[box type=”bio”] Learning Point of the Article: [/box]
High energy contact sports can induce device failure and arthroscopic techniques can assist surgeons in its management.
Case Report | Volume 10 | Issue 5 | JOCR August 2020 | Page 16-19 | Karan Singh Panesar, Angus Robertson. DOI: 10.13107/jocr.2020.v10.i05.1818
Authors: Karan Singh Panesar[1], Angus Robertson[1]
[1]Department of Orthopaedics, University Hospital of Llandough, Penlan Rd, Llandough, Penarth, CF64 2XX, Wales.
Address of Correspondence:
Dr. Karan Singh Panesar,
Foundation Year 2 Doctor, University Hospital of Llandough, Penlan Rd, Llandough, Penarth, CF64 2XX, Wales.
E-mail: karanpanesar2303@gmail.com
Abstract
Introduction: Introduction: Acromioclavicular joint (ACJ) separation is a common sports injury. Suture- button repair is favoured technique with a complication rate of 20%. We are the first to report the migration of a suture button into the glenohumeral joint.
Case Report: A 28-year-old right-handed rugby player presented with symptoms of laxity and catching within the right shoulder 4 years after reconstruction using an ACJ Dog Bone TM Technique (Arthrex Inc.). Magnetic resonance imaging showed that the coracoid suture button had migrated into the glenohumeral joint.
Conclusion: The patient was successfully treated with an arthroscopic examination of the glenohumeral joint and removal of the button. We outline the risk factors and treatment options involved in this unique presentation.
Key words: Acromioclavicular joint ACJ separation, Suture-button migration, Glenohumeral joint.
Introduction
Acromioclavicular joint (ACJ) separation is a common shoulder pathology with an estimated incidence of 1.8 per 10,000 annually [1]. It is an injury of youth with a mean presenting age of 37.5 years and around 50% of cases occurring between 20 and 39 years [1]. The most common mechanism of damage being sports- related injury, with road traffic accident being a close second. Several classifications exist for the injury, with a commonly used classification being Rockwood’s. Originally described in 1984, Rockwood outlined six different patterns of ACJ separation with the most severe demonstrating complete disruption of the acromioclavicular and costoclavicular ligaments alongside dislocation of ACJ and detachment of the deltoid and trapezius muscles [2]. Current practice is conservative management for type I and II separations, surgical intervention for Type IV to VI, and initial conservative management of type III with reconstruction reserved for those unsuccessful [3]. A variety of techniques are available for reconstruction with lag- screws, hook- plates, or suture- buttons as options [4]. In those undergoing reconstruction, there is an array of potential complications such as infection, shoulder pain, coracoclavicular calcification, fracture, and loss of reduction. Hardware migration is amongst the most commonly reported complications of suture-button reconstruction with the clavicle and coracoid being the quoted sites of migration [5]. It does not appear, however, that the literature has reported the occurrence of glenohumeral joint migration of a suture- button. This case report outlines the presentation and management of a patient with intra-joint migration.
