with debridement and antibiotic spacer in the first stage and final hip prosthesis in the second stage.
Conclusions: Leprosy can present with large joint-like hip involvement including tenosynovitis and acutesymmetrical polyarthritis. Two-stage THA is an alternative treatment option for patients with advanced arthritis of the hip under some difficult conditions. The Harris hip score was increased from 35 preoperatively to 91.5 at the final follow-up.
Keywords: Leprosy arthritis, Hip Arthroplasty in leprosy, articular involvement, Charcot’s arthropathy.
Introduction
Leprosy is a chronic infectious disease caused by leprosy bacillus, which mainly damages the skin and peripheral nerves, and can also invade visceral and bone joints. Arthritis is a common feature of leprosy and contributes to disability. Direct invasion of joints and bones by mycobacteria may lead to a destructive arthritis in lepromatous disease. The infective process may involve few or many joints. In both, type 1 reaction of borderline case and the type 2 reaction of the lepromatous disease, intense inflammation may occur at sites of infection. The immunology of the reactions is different, but they may have same clinical features including a polyarthritis which may resemble rheumatoid disease [1]. We report such rare cases of hip arthritis secondarily to leprosy bacilli. To the best of our knowledge, this is the first case report of leprosy involving large joints.
Case Report
We report a rare case of a 32-year-old male, a known case of leprosy presented to our tertiary hospital in February 2017 with pain, swelling, burning sensation, and numbness of multiple joints. The pain started on his ankle and feet, with both hands and feet numbness 9 months ago. Joints swelling and pain gradually developed in the metacarpo-phalangeal joints, proximal inter phalangeal joints, and wrist joints with decreased hand grip (Fig. 1). He also had recurrent episodes of low-grade fever and large maculopapular skin lesions (approximately 5 cm in diameter) which was hypopigmented, with a roughly symmetric distribution, scattered throughout the back and arms, with central hypoesthesia. He had no painful or thickened nerve roots. Tenderness over right ulnar nerve and left common peroneal nerve were present.

Laboratory investigations revealed white blood cell count of 36,800 (normal 4000–10,000) (93% neutrophils), hemoglobin of 7.9 g/dl (mean corpuscular volume of 74.6 and mean corpuscular hemoglobin of 22.3), and platelet counts of 656,000. Inflammatory markers were raised (C-reactive protein [CRP] of 61 mg/l and erythrocyte sedimentation rate [ESR] of 87 mm/1 h). Blood and urine culture did not grow any organism. Further investigation revealed negative anti-nuclear antibody, rheumatoid factor (RF), anti-cyclic citrullinated peptide (CCP), and normal complements. X-rays of hands and foot were normal.
Electromyogram and nerve conduction velocity indicated Mononeuritis multiplex affecting the nerves with preserved “H” reflexes suggestive of Hansen disease.
The patient was started on anti-leprosy drugs (dapsone, rifampicin, and clofazimine) which resulted into gradual improvement of skin lesions, but there was persistence of articular symptoms. Later during the course of treatment, he was started on oral steroid in view of CPN neuritis. The patient had regular follow up in the outpatient clinic with infectious disease physician. Steroid was tapered slowly and the patient was improved clinically. Four months after initiation of treatment, the patient developed involvement of multiple joints including bilateral hip pain which was referred to knees (more on the left side).
