[box type=”bio”] Learning Point of the Article: [/box]
The physician should remember that the ulnar neurovascular bundle may be vulnerable to tension caused by severely displaced distal radius fracture.
Case Report | Volume 10 | Issue 4 | JOCR July 2020 | Page 25-30 | Mehmet Sukru Sahin, Kemal Gokkus, Mehmet Baris Sargin. DOI: 10.13107/jocr.2020.v10.i04.1786
Authors: Mehmet Sukru Sahin[1], Kemal Gokkus[1], Mehmet Baris Sargin[1]
[1]Department of Orthopaedics and Traumatology, Baskent University Alanya Research and Practice Center, Saray Mahallesi Yunus Emre Caddesi No 1, Alanya 07400, Antalya, Turkiye.
Address of Correspondence:
Dr. Kemal Gokkus, Department of Orthopaedics and Traumatology, Baskent University Alanya Research and Practice Center, Saray Mahallesi Yunus Emre Caddesi No 1, Alanya 07400, Antalya, Turkiye.
E-mail: kgokkus@gmail.com
Abstract
Introduction: Distal radius fractures are one of the most frequent traumas encountered in daily orthopedic practice. With this case report, we would like to emphasize the significance of an unexpected associated ulnar nerve and artery injury with distal radius fracture to physicians.
Case Report: A 56-year-old male patient was evaluated in the emergency room after a motorcycle accident. The left wrist had a deformity and swelling, and about 3 × 1.5 cm of superficial skin abrasion was found in the volar surface of the wrist. It was noted that distal pulses were palpable, no neurological damage was found except hypoesthesia in the 5th finger. Radiologic examination revealed that the right shoulder was dislocated, and there was a displaced comminuted distal radius fracture in the left wrist with a non-displaced fracture of the ulnar styloid. The fracture was treated with open reduction and internal fixation using volar anatomic plate through the volar approach. After the surgery, pre-operative numbness did not resolve and opposing that expected; it increases with associated pain on the ulnar nerve innervated area within 30 days. The electromyographic analysis revealed severe partial ulnar nerve injury. The surgical exploration of the nerve was decided. The ulnar nerve was found to be trapped in scar tissue, and intimal injury and consequent thrombosis were observed at the ulnar artery.
Conclusion: Distal radius fractures are well-known fractures among the orthopedic surgeons; median nerve compression with a fracture is also within the expectation of the physician. However, the injury of the ulnar nerve and artery is unexpected. With this case report, we would like to emphasize the awareness of the diagnosis and treatment of this kind of associated unexpected ulnar nerve and artery injuries.
Keywords: Distal radius fracture, ulnar nerve injury, Guyon’s canal, ulnar artery injury.
Introduction
Distal radius fractures are one of the most frequent traumas encountered in daily orthopedic practice. Approximately one-sixth of the fractures seen at the emergency rooms is distal radius fractures [1]. Although the most frequent neurological injury caused by these fractures is median nerve neuropathy, it has been reported in the literature that such fractures might cause ulnar nerve and artery injury. This study aims to share the case of the ulnar nerve and ulnar artery injury following a closed distal radius fracture due to high energy trauma and our approach to this patient.
