[box type=”bio”] Learning Point of the Article: [/box]
Review of literature suggests a knee dislocation warranting diagnosis of “irreducible” stems from the combination of lack of completed closed reductions, despite several attempts, due to entrapped structures within the capsule and characteristic gross examination findings. Our patient presented with a “dimple sign,” perceived as pathognomonic by many, as well as an X-ray demonstrating lateral subluxation with wide medial compartment. We then performed a technique previously described by Tetada et al. resulting in successful closed reduction with resolution of the “dimple sign.”
Case Report | Volume 10 | Issue 7 | JOCR October 2020 | Page 6-10 | Thomas Schmicker, Timothy Kocher, Tyag Patel, Dana Lycans. DOI: 10.13107/jocr.2020.v10.i07.1894
Authors: Thomas Schmicker[1], Timothy Kocher[2], Tyag Patel[1], Dana Lycans[3]
[1]Department of Orthopaedic Surgery, Marshall University, 1600 Medical Center Dr., Huntington, WV 25701, United States,
[2]Department of Orthopaedics, Joan C, Edwards School of Medicine, Marshall University, 1600 Medical Center Dr., Huntington, WV 25701, United States,
[3]Department of Orthopedic Sports Medicine, Marshall University, 1600 Medical Center Dr., Huntington, WV 25701, United States.
Address of Correspondence:
Dr. Thomas Schmicker,
PGY-4, MD, Department of Orthopaedic Surgery, Marshall University, 1600 Medical Center Dr., Huntington, WV 25701, United States.
E-mail: schmicker@marshall.edu
Abstract
Addition to Orthopedic Literature: Posterolateral knee dislocations are extremely rare and generally require open reduction; however, we were able to provide closed reduction by reproducing mechanism of injury with a technique described in the literature. This is the second reported case of such accomplishment.
Introduction: Posterolateral knee dislocation is the most common form of “irreducible” knee dislocations. Buttonholing of the medial femoral condyle through medial soft tissues of the knee results in entrapment. We report the second known case of successful closed reduction.
Case Presentation: A 51-year-old female with morbid obesity sustained a right posterolateral knee dislocation shown on plain radiograph. This was accompanied by lateral patella dislocation and a dimple sign at the medial joint line after a fall from standing height produced a rotational mechanism.
Conclusion: This is the second reported case of successful closed reduction to an injury that has been generally established to be “irreducible.” The technique used closely matches that described in the only other reported case and involves reproduction of the mechanism of injury. This establishes additional evidence to a previously isolated report of successful acute treatment that counters the current narrative.
Keywords: Posterolateral dislocation, dimple sign, buttonhole, irreducible dislocation.
Introduction
Traumatic knee dislocations are uncommon injuries, and rarely, they may be irreducible with closed methods. These injuries can occur from an ultra-low to the high-energy mechanism. Acute management includes emergent neurovascular evaluation followed by prompt closed reduction under conscious sedation, as there is a possibility for limb loss and sequelae of limb ischemia. Irreducible knee dislocations are often the result of a rotational mechanism and are usually posterolateral. In these cases, the medial femoral condyle (MFC) passes through or “buttonholes” the medial soft tissues of the knee. The subsequent interposition of the medial retinaculum, MCL, vastus medialis, and/or medial meniscus can create a characteristic “dimple sign” with a prominence of the MFC on physical examination. As the dimple sign has been described as a contraindication to closed reduction, few instances of closed reduction maneuvers for these posterolateral dislocations have been described. We report the clinical case of a 51-year-old morbidly obese woman who sustained a right posterolateral knee dislocation with a concomitant lateral patella dislocation and fibula head fracture after a fall from standing height. The dimple sign was present and closed reduction under conscious sedation in the emergency department failed. She subsequently underwent a successful closed reduction in the operating room under general anesthesia by flexing the knee to 120 combined with internal rotation of the lower extremity and application of valgus stress at the distal thigh as described by Tateda et al. She was placed in knee-spanning external fixation. Post-reduction MRI showed ACL, PCL, MCL, and partial LCL rupture with disruption of the medial patellar retinaculum. Clinical course is outlined below.