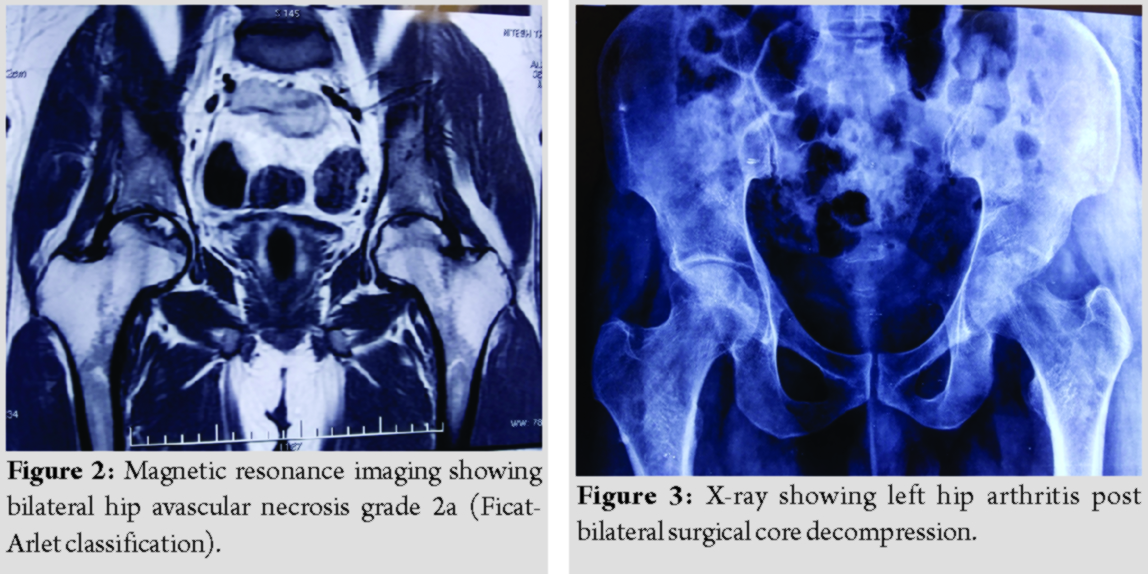
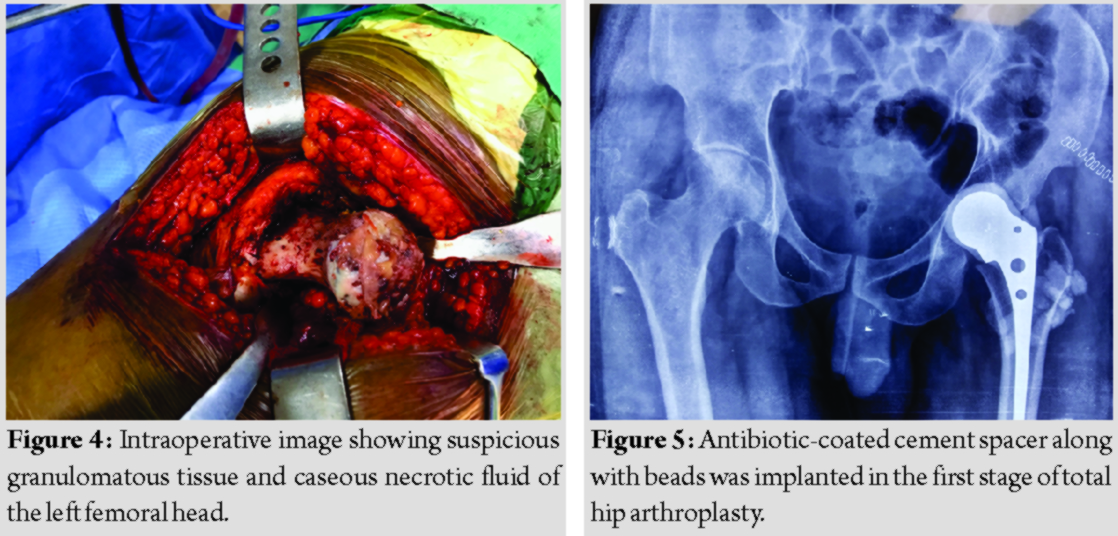
Magnetic resonance imaging was suggestive of bilateral grade 2a avascular necrosis hip (Ficat-Arlet classification) (Fig. 2) for which he underwent bilateral core decompression with delayed weight-bearing initially. After that, the patient was improved symptomatically for 6 months but later on patient started aggravation of the left hip pain which was diagnosed as the left hip arthritis (Fig. 3) even though the patient had completed 13 months of anti-leprosy treatment till this time.