Case Report
A fit and healthy 28-year-old right hand dominant patient presented with bilateral symptoms of shoulder instability after multiple impacts while playing rugby. The right shoulder clinically demonstrated greater anteroposterior laxity than the left and was more symptomatic. Symptoms included intermittent mechanical symptoms of “’catching”’ within the shoulder. There was also evidence of scarring consistent with a previous ACJ reconstruction. Clinically, there had been partial failure of the reconstruction with subluxation at the ACJ. There was no other relevant history of note. On reviewing the patients records, it appeared that the patient had a prior history of ACJ separation, a result of a rugby injury 4 years previously. He had suffered a high Grade III ACJ separation of the right shoulder. This was reconstructed within 2 weeks of the injury using a standard arthroscopic technique using two dog bone buttons and two FiberTape sutures. The patient had an uncomplicated recovery and a post-operative X-ray demonstrated a good reduction and button positions. (Fig. 2). Three years after this initial presentation, the patient had sustained a further rugby injury to the right shoulder. Examination revealed partial failure of the reconstruction. X-rays demonstrated minimal ACJ displacement and button displacement and it was, therefore, decided to manage the patient conservatively (Fig. 3). The patient returned to unrestricted sport.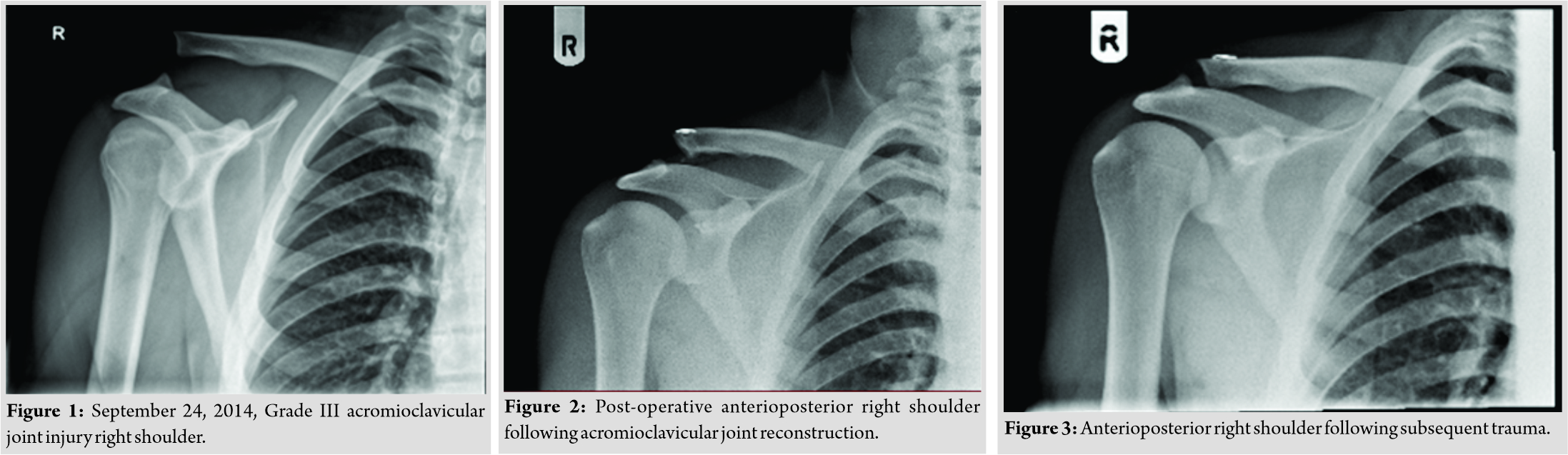
In order to investigate the patient’s instability, a magnetic resonance arthrogram (MRA) of the right shoulder was requested. The arthrography X-rays confirmed that the coracoid suture button had migrated into the glenohumeral joint. (Fig. 4) The subsequent MRA confirmed this and demonstrated a Hills-–Sachs lesion and posterior labral injury (Fig. 5). A labral repair was performed alongside arthroscopic removal of the loose dog bone button. Four months after stabilisation, the patient is recovering well with no further ACJ or instability symptoms.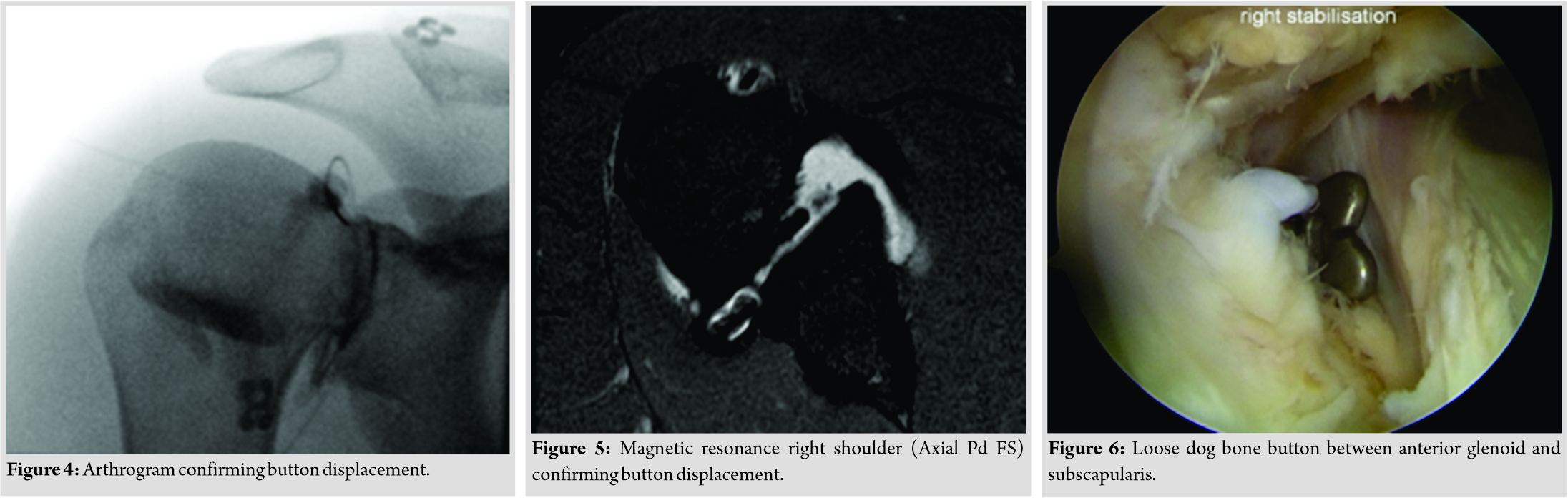
Discussion