Case Report
A 56-year-old male patient was evaluated in the emergency room after a motorcycle accident. In the patient’s physical examination, it was found that the right shoulder had an epaulet sign, the right arm was in external rotation and abduction, and the humeral head could be felt by deep palpation in the anterior part of the glenoid.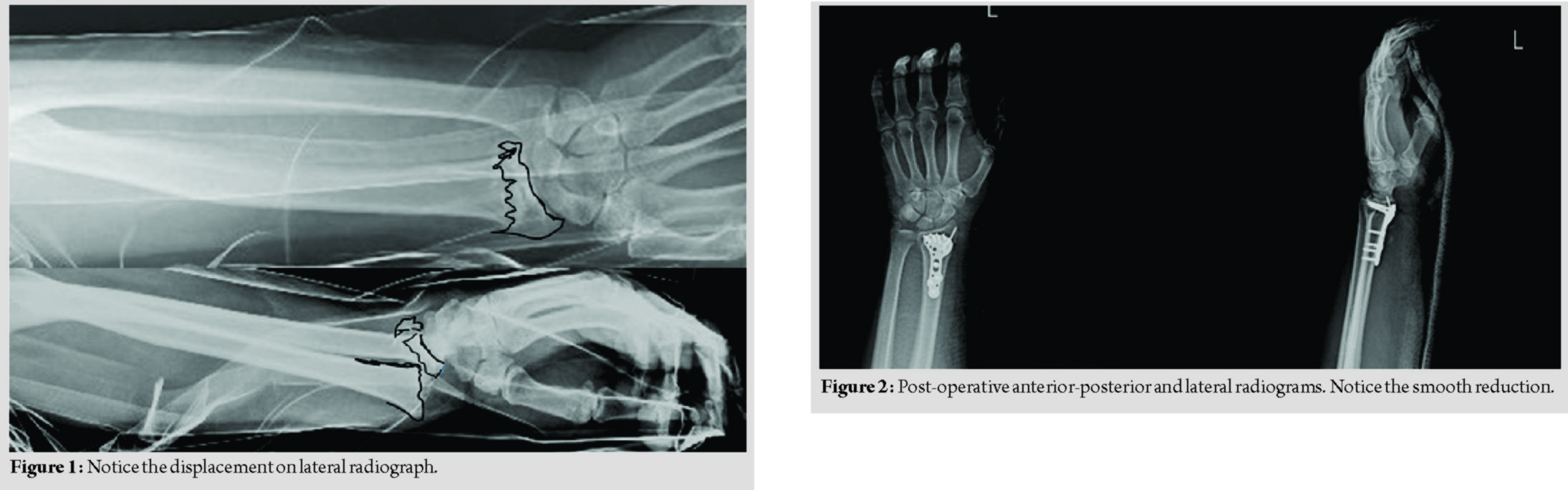
The left wrist had a deformity and swelling, and about 3 × 1.5 cm of superficial skin abrasion was found in the wrist’s volar surface. It was noted that distal pulses were palpable, no neurological damage was found except hypoesthesia in the 5th finger.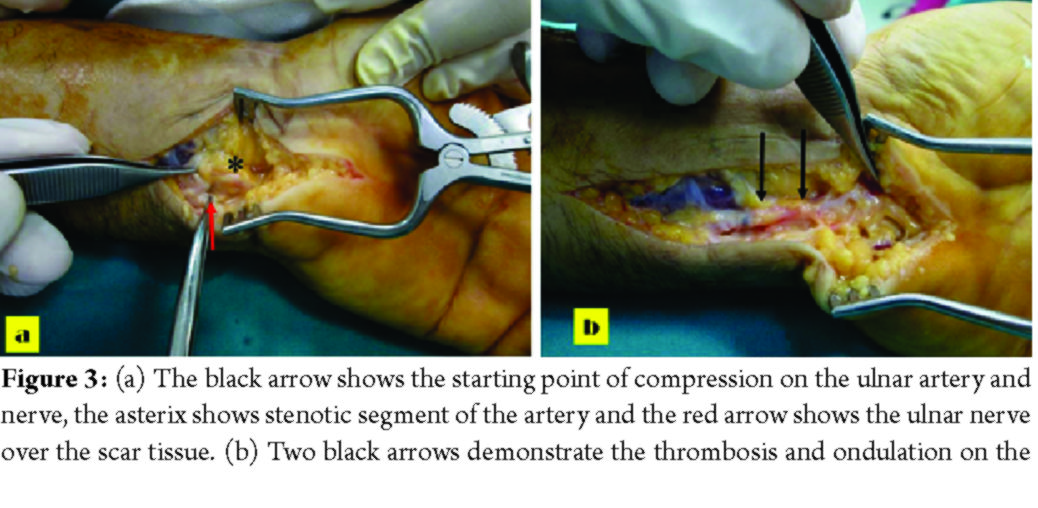
Radiologic examination revealed that the right shoulder was dislocated, and there was a dorsally displaced severely comminuted distal radius fracture in the left wrist with a non-displaced fracture of the ulnar styloid (Fig. 1). The dislocated right shoulder was reduced under sedoanalgesia. The patient was operated electively 1 day after the injury.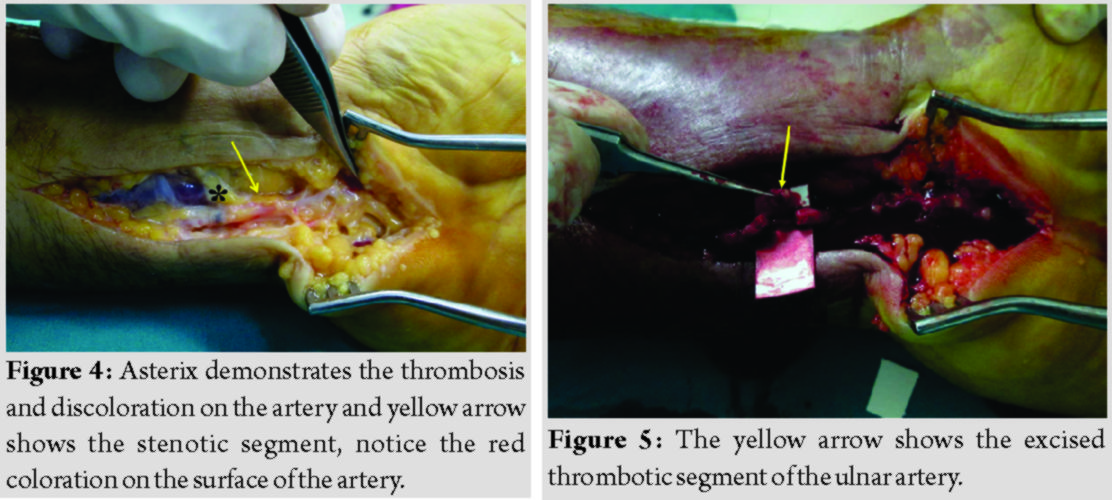
Under infraclavicular blockage anesthesia, with a pneumatic tourniquet inflated, approximately 10 cm skin incision was made on the volar aspect of the left wrist. The radial artery was explored and protected. After the fracture was reduced, it was temporarily fixed with 3 K-wires. Then, permanent fixation was achieved using a distal radius volar anatomic plate and screws (Fig. 2).
The patient had symptoms of paresthesia and severe pain on the 4th and 5th fingers at 10th-day follow-up after the procedure. He was closely monitored, as current symptoms did not improve, and electromyographic examination was obtained at the 4th week postoperatively. The electromyographic analysis revealed severe partial ulnar nerve injury. The surgical exploration of the nerve was decided. Approximately 10 cm incision was made on the ulnar aspect of the wrist’s volar part. The ulnar nerve and the ulnar artery were found trapped inside the scar tissue (Fig. 3).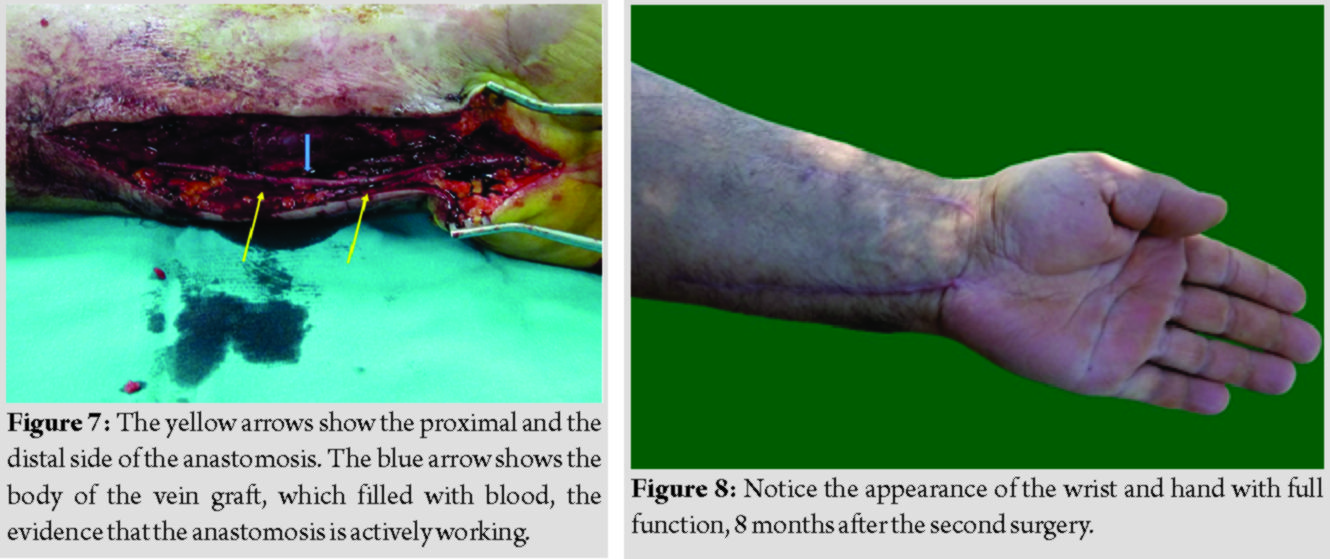
The compressed ulnar nerve was released. Intimal injury and consequent thrombosis were observed at the ulnar artery. The thrombosed segment was excised till to the edge of the healthy vascular intimal layer (Fig. 4). As the defect was approximately 5 cm, an anastomosis was planned with a vein graft from the forearm. About 8 cm of skin incision was made on the forearm’s volar side, 10 cm below the elbow joint, and 6 cm of vein