Background
Dislocations of the knee comprise <0.2% of orthopedic injuries, though they are likely under reported due to spontaneous reduction and misdiagnosis [1, 2, 3]. Irreducible dislocations are a rare subset comprising 4% of these injuries and are almost always posterolateral or lateral dislocations with medial tissue entrapment requiring open reduction [4]. Emergent and continuous neurovascular evaluation of these patients are paramount as the incidence of the popliteal artery and peroneal nerve injury is 16% and 20–40%, respectively [4, 5]. The medial retinaculum and MCL are the most commonly entrapped structures blocking reduction [4]. Subsequent traction of soft-tissue surrounding the subcutaneous medial femoral condyle often causes puckering of the skin known as the dimple sign and can lead to skin necrosis if the reduction of the joint is not promptly achieved [6].
Case Presentation
A 51-year-old morbidly obese female presented to the emergency department of our facility after sustaining a fall from standing height while at home. She described a rotatory mechanism and an inability to bear weight on her right lower limb due to pain and instability at the knee. On examination, the invagination of the skin was noted at the medial joint line of the knee in a characteristic dimple sign. Posterior tibial and dorsalis pedis pulses were palpable bilaterally at 2+ and 1+, respectively, with no signs of hypoperfusion to the right foot. All compartments were soft, and no pain with passive range of motion was noted at the ankle and foot. Sensory and motor innervation was intact. Ankle-brachial indices (ABIs) of bilateral lower extremities were documented at 1.10. Neurovascular status was closely monitored throughout the patient’s stay. Further, vascular studies, such as angiography, were deferred. Radiographs revealed lateral subluxation of the tibiofemoral joint with a wide medial compartment and lateral dislocation of the patella (Fig. 1a, 1 b, 1c).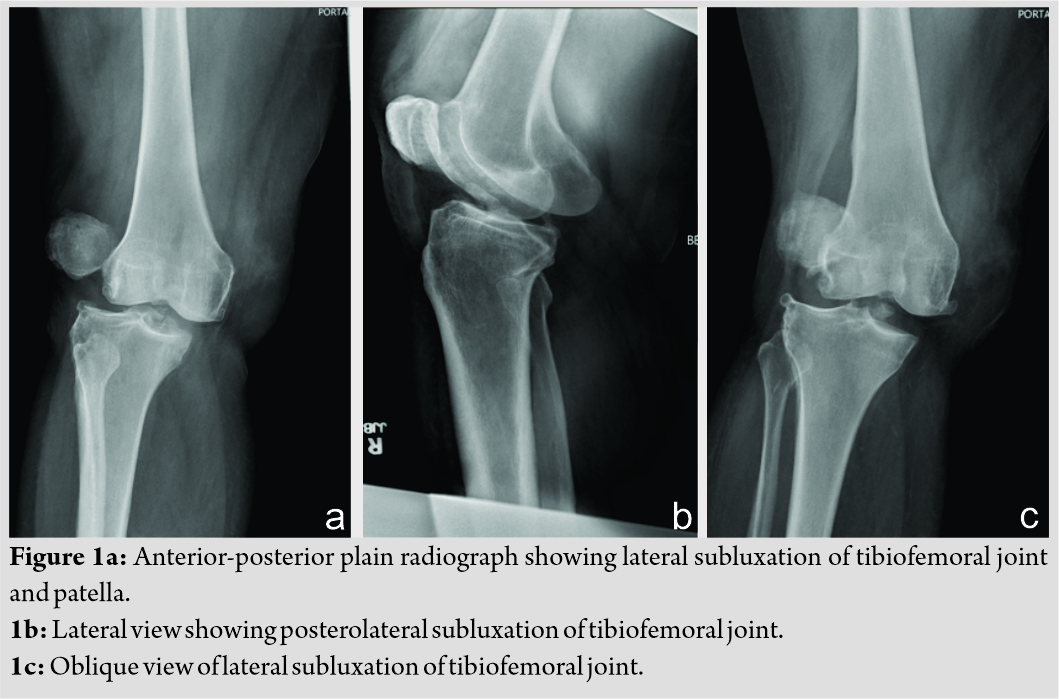
The emergency room physician urgently sedated the patient and the orthopedic trauma team, which was inclusive of a junior and senior resident as well as the attending surgeon, performed several attempts at reduction. The reduction technique employed consisted of traction and counter-traction with a force directed to correct the deformity. A lateral-to-medial force failed to reduce the patella. After unsuccessful closed reduction, the patient was transported to the OR for closed versus open reduction under general anesthesia. She was placed supine on the table with a bump under the right hip and with her right leg slightly flexed on a foam pad. The leg was prepped in the usual sterile fashion and before the incision was made, the hip was flexed, and the knee was flexed to 120 with internal rotation of the limb. A large valgus force was applied at the distal thigh, as described by Tateda et al. [7]. The dislocation was reduced, and the dimple sign disappeared. The limb was brought out to extension and reduction was confirmed with fluoroscopy in the anterior-posterior and lateral views. Some lateral subluxation of the patella remained (Fig. 2a, 2b). It was felt that this maneuver allowed the medial femoral condyle to be pulled back through the buttonhole in the medial retinaculum.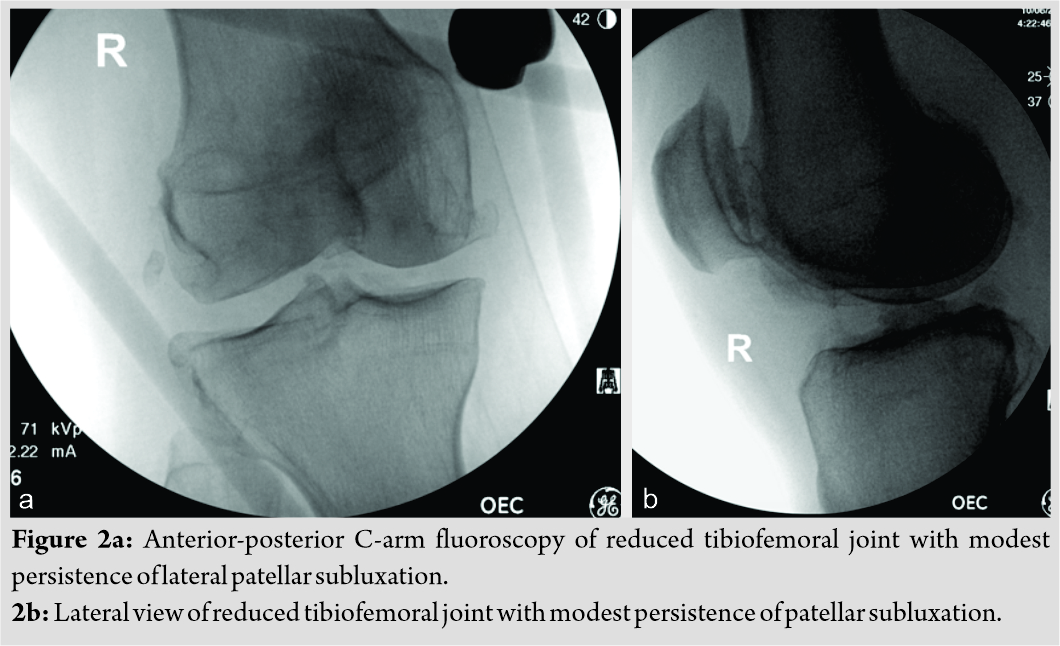
