[box type=”bio”] Learning Point of the Article: [/box]
A neglected Pipkin type IV injury of the hip can be given a trial of joint preservation surgery even in older age group especially in Indian scenario.
Case Report | Volume 10 | Issue 4 | JOCR July 2020 | Page 38-41 | Rakesh Goyal, Neel M Bhavsar, Akash Goel, Nishant Bhatia, Anurag Mehndiratta, Shakti A Goel. DOI: 10.13107/jocr.2020.v10.i04.1792
Authors: Rakesh Goyal[1], Neel M Bhavsar[2], Akash Goel[3], Nishant Bhatia[3], Anurag Mehndiratta[4], Shakti A Goel[5]
[1]Department of Orthopaedics, Sports Injury Centre, Vardhman Mahavir Medical College and Safdarjung Hospital New Delhi, India,
[2]Department of Orthopaedics, Sardar Vallabhbhai Patel Institute of Medical Sciences and Research, Ahmedabad, Gujarat, India,
[3]Department of Orthopaedic Surgery, Maulana Azad Medical College and Associated Lok Nayak Hospital, New Delhi, India,
[4]Department of Radiodiagnosis, Maulana Azad Medical College and Associated Lok Nayak Hospital, New Delhi, India,
[5]Indian Spinal Injury Centre, New Delhi, India.
Address of Correspondence:
Dr. Nishant Bhatia,
Department of Orthopaedic Surgery, Maulana Azad Medical College and Associated Lok Nayak Hospital, New Delhi, India.
E-mail: bhatianishant1111@gmail.com
Abstract
Introduction: Hip joint fracture-dislocations are rare injuries and usually result from high energy trauma. Femoral head fractures account for only 7–16% of all hip fracture-dislocations. There is always a controversy regarding optimal surgical treatment modality and approach for the treatment of Pipkin type IV fractures. In a 60 years old individual, various reports favor primary hip arthroplasty as compared to open reduction and internal fixation (ORIF). The posterior approach is preferred because it provides adequate exposure of the acetabular fracture and an opportunity for simultaneous repair of the femoral head and acetabular fractures. Another benefit is that anterior vascular supply to the femoral head and abductor function can be preserved.
Case Report: In this case report, we present a neglected 15 days old rare injury (Pipkin type IV femoral head fracture) in a 60 years old male patient that was given a trial of hip preservation surgery by ORIF through posterior (Kocher-Langenbeck) approach.
Conclusion: A neglected case of Pipkin type IV injury with chances of avascular necrosis and arthritis can be given a trial of hip preservation surgery because in an Indian scenario sitting cross legged and squatting are indispensable activities of daily lifestyle and appropriate surgical technique, adequate exposure, anatomic reduction, and stable internal fixation of the fractures are critical to achieve satisfactory clinical results.
Key words: Acetabulum, Dislocation, Fracture, Neglected, Pipkin IV.
Introduction
Hip joint fracture-dislocations are rare injuries and usually result from high-energy trauma. Femoral head fractures account only 7–16% of all hip fracture-dislocations [1, 2, 3, 4]. Combined femoral head and acetabular fractures (Pipkin IV) are relatively rare injuries and have an incidence of one in 7–1 in 15 traumatic hip dislocations [2, 3, 5, 6, 7]. They occur as a shearing injury as the flexed femoral head is forced on the posterior wall of the acetabulum causing facture dislocation [2]. There is always a controversy regarding optimal surgical treatment modality and approach for the treatment of Pipkin type IV fractures. Recent literature favors primary hip replacement as compared to open reduction and internal fixation (ORIF) in age above 55–60 years due to high chances of avascular necrosis and arthritis [8, 9]. Several surgical approaches have been described for both ORIF and replacement, including posterior, anterior, and anterolateral approaches [10, 11, 12, 13, 14]. The posterior approach provides adequate exposure of the acetabular fracture and an opportunity for simultaneous repair of the femoral head and acetabular fractures. Another benefit is that anterior vascular supply to the femoral head and abductor function can be preserved. On the other hand, main advantage of the anterior approach is the provision of good exposure, reduced operative time and blood loss, and thereby reduced incidence of postoperative avascular necrosis of the femoral head but its drawback is higher incidence of heterotrophic ossification [13, 14, 15, 16]. We went ahead with ORIF through the posterior Kocher-Langenbeck approach (to preserve whatever anterior blood supply was left) for this neglected 15 days old Pipkin type IV fracture dislocation. As the patient was a farmer by occupation, squatting and crossed leg sitting were important activities for him to earn his livelihood and hence after discussing with the patient it was decided to give a trial of hip preservation surgery. Though Pipkin type IV variety is not only uncommon but also it is not frequently seen and this was a neglected unstable case hence, making it a challenging entity which was managed successfully with traction followed by fixation.