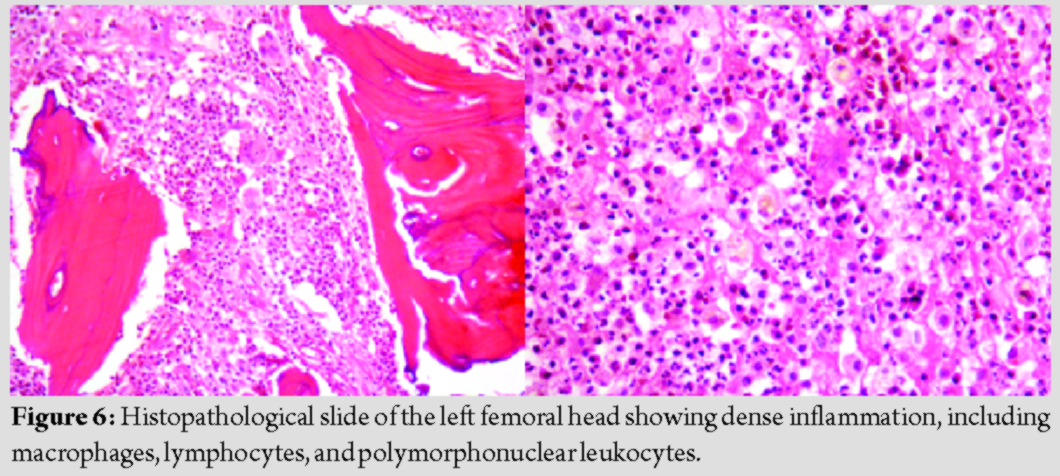
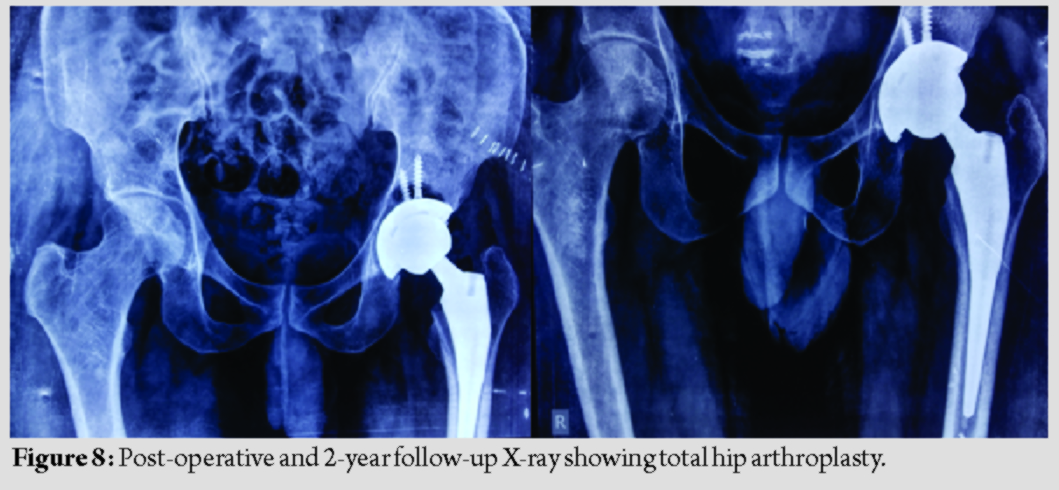
The patient was planned for total hip arthroplasty (THA) for the left hip arthritis and the patient was on anti-leprosy treatment, but intraoperative suspicious granulomatous tissue was observed and caseating necrotic fluid was present around the hip joint (Fig. 4);hence, planned THA was converted into staged THA with debridement and antibiotic spacer in the first stage and final hip prosthesis in the second stage. During the first stage, debridement was carried out to remove infected and necrotic tissues as thoroughly as possible. Antibiotic (vancomycin + gentamycin) coated cement spacer along with beads was implanted for 6 weeks (Fig. 5). These antibiotics were chosen empirically because we were not sure about the pathology of this infected tissue around the hip joint and leprosy being involving large joint is rare. Histopathological examination confirmed hip arthritis secondarily to leprosy (Fig. 6). During this time, the patient had continued anti-leprosy treatment. During the second stage, when the ESR and CRP were normal and the wound was well healed, antibiotic spacer was removed (Fig. 7) and final hip prosthesis was implanted. The patient was advised to continue with anti-leprosy treatment for 6 months. The patients were then evaluated based on the reactivation of infection, the Harris hip score system, X-ray, ESR, and CRP (Fig. 8).