graft was harvested from the basilic vein, reversed, and the defect was repaired with the graft (Fig. 5-7). The ulnar artery was also decompressed against the probability of further compression. Four weeks after the second operation, finger hypoesthesia started to improve, and clinically, the pain diminished, and wrist and hand functions became better (in complete comparison). The patient had full functionality and pain-free wrist without any neurovascular impairment; after the 8 months from the second surgery (Fig. 8-10).
Discussion
There have been the case reports and series regarding isolated ulnar nerve and ulnar artery injuries associated with distal radius fracture in the literature; however, and two authors have reported both artery and nerve injury. Regarding treatment and intraoperative findings, our report is unique in the literature. While distal radius fractures are rarely associated with neurological injuries, the median nerve is most commonly affected by this type of fracture. Its frequency has been reported in the literature ranging from 0.2% to 20% [2, 3, 4, 5, 6, 7, 8, 9]. In large series, ulnar nerve injury has been reported much less than the median nerve [2, 4, 6]. Isolated ulnar nerve injuries that reported in the literature mostly case reports (Table 1) [10, 11, 12, 13, 14, 15, 16, 17, 18, 19]. Zoëga (1966) observed ulnar nerve palsy in three patients after a closed distal radius fracture; he emphasized that the abnormal dorsoradial displacement of the fracture can cause tension due to the contact pressure of the proximal fragment [10]. Vance and Gelberman (1978) reported ulnar neuropathy in three cases following a distal fracture in the radius. Compared to the common era of distal radius fractures, all cases sustained high-energy injuries, and all of the fractures had a more marked dorsal displacement than standard Colles’ fracture [11]. In their anatomical study, they found that the ulnar nerve was approximately 2 mm close to the fragments in a dorsally displaced distal radius fracture, and they emphasized that in an isolated distal radius fracture, ulnar nerve damage might occur as contusion or being tethered by intact distal ulna [11]. Furthermore, ulnar sided-hematoma may compress the nerve in Guyon’s canal [11]. If a distal radius fracture is paired with a distal ulna fracture, the likelihood of ulnar nerve damage is higher [11]. They suggested that the ulnar nerve in Guyon’s canal was less exposed to pressure than the