Case Report
In 2015, a 60 years old male patient presented to the hospital with complaints of pain and swelling in right hip region and inability to bear weight on right lower limb for 15 days. Patient had history of motor vehicle accident and sustained injury to the right hip region. He had not taken any treatment previously and presented to us for the 1st time. On clinical examination, right lower limb was adducted and internally rotated. Movements at right hip joint were painful and restricted. Swelling was present in right gluteal region and vascular sign of Narath was positive. Distal neurovascular structures were intact. Radiograph of right hip revealed posterior dislocation and femoral head fracture with a large intra-articular fragment. There was disruption of posterior acetabular wall with a displaced acetabular fragment posterosuperiorly. The ilioischial and iliopectineal lines were intact as was the obturator ring. The femoral neck was also intact (Fig. 1).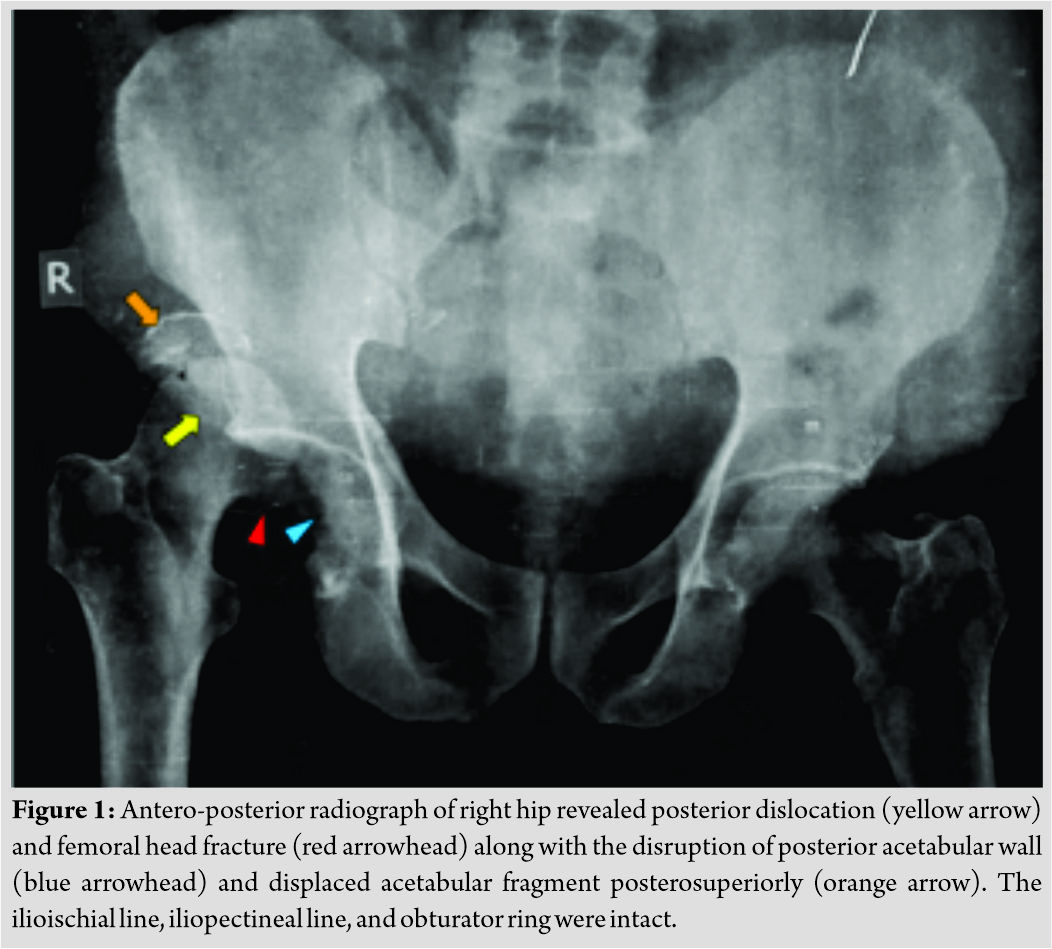
Pre-reduction non-contrast computed tomography scan was performed for further evaluation. Images were reconstructed in bone window and volume rendered images were also obtained. The study confirmed the findings of radiography and revealed right posterior hip dislocation with femoral head fracture confined to the part of head caudal to Fovea Centralis. There was a coexisting isolated acetabular posterior wall fracture. Hence, the lesion was classified as Pipkin type IV (Fig. 2).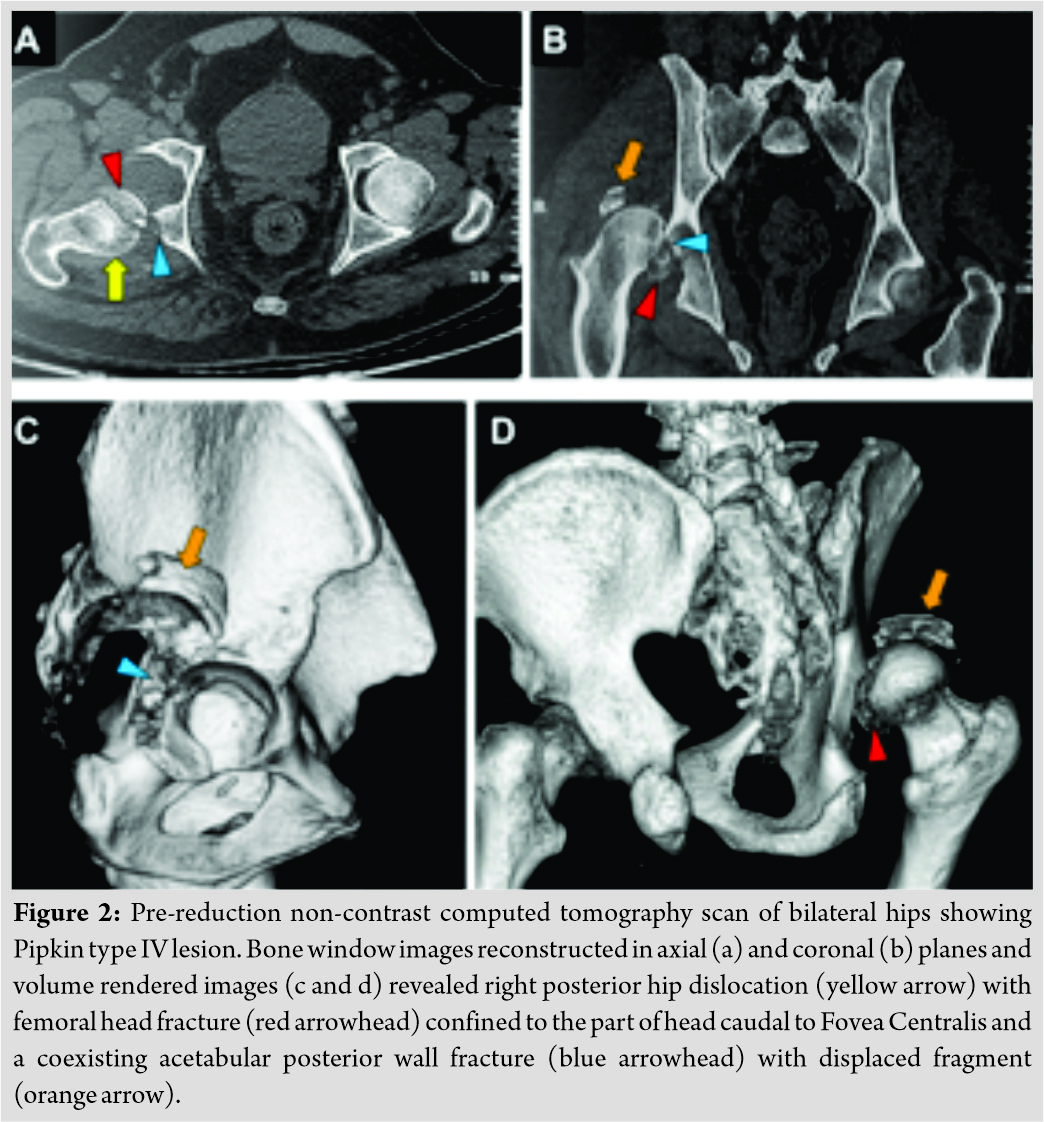