Discussion
Musculoskeletal involvement in leprosy is the third most frequent manifestation after dermatological and neurological involvements. Leprosy must always be considered among the differential diagnoses of arthritis in endemic regions. In the literature, there are descriptions of patients with leprosy that was diagnosed with SLE, RA, dermatopolymyositis, and systemic vasculitis [2]. These manifestations occur mainly in multibacillary forms of leprosy, in reactional episodes and arise from infiltration and direct proliferation of the bacillus in the affected organ [2]. There are two types of immunologic reactions to Mycobacterium leprae antigens. These immunologic reactions can occur before, during, or after the treatment of leprosy.
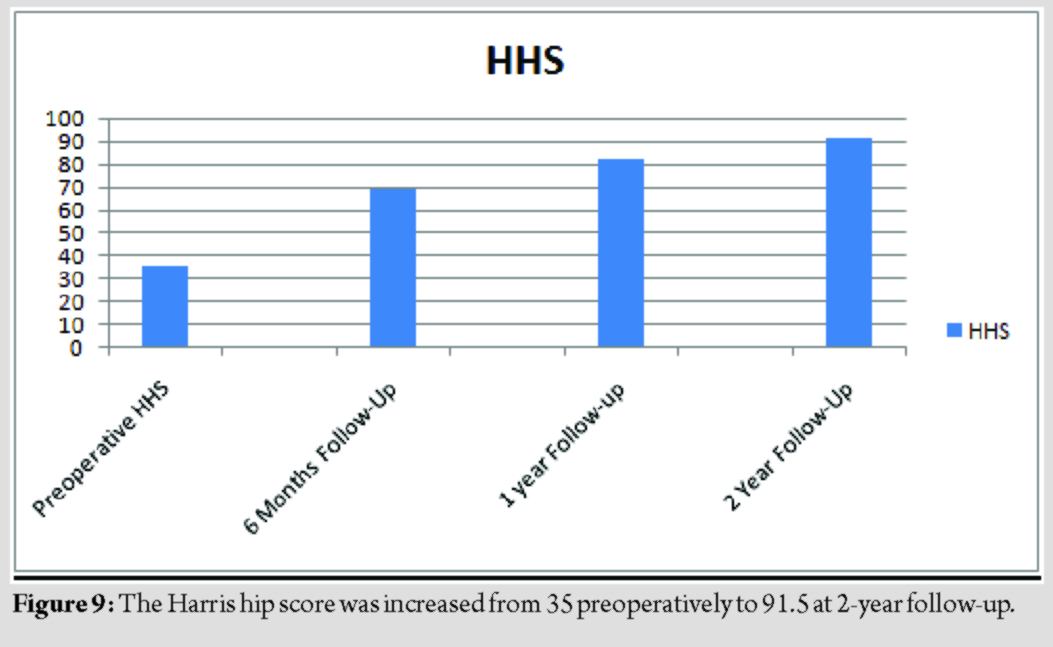
Type 1 lepra (Graham et al., 2010) [3] reaction is a delayed hypersensitivity reaction. It is a cell-mediated immune response to M. leprae antigenic determinants and is characterized by acute inflammation of pre-existing skin lesions or by the appearance of new lesions and/or neuritis. Systemic involvement does not occur in type 1 reaction. Type 2 lepra (Graham et al., 2010) [3] reaction also termed as erythema nodosum leprosum is an immune complex mediated (type 3 hypersensitivity) response to M. leprae antigenic determinants. It results in severe painful skin lesion, nerve damage, fever, and systemic manifestation. Systemic involvement can lead to arthritis, dactylitis, orchitis, uveitis, lymphadenitis, glomerulonephritis, proteinuria, and hepatitis. It occurs mostly during the 1styear of leprosy treatment. Chauhan et al. [4]classified the arthritis in leprosy into the following groups: (1) Charcot’s arthropathy secondary to peripheral sensory neuropathy; (2) swollen hands and feet syndrome; (3) acute polyarthritis of lepra reaction; and (4) chronic arthritis from direct infiltration of the synovium by lepra bacilli. Atkin et al. [5] conducted a study in 77 patients with leprosy. The study showed that 10 patients had generalized enthesitis and 20 patients had leprosy with manifestations of arthritis. Specific bony lesions in leprosy are rare with an incidence of between 3% and 5% among hospitalized patients and are mainly confined to the small bones of the face, hands, and feet [6]. In our patient, there is a presentation of small joints involvement first followed by skin lesion. Many times hip pain in known case of leprosy patient with a history of anti-leprosy and steroid drug intake for longer duration gives a picture of drug-induced secondary hip arthritis. Our patient presented with an acute onset of symmetrical polyarthritis and fever. High inflammatory markers, leukocytosis negative blood, and urine cultures are supporting evidence for type 2 lepra reaction [7]. Acute arthritis as well as enthesitis and tenosynovitis initially improved within a week after initiation of treatment. In recent times, primary articular involvement in leprosy, due to infiltration by M. leprae or as part of lepra reaction, has been