The right lower extremity was subsequently placed in knee spanning external fixation due to gross instability. Post-operative pulses remained at baseline 2+ DP and 1+ PT bilaterally, and the patient was admitted for regular neurovascular checks. Repeat ABIs were 0.99 right leg and 1.10 left leg. MRI of the right knee showed a fracture of the fibula with ruptures of the ACL, PCL, MCL, and partial LCL, therefore classifying this as a KD-V injury by the Schenck classification [4] (Fig. 3a, 3b, 3c, 3d). A medial meniscal root tear was also present. It was planned that the patient would remain non-weight-bearing and in external fixation for 6 weeks to undergo staged ligament reconstruction.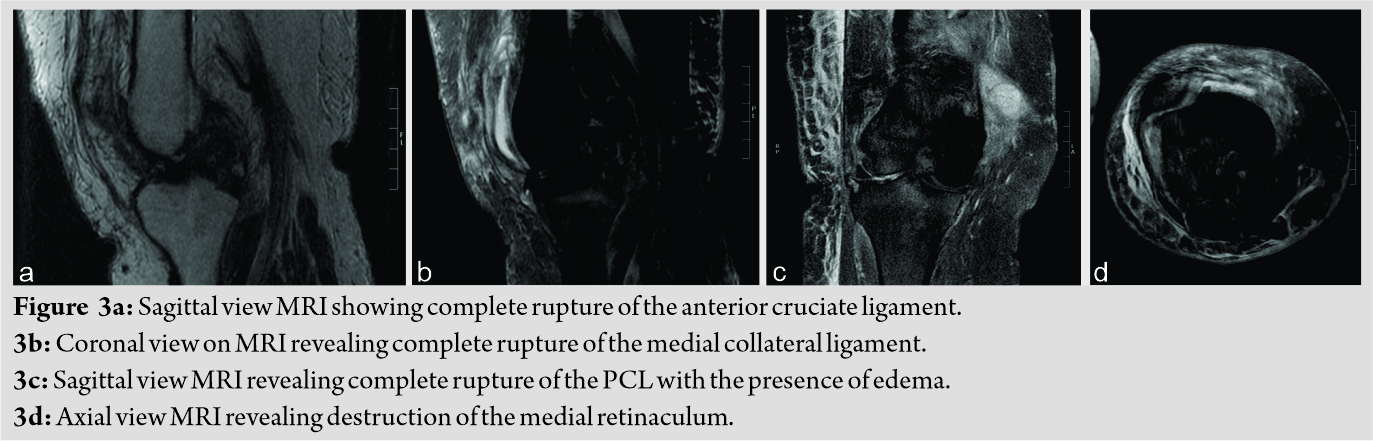
Discussion
A descriptive classification of knee dislocation was created by Kennedy in 1963 with five categories based on tibial translation with regard to the femur; anterior, posterior, medial, lateral, and rotatory [8]. Knee dislocations may be reduced before evaluation, and the more recent and commonly used Wascher-modified Schenck classification categorizes dislocation based on the pattern of ligamentous injury [9, 10]. In addition, dislocations can occur from ultra-low velocity to high-velocity mechanisms [1, 11] Historically, knee dislocations have been considered high-energy injuries sustained commonly during motor vehicle collisions; however, lower-energy injuries such as sports-injuries have become more common. This may be due to today’s larger, faster athletes participating in higher-contact and extreme sports [3]. Those patients in the ultra-low-velocity cohort, such as our patient, are likely to be female, morbidly obese, with an average BMI of 49, and to have KD-IV injuries with a higher prevalence of neurovascular injury [1, 11]. The majority of dislocations reduce easily with a spontaneous reduction rate of 50%; therefore, a high degree of suspicion is necessary from the treating clinician [8]. The primary concern is for neurovascular injury and compartment syndrome, and urgent neurovascular evaluation is required. The popliteal artery is injured in 10–40% of instances, most commonly in anterior and posterior dislocations [3]. With anterior dislocations, a traction mechanism causes intimal damage to the popliteal artery, while a posterior dislocation can transect the popliteal artery from the tibia as the artery is tethered proximally at the adductor hiatus and distally at the soleus arch [1, 3]. Peroneal nerve injury is common at 20–45%, though a wide variation in incidence is reported, with only 50% achieving a return of function [1, 3, 8]. The peroneal