Suture- button fixation of the ACJ has been shown to offer better quality of life post-surgery when compared to alternative methods. A meta-analysis between hook plate fixation and suture- button repair demonstrated similar complication rates, but reduced pain scores and better functional outcomes with suture buttons [6]. This is replicated in sport, with athletes having superior sport- specific outcomes when treated via through suture- button repair [7]. The complication rate after suture- button repair of the ACJ is around 20% [8]. Loss of reduction and migration are frequently reported, with the majority of patients showing at least some migration of the implant into the superior cortex of the clavicle by two 2 years [9]. Around one- quarter of patients will experience some loss of reduction radiographically, however, this is usually asymptomatic, with patients still reporting high satisfaction rates and excellent functional outcomes [10]. Return to activity is relatively short with the average time lost for high- grade ACJ separation being 2.5 months [11]. The majority of patients will have a sport- specific ACJ integrity that was at least as good as prior to before the trauma [12]. In regard to our patient, he appeared to suffer reinjury twice after the initial tear, both times occurring years after the previous episode. Sport is the most common cause of ACJ separation in the young [1]. Rugby has been shown to have a high preponderance for ACJ injury [11]. For professional rugby players, it is the most common injury, causes most absence, and has the highest rate of recurrence [13]. In this case, the patient’s successful return to contact sports resulted in subsequent reinjury of the shoulder girdle and eventual hardware failure. The energy involved in impacts may be responsible for the nature of migration of the suture button. The patient’s glenohumeral symptoms led us to request the MRA. Nearly 40% of patients suffering from ACJ separations will have a concurrent glenohumeral injury [14], as did our patient with his Hill-–Sach’s lesion. The proportion of associated glenohumeral injury increases with age, rising as high as 57.3% in those over 35. This favours arthroscopic over open surgery as it allows identification and correction of any possible glenohumeral defects, a sentiment shared by other authors [14].