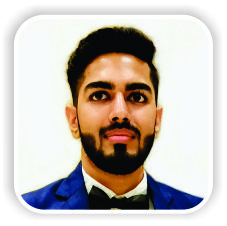
Reduction of hip dislocation was attempted in emergency room but found to be unstable. Patient was kept on skeletal traction for 24–48 h and subsequently planned for open reduction and internal fixation. Kocher-Langenbeck approach was used which allowed direct visualization of the dorso-cranial part of acetabulum. Femoral head fracture was fixed using Herbert screw and recon plate and spring hook plates were used to fix acetabular fracture fragment and to stabilize the reduction (Fig. 3). Post-operative period was uneventful. Hip joint was kept in abduction and slight external rotation for optimal healing while allowing controlled flexion and extension. Hip muscles strengthening exercises were started slowly and gradually as tolerated by the patient. Bony union was noted 12 weeks postoperatively (Fig. 4) and after 14 weeks patient was able to sit and squat easily.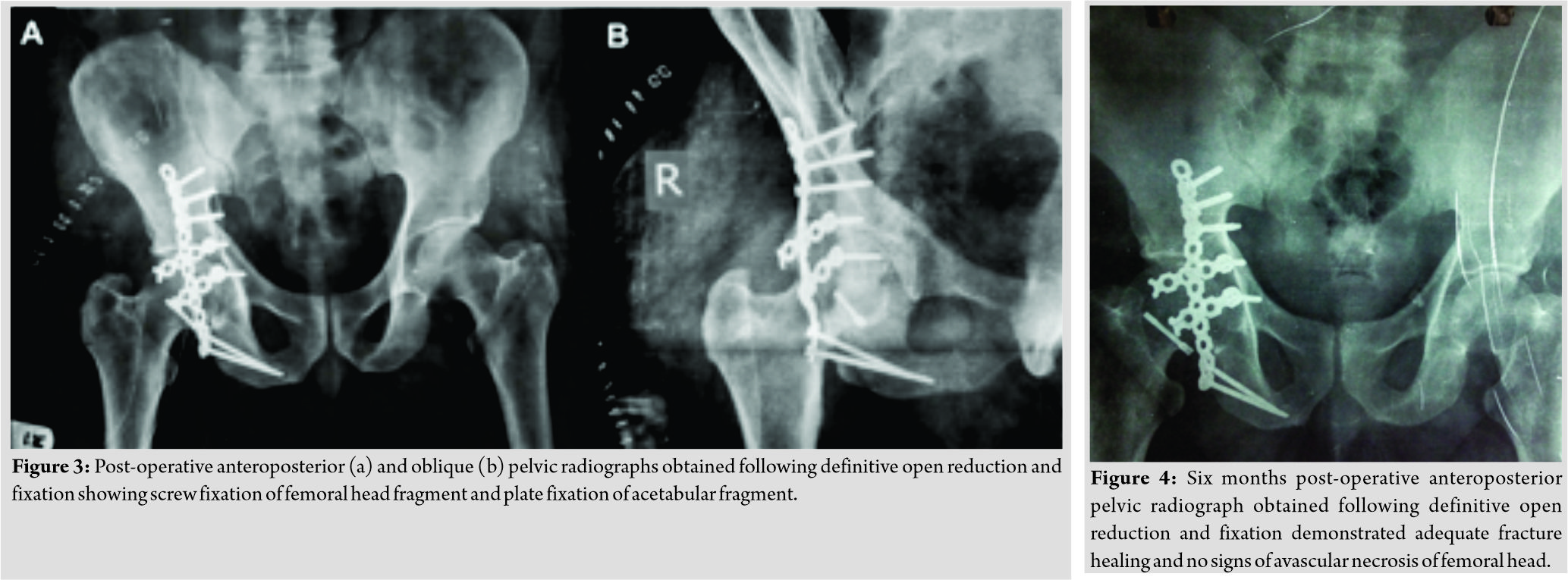 In follow-up, patient was evaluated clinically and radiologically. There were no signs of avascular necrosis and arthritis after 5 years of follow-up. Patient had rewarding outcomes in the form of adequate range of motion and painless ambulation (Fig. 5).