nerve is constrained at the fibular neck proximally and at the intermuscular septum distally similarly to the popliteal artery; however, displacement in the coronal plane is more likely to result in injury of this structure [3]. Irreducible dislocations are commonly lateral or posterolateral and have a lower rate of vascular injury but will more commonly have peroneal nerve injury [12]. Although some studies have shown that normal distal pulses may exclude vascular injury with 100% sensitivity, ABIs are the appropriate initial vascular study with a value below 0.9, having a 100% sensitivity and specificity for arterial injury [3]. While in the past, some authors have advocated for angiography in all dislocations, the current consensus is that further evaluation with angiography is appropriate with abnormal ABIs and can be foregone with normal values [13]. Dislocations eventually designated as “irreducible” are most often those that involve posterolateral translation [12]. The two most common structures that became entrapped are the MCL and medial retinaculum, but other structures that can block reduction include the vastus medialis, medial meniscus, capsule, and adductor magnus [1, 4]. The patella and posterolateral capsuloligamentous structures may obstruct reduction as well [4]. Both cruciate ligaments are usually torn. In lateral dislocations, the hamstring tendons may enter the notch and impede reduction, but knee flexion reliably reduces this injury [4]. In posterolateral dislocations, a valgus and external or internal rotation of the tibia mechanism has been described to tension the subsequently injured medial structures but leave the lateral structures slack and often uninjured [6]. The presence of a dimple sign has been stated to be pathognomonic of irreducible dislocations and present in 85% of these injuries [4]. It has been described as a contraindication to closed reduction with case reports suggesting worsened skin puckering and subsequent skin sloughing with repeated attempts [12]. Other case reports have illustrated unsuccessful attempts at closed reduction of irreducible posterolateral dislocations with maximal knee flexion, gentle manual manipulation with traction counter-traction, posterior force on the tibia with internal rotation of the tibia, and arthroscopic attempts at a reduction that have also been generally unsuccessful [6, 12]. Open reduction with or without acute repair or reconstruction of ligaments is traditionally indicated, and the prognosis is generally good [13]. In this case, we used a technique first described by Tateda et al. to successfully close reduce an otherwise irreducible posterolateral knee dislocation [7]. There are few reported instances of closed reduction maneuvers for posterolateral knee dislocations, in which the medial femoral condyle has buttonholed through medial soft-tissue structures. Dr. Tateda describes flexing the knee to 120 degrees, along with an internal rotation of the lower extremity and