recognized. The reported prevalence varies from 1% to 70% [8]. Acute and chronic symmetric polyarthritis involving hand joints, mimicking rheumatoid arthritis (RA), has also been described with or without lepra reaction [9]. Sometime, it is difficult to differentiate symmetrical polyarthritis due to leprosy from RA as in our patient. This question was entertained on initial presentation of our patient with symmetrical polyarthritis. Absence of rheumatoid nodule, extra-articular manifestation, patient being male, good response to anti-leprosy treatment, and absence of RF and anti-CCP are the clinical distinguishing features from RA in our patient [10]. Articular involvement in leprosy has been recognized since 600 B.C. in Chinese literature [11]. The two most common and well-recognized forms of articular involvement, neuropathic joints, and post-traumatic septic arthritis occur as a consequence of neuropathy [12 ,13]. Multidrug therapy is the mainstay of treatment. The current multidrug therapy recommended by the WHO in adults with MB disease is rifampicin 600 mg orally once a month, dapsone 100 mg orally daily, and clofazimine 300 mgorally once monthly with additional 50 mg daily. The WHO recommends that it should be continued for 12 months, but patients with initial high bacterial loads may need longer treatment. For paucibacillary disease (bacteriological index 2+), the regimen is rifampicin 600 mg orally once monthly and dapsone 100 mg orally daily for 6 months. Any patient who develops peripheral nerve damage during the past 6 months of treatment should receive a 4–6 months course of oral steroids. The surgical treatment for leprosy-induced hiparthritis includes debridement, arthrodesis, and resection arthroplasty combined with a certain period of anti-leprosy therapy. Arthrodesis is no longer popular in the Asia-Pacific region because of the customary need for squatting, kneeling, and sitting cross-legged. With the advent of improved chemotherapy and the distinct disadvantages of arthrodesis among the above population, this treatment is now practiced infrequently. Resection arthroplasty offers a painless and mobile hip, with removal of most of the infected tissues, and helps in eradicating the disease. However, a significant reduction in the limb and instability persists [14]. In addition, the conversion to THA after excision arthroplasty is complex and may be less satisfactory [14]. With the use of THA, hip arthritis secondary to leprosy in the quiescent stage has been successfully treated. The follow-up period was 2 years. No reactivation of leprosy or superimposed infection was observed. The ESR and CRP returned to the normal level with no liver injury. The Harris hip score was increased from 35 preoperatively to 91.5 at 2-year follow-up (Fig. 9). As far as we know, this is the first report focusing on two-stage THA for patients with advanced hip arthritis secondary to leprosy. With anti-leprosy medications, the two-stage THA protocol offers the greatest chance for the eradication of infection.