In follow-up, patient was evaluated clinically and radiologically. There were no signs of avascular necrosis and arthritis after 5 years of follow-up. Patient had rewarding outcomes in the form of adequate range of motion and painless ambulation (Fig. 5).
Discussion
Hip joint fractures associated with dislocation are relatively rare and often associated with a poor functional outcome [17]. Treatment strategies in femoral head fracture-dislocations are very controversial and represent one of the few true orthopedic emergencies. Reduction must be done as soon as possible. The time elapsed between dislocation and reduction of hip joint is an important element for a good outcome as it has been reported that early reduction (within 24 h) is associated with better results than late reduction [7]. Some authors have shown that the joint should be relocated within 6 h; failure to do so increases the risk of avascular necrosis of the femoral head [17]. There are several reports of good results after primary hip replacement in these injuries [8, 9] and given the age and duration of injury in the above patient one would be more inclined to replace it totally. However, patient was a farmer by occupation and required deep squatting and crossed leg sitting for earning his daily livelihood which would have been difficult after joint replacement. We also faced the same dilemma in deciding the appropriate modality and approach for this neglected injury but after discussing with the patient, it was agreed to perform ORIF for this gentleman. Anterior approach would have allowed easy reduction and fixation of the femoral head fracture, but we adopted the posterior Kocher-Langenbeck approach as this approach prevents further destruction of the soft tissue of the anterior hip; it preserves the blood supply of the anterior capsule; and it can simultaneously be used to repair the injury to the posterior capsule, which is beneficial for the recovery of the blood supply to the femoral head. In addition, good exposure of the acetabular fracture allows reduction to be accomplished under direct visualization, thereby restoring the congruency and stability of the hip. At the same time, surgery should be performed carefully to reduce the stripping and cutting of the gluteal muscles as much as possible, to protect the remaining blood supply of the hip joint and reduce the incidence of post-operative avascular necrosis of the femoral head.
Conclusion
A neglected case of Pipkin type IV injury with chances of avascular necrosis and arthritis can be given a trial of hip preservation surgery because in an Indian scenario sitting cross legged and squatting are indispensable activities of daily lifestyle and appropriate surgical technique, adequate exposure, anatomic reduction, and stable internal fixation of the fractures are critical to achieve satisfactory clinical results.