valgus force at the distal thigh. He explains that this maneuver essentially recreates the mechanism of injury while allowing the medial femoral condyle to reduce through the medial retinaculum. The authors also demonstrated that the dislocation could be reproduced with external rotation of the tibia and postulates this to be the mechanism of dislocation in his patient. In our case and in that reported by Tateda et al., an MRI was not obtained before reduction, so it is uncertain, in which medial tissues were interposed. Therefore, it is possible that irreducible dislocations with interposed tissues different from this patient’s may not be reducible with this maneuver. After reduction, the timing of ligamentous reconstruction remains controversial [14]. Indications for external fixation in the setting of an acute knee dislocation are the inability to maintain reduction, history of vascular injury, and open dislocation. There are very little data comparing spanning external fixation versus bracing before multiligament knee reconstruction [13]. A Mayo Clinic study compared eight knees placed in external fixation after reduction with 23 knees braced after reduction and found no statistically significant difference in patient Lysholm scores and mean IKDC scores at 27 months of follow-up [15]. Interestingly, patients placed in a brace had a better range of motion at long-term follow-up compared to external fixation; however, this could be attributed to more complex injuries requiring external fixation.
Conclusion
Irreducible knee dislocations are uncommon and have been described as needing obligate open reduction. A recent literature review of irreducible knee dislocations and management acknowledges the only other reported case of closed reduction done by Dr. Tateda but omit it from management considerations due to lapse in terminology [14]. However, the literature suggests a knee dislocation warranting title of “irreducible” stems from a combination of lack of completed closed reduction, despite several attempts, due to entrapped structures within the capsule and characteristic gross examination findings. Evidence of widened joint space shown on radiograph along with the presence of the dimple sign, which resolved post-reduction and reported mechanism of injury with clinical presentation, matches our patient to the described literature. This case report is the second reported instance of what has been broadly considered an “irreducible” dislocation being acutely treated with closed reduction techniques. Concomitant neurovascular injury is frequent, necessitating prompt evaluation and treatment. In this case, knee flexion combined with internal rotation of the limb and application of a valgus force at the knee withdrew the medial femoral condyle from the buttonhole in the medial soft-tissue structures successfully reducing the tibiofemoral joint. Added evidence of successful outcomes paves the way for further research and assessment of this technique.