Conclusion
We present a case of a patient presenting 4 years after an ACJ reconstruction using a suture- button with migration of the suture- button into the glenohumeral joint space and an associated Hill-–Sach’s lesion. The involvement of the patient in contact sports with repeated, high- energy impacts through the ACJ is the culprit for such a presentation, and patients should be aware of the risk of recurrence and complication associated with continued participation.
Clinical Message
High- energy contact sports can induce device failure. It is important for physicians treating these types of injuries and to be aware of this possibility. Arthroscopic techniques can assist surgeons in managing device failure as well as dealing with additional pathology.
References
1. Chillemi C, Franceschini V, Dei Giudici L, Alibardi A, Santone FS, Alday LJ, et al. Epidemiology of isolated acromioclavicular joint dislocation. Emerg Med Int 2013;2013:1-5.
2. Gorbaty JD, Hsu JE, Gee AO. Classifications in brief: Rockwood classification of acromioclavicular joint separations. Clin Orthop Relat Res 2017;475:283-7.
3. Beitzel K, Cote MP, Apostolakos J, Solovyova O, Judson CH, Ziegler CG, et al. Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy 2013;29:387-97.
4. Lee S, Bedi A. Shoulder acromioclavicular joint reconstruction options and outcomes. Curr Rev Musculoskelet Med 2016;9:368-77.
5. Nelson A, Woodmass J, Esposito J, Ono Y, Lo I, Boorman R, et al. Complications following arthroscopic fixation of acromioclavicular separations: A systematic review of the literature. Open Access J Sports Med 2015;6:97-107.
6. Wang C, Meng JH, Zhang YW, Shi MM. Suture button versus hook plate for acute unstable acromioclavicular joint dislocation: A meta-analysis. Am J Sports Med 2020;48:1023-30.
7. Müller D, Reinig Y, Hoffmann R, Blank M, Welsch F, Schweigkofler U, et al. Return to sport after acute acromioclavicular stabilization: A randomized control of double-suture-button system versus clavicular hook plate compared to uninjured shoulder sport athletes. Knee Surg Sports Traumatol Arthrosc 2018;26:3832-47.
8. Clavert P, Meyer A, Boyer P, Gastaud O, Barth J, Duparc F. Complication rates and types of failure after arthroscopic acute acromioclavicular dislocation fixation. Prospective multicenter study of 116 cases. Orthop Traumatol Surg Res 2015;101:S313-6.
9. Scheibel M, Dröschel S, Gerhardt C, Kraus N. Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med 2011;39:1507-16.
10. Murena L, Vulcano E, Ratti C, Cecconello L, Rolla PR, Surace MF. Arthroscopic treatment of acute acromioclavicular joint dislocation with double flip button. Knee Surg Sports Traumatol Arthrosc 2009;17:1511-5.
11. Pallis M, Cameron KL, Svoboda SJ, Owens BD. Epidemiology of acromioclavicular joint injury in young athletes. Am J Sports Med 2012;40:2072-7.
12. Saier T, Plath JE, Beitzel K, Minzlaff P, Feucht JM, Reuter S, et al. Return-to-activity after anatomical reconstruction of acute high-grade acromioclavicular separation. BMC Musculoskelet Disord 2016;17:145.
13. Headey J, Brooks JH, Kemp SP. The epidemiology of shoulder injuries in English professional rugby union. Am J Sports Med 2007;35:1537-43.
14. Markel J, Schwarting T, Malcherczyk D, Peterlein CD, Ruchholtz S, El-Zayat BF. Concomitant glenohumeral pathologies in high-grade acromioclavicular separation (type III-V). BMC Musculoskelet Disord 2017;18:439.
 |
 |
| Dr. Karan Singh Panesar | Dr. Angus Robertson |
| How to Cite This Article: Panesar KS, Robertson A. Glenohumeral Migration of Intraosseous Suture Button after Acromioclavicular Joint Reconstruction – A Case Report. Journal of Orthopaedic Case Reports 2020 August;10(5): 16-19. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