median nerve did in the carpal tunnel [11]. They also suggested that if there is ulnar nerve deficit due to a distal radius fracture, immediate the closed or open reduction should be performed, and later if the neurological deficit does not improve in 24–36 h, and surgical decompression will be mandatory [11]. In an anatomical analysis, Clarke and Spencer (1991) found that the ulnar nerve had more mobility and extensibility than the median nerve; thus, the ulnar nerve was possibly less damaged than the median nerve after distal radius fractures [20]. Soong and Ring (2007) found that median nerve entrapment and ulnar nerve injury due to distal radius fracture were associated with high energy. We also justified this hypothesis in our case. Comparing with median nerve compression, ulnar nerve compression was less commonly encountered [16]. Furthermore, they postulated that the secondary ulnar nerve injury was not correlated with the pressure phenomenon, in contrast with the median nerve. They disagreed with the idea that a displaced distal radius fracture was not very commonly associated with ulnar nerve injury; they argued that the ulnar nerve was more vulnerable to contusion and stretching than the median nerve due to its fixed position in the Guyon’s canal, but that, unlike the median nerve, the ulnar nerve was less affected by pressure-related injuries as it was outside of the carpal tunnel [16]. They recommended exploration of the nerve when there was a coexisting open wound with fracture associated with ulnar nerve injury; otherwise, close follow-up was recommended after the reduction [16]. In our case, the 5th finger had slightly hypoesthesia preoperatively, and we suggested that this was acute neuropraxia that could resolve spontaneously. In the post-operative 1 month follow-up, although the stretching effect of displaced fracture on the nerve resolved and hypoesthetic symptoms on the 4th and 5th fingers progressed. The decision of surgical exploration was made. The injury of both the ulnar nerve and ulnar artery after distal radius fracture has been reported very rarely in the literature [12, 21]. Poppi et al. (1978) made a surgical exploration while the symptoms of ulnar nerve entrapment that did not resolve after 3 months from the injury in a conservatively treated distal radius fracture; found that the ulnar nerve, artery, and veins were trapped in scar tissue and the ulnar artery was thrombosed. They released the ulnar nerve but did not