Conclusion
Leprosy can also involve large joints like hip along with tenosynovitis and acute symmetrical polyarthritis. This case report further expands the range of articular manifestations that can occur in leprosy. Staged total hip replacement with debridement and antibiotic spacer may be used as a treatment option for patients with advanced lepromatous hip arthritis.
Clinical Message
Leprosy disease should no longer be considered as a small joint disease. This case report shows that it can involve large joints also like hip joint. Staged THA should be considered as a treatment option in leprosy-induced hip arthritis.
References
1. Gibson T. Bacterial infections: The arthritis of leprosy. Baillieres Clin Rheumatol 1995;9:179-91.
2. Freire M, Carneiro HE, Teodoro RB, Cecin HA. Manifestacoes reumaticas na hanseniase: Dificuldades no diagnostico precoce. Rev Bras Reumatol 1998;38:210-4.
3. Graham A, Furlong S, Margoles LM, Owusu K, Franco-Paredes C. Clinical management of leprosy reactions. Infect Dis Clin Pract 2010;18:235–238.
4. Chauhan S, Wakhlu A, Agarwal V. Arthritis in leprosy. Rheumatology (Oxford, England) 2010;49:2237-42.
5. Atkin SL, El-Ghobarey A, Kamel M, Owen JP, Dick WC. Clinical and laboratory studies in patients with leprosy and enthesitis. Ann Rheum Dis 1990;49:715-7.
6. Dewi S, Setiyohadi B. Arthritis in leprosy without specific skin lesion. Indones J Rheumatol 2010;3:31-4.
7. Legendre DP, Muzny CA, Edwin S. Hansen’s disease (Leprosy): Current and future pharmacotherapy and treatment of disease-related immunologic reactions. Pharmacotherapy 2012;32:27-37.
8. Bonvoisin B, Martin JM, Bouvier M, Bocquet B, Boulliat J, Duivon JP. Articular manifestations in leprosy. Sem Hop 1983;59:302-5.
9. Gibson T, Ahsan Q, Hussein. Arthritis of leprosy. Br J Rheumatol 1994;33:963-6.
10. Alam F, Emadi SA. Case of arthritis secondary to leprosy. Springerplus 2014;3:734.
11. Messner RP. Arthritis due to mycobacteria, fungi and parasites. In: Arthritis and Allied Conditions. 13th ed. Maryland: Williams and Wilkins; 1997. p. 2305-20.
12. Crawford CL, Hardwicke PM. The Charcot foot. Lancet 2003;361:1225.
13. Gratacos J, Vila J, Brancos MA, Marco MA, Munoz Gomez J. Septic arthritis caused by group G Streptococcus in a female patient with lepromatous leprosy. Med Clin 1991;96:35-6.
14. Dallari D, Fini M, Carubbi C, Giavaresi G, Rani N, Del Piccolo N, et al. Total hip arthroplasty after excision arthroplasty: Indications and limits. Hip Int 2011;21:436-40.
 |
 |
 |
 |
| Dr. Romit Agrawal | Dr. Vijay Singh | Dr. Ayush Sharma | Dr. Nilesh Mangale |
| How to Cite This Article: Agrawal R, Singh V, Sharma A, Mangale N. Leprosy-induced hip arthritis: A rare case report. Journal of Orthopaedic Case Reports 2020 May-June;10(3): 71-75. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