Clinical Message
A neglected Pipkin type IV femoral head fracture poses great dilemma regarding its treatment plan and approach. A trial of ORIF through posterior approach can be given in individuals near 60 years of age in Indian scenario even though the risks of AVN are far greater. Meticulous technique and anatomic reduction may give favorable results.
References
1. Brav TA. Traumatic dislocation of the hip: Army experience over a twelve-year period. J Bone Joint Surg 1962;44:1115-34.
2. Epstein HC, Wiss DA, Cozen L. Posterior fracture dislocation of the hip with fractures of the femoral head. Clin Orthop Relat Res 1985;201:9-17.
3. Brumback RJ, Kenzora JE, Levitt LE, Burgess AR, Poka A. Fractures of the femoral head. Hip 1987;181-206.
4. Sahin V, Karakas ES, Aksu S, Atlihan D, Turk CY, Halici M. Traumatic dislocation and fracture-dislocation of the hip: A long-term follow-up study. J Trauma 2003;54:520- 9.
5. Butler JE. Pipkin Type-II fractures of the femoral head. J Bone Joint Surg Am 1981;63:1292-6.
6. Epstein HC. Posterior fracture dislocations of the hip: Long-term follow-up. J Bone Joint Surg Am 1974;56:1103-27.
7. Pipkin G. Treatment of grade IV fracture dislocation of the hip. J Bone Joint Surg Am 1957;39:1027-42.
8. Guimaraes RP, de Souza GS, da Silva Reginaldo S, Ono NK, Honda EK, Polesello GC, et al. Study of the treatment of femoral head fractures. Rev Bras Ortop 2010;45:355-61.
9. Gänsslen A, Müller M, Nerlich M, Lindahl J, editors. 24 Femoral Head Fractures: Pipkin IV. Acetabular Fractures. Germany: Georg Thieme Verlag; 2018.
10. Gardner MJ, Suk M, Pearle A, Buly RL, Helfet DL, Lorich DG. Surgical dislocation of the hip for fractures of the femoral head. J Orthop Trauma 2005;19:334-42.
11. Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip-a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br 2001;83:1119-24.
12. Siebenrock KA, Gautier E, Woo A, Ganz R. Surgical dislocation of the femoral head for joint debridement and accurate reduction of fractures of the acetabulum. J Orthop Trauma 2002;16:543-52.
13. Kloen P, Siebenrock KA, Raaymakers EL, Marti RK, Ganz R. Femoral head fractures revisited. Eur J Trauma 2002;28:221-33.
14. Chen Z, Dai Z, Liao Y, Fan W, Tang Z. Treatment of type IV Pipkin fracture through transtrochanteric approach with trochanteric osteotomy. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2011;25:1184-7.
15. Guo JJ, Tang N, Yang HL, Qin L, Leung KS. Impact of surgical approach on postoperative heterotopic ossification and avascular necrosis in femoral head fractures: A systematic review. Int Orthop 2010;34:319-22.
16. Swiontkowski MF, Thorpe M, Seiler JG, Hansen ST. Operative management of dis-placed femoral head fractures: Case-matched comparison of anterior versus posterior approaches for Pipkin I and Pipkin II fractures. J Orthop Trauma 1992;6:437-42.
17. Stannard JP, Harris HW, Volgas DA, Alonso JE. Functional outcome of patients with femoral head fractures associated with hip dislocations. Clin Orthop Relat Res 2000;377:44-56.
 |
 |
 |
 |
 |
| Dr. Rakesh Goyal | Dr. Neel M Bhavsar | Dr. Akash Goel | Dr. Nishant Bhatia | Dr. Anurag Mehndiratta |
| How to Cite This Article: Goyal R, Bhavsar NM, Goel A, Bhatia N, Mehndiratta A, Goel SA. Neglected Two-Week-Old Unstable Fracture-Dislocation of the Hip in a 60 Years Old, Managed with Hip Preservation Surgery. Journal of Orthopaedic Case Reports 2020 July;10(4): 38-41. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