give additional detail about the ulnar artery in the report [12]. This report seems very similar to ours, but in detail, they did not report any treatment regarding the artery. De Witte et al. (2008) published a series of six patients with vascular injury after distal radius fracture, which was treated with open reduction and volar plate fixation. In their series, they reported ulnar artery and ulnar nerve injury in two patients. In the first patient with ulnar nerve contusion and ulnar artery laceration, they preferred to perform ligation for the lacerated ulnar artery. The second patient had partial nerve laceration and ulnar artery thrombosis. They performed a repair of the nerve and reconstruction of the artery with a vein graft. They suggested that vascular injuries associated with distal radius fractures were higher than previously published, and the increased usage of the volar approach in fixation of such fractures was associated with more vascular injuries [21]. In their case, the ulnar nerve has been lacerated while, in our case, the ulnar nerve was trapped in scar tissue. This critical detail distinguishes this case from ours (Table 1). In our case, we did a surgical exploration and detected that the ulnar nerve was compressed inside the scar tissue, and the ulnar artery was thrombosed with segmental intimal damage. We performed decompression of the ulnar nerve and repaired the thrombosed ulnar artery with segmental resection and vein grafting.
Conclusion
Distal radius fractures are well-known fractures among the orthopedic surgeons; median nerve compression with a fracture is also within the expectation of the physician. However, the injury of the ulnar nerve and artery is unexpected. With this case report, we would like to emphasize the awareness of the diagnosis and treatment of this kind of associated unexpected ulnar nerve and artery injuries.
Clinical Message
Distal radius fractures are well-known fractures among orthopedic surgeons. However, associated injury of ulnar nerve and artery with a fracture is unexpected. The physician should keep in mind that the ulnar neurovascular bundle might be vulnerable to a tension caused by severely displaced distal radius fracture.
References
1. Jupiter JB. Fractures of the distal end of the radius. J Bone Joint Surg Am 1991;73:461-9.
2. Bacorn RW, Kurtzke JF. Colles’ fracture; a study of two thousand cases from the New York state workmen’s compensation board. J Bone Joint Surg Am 1953;35:643-58.
3. Lynch AC, Lıpscomb PR. The carpal tunnel syndrome and colles’ fractures. JAMA 1963;185:363-6.
4. Frykman G. Fracture of the distal radius ıncluding sequelae shoulder-handfinger syndrome, disturbance in the distal radio-ulnar joint and ımpairment of nerve function: A clinical and experimental study. Acta Orthop Scand 1967;38:1-61.
5. Aro H, Koivunen T, Katevuo K, Nieminen S, Aho AJ. Late compression neuropathies after colles’ fractures. Clin Orthop Relat Res 1988;233:217-25.
6. Hove LM. Nerve entrapment and reflex sympathetic dystrophy after fractures of the distal radius. Scand J Plast Reconstr Surg Hand Surg 1995;29:53-8.
7. Bienek T, Kusz D, Cielinski L. Peripheral nerve compression neuropathy after fractures of the distal radius. J Hand Surg Br 2006;31:256-60.
8. Ward CM, Kuhl TL, Adams BD. Early complications of volar plating of distal radius fractures and their relationship to surgeon experience. Hand (N Y) 2011;6:185-9.
9. Esenwein P, Sonderegger J, Gruenert J, Ellenrieder B, Tawfik J, Jakubietz M. Complications following palmar plate fixation of distal radius fractures: A review of 665 cases. Arch Orthop Trauma Surg 2013;133:1155-62.
10. Zoëga H. Fracture of the lower end of the radius with ulnar nerve palsy. J Bone Joint Surg Br 1966;48:514-6.
11. Vance RM, Gelberman RH. Acute ulnar neuropathy with fractures at the wrist. J Bone Joint Surg Am 1978;60:962-5.
12. Poppi M, Padovani R, Martinelli P, Pozzati E. Fracture of the distal radius with ulnar nerve palsy. J Trauma 1978;18:278-9.
13. Fernandez DL. Irreducible radiocarpal fracture-dislocation and radioulnar dissociation with entrapment of the ulnar nerve, artery and flexor profundus II-V-case report. J Hand Surg Am 1981;6:456-61.
14. Pazart F, Stindel E, Le Nen D. Fracture of the distal part of the radius associated with severed ulnar nerve. Chir Main 1999;18:197-201.
15. Lu CC, Chuo CY, Chen SK, Huang YH, Chou PH. Ulnar nerve palsy following fracture of the distal radius in an adolescent: A case report. Kaohsiung J Med Sci 2007;23:151-5.
16. Soong M, Ring D. Ulnar nerve palsy associated with fracture of the distal radius. J Orthop Trauma 2007;21:113-6.
17. Sohal JK, Chia B, Catalano LW 3rd. Dorsal displacement of the ulnar nerve after a displaced distal radius fracture: Case report. J Hand Surg Am 2009;34:432-5.
18. Cho CH, Kang CH, Jung JH. Ulnar nerve palsy following closed fracture of the distal radius: A report of 2 cases. Clin Orthop Surg 2010;2:55-8.
19. Rotman D, Schermann H, Kadar A. Displaced distal radius fracture presenting with neuropraxia of the dorsal cutaneous branch of the ulnar nerve (DCBUN). Arch Orthop Trauma Surg 2019;139:1021-3.
20. Clarke AC, Spencer RF. Ulnar nerve palsy following fractures of the distal radius: Clinical and anatomical studies. J Hand Surg Br 1991;16:438-40.
21. de Witte PB, Lozano-Calderon S, Harness N, Watchmaker G, Green MS, Ring D. Acute vascular injury associated with fracture of the distal radius: A report of 6 cases. J Orthop Trauma 2008;22:611-4.
 |
 |
 |
| Dr. Mehmet Sukru Sahin | Dr. Kemal Gokkus | Dr. Mehmet Baris Sargin |
| How to Cite This Article: Sahin MS, Gokkus K, Sargin MB. Ulnar Nerve and Ulnar Artery Injury Caused by Comminuted Distal Radius Fracture. Journal of Orthopaedic Case Reports 2020 July;10(4): 25-30. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