Clinical Message
Irreducible knee dislocations are almost always posterolateral or lateral dislocations with medial tissue entrapment requiring open reduction. However, we closely reproduced a technique that successfully accomplished closed reduction by recreating the rotary mechanism. This may open the path to a refined acute first-line treatment that releases joint tension and allows reassessment for further management without the risks of surgery.
References
1. Boyce RH, Singh K, Obremskey WT. Acute management of traumatic knee dislocations for the generalist. J Am Acad Orthop Surg 2015;23:761-8.
2. Rihn JA, Groff YJ, Harner CD, Cha PS. The acutely dislocated knee: Evaluation and management. J Am Acad Orthop Surg 2004;12:334-46.
3. Peskun CJ, Levy BA, Fanelli GC, Stannard JP, Stuart MJ, MacDonald PB, et al. Diagnosis and management of knee dislocations. Phys Sportsmed 2010;38:101-11.
4. Xu B, Xu H, Tu J, Guo R. Initial assessment and implications for surgery: The missed diagnosis of irreducible knee dislocation. J Knee Surg 2018;31:254-63.
5. Halvorson JJ, Anz A, Langfitt M, Deonanan JK, Scott A, Teasdall RD, et al. Vascular injury associated with extremity trauma: Initial diagnosis and management. J Am Acad Orthop Surg 2011;19:495-504.
6. Huang FS, Simonian PT, Chansky HA. Irreducible posterolateral dislocation of the knee. Arthroscopy 2000;16:323-7.
7. Tateda S, Takahashi A, Aizawa T, Umehara J. Closed reduction of “Irreducible” posterolateral knee dislocation-a case report. J Orthop Case Rep 2016;6:20-3.
8. Kennedy JC. Complete dislocation of the knee joint. J Bone Joint Surg 1963;45:889-904.
9. Schenck R. Classification of knee dislocations. Oper Tech Sports Med 2003;11:193-8.
10. Wascher DC, Dvirnak PC, DeCoster TA. Knee dislocation: Initial assessment and implications for treatment. J Orthop Trauma 1997;11:525-9.
11. Werner BC, Gwathmey FW Jr., Higgins ST, Hart JM, Miller MD. Ultra-low velocity knee dislocations: Patient characteristics, complications, and outcomes. Am J Sports Med 2014;42:358-63.
12. Capito N, Gregory MH, Volgas D, Sherman SL. Evaluation and management of an irreducible posterolateral knee dislocation. J Knee Surg 2013;26:S136-41.
13. Levy BA, Fanelli GC, Whelan DB, Stannard JP, MacDonald PA, Boyd JL, et al. Controversies in the treatment of knee dislocations and multiligament reconstruction. J Am Acad Orthop Surg 2009;17:197-206.
14. Khanna G, Herrera DA, Wolters BW, Dajani KA, Levy BA. Staged Protocol for High Energy Knee Dislocation: Initial Spanning External Fixation Versus Hinged Knee Brace. Washington, DC: Presented as an E-Poster at the 27th Annual Meeting of the Arthroscopy Association of North America; 2008.
15. Malik SS, MacDonald PB. The irreducible knee dislocation. J Knee Surg 2020;33:328-34.
 |
 |
 |
 |
| Dr. Thomas Schmicker | Mr. Timothy Kocher | Dr. Tyag Patel | Dr. Dana Lycans |
| How to Cite This Article: Schmicker T, Kocher T, Patel T, Lycans D. Closed Reduction of an Irreducible Knee Dislocation: A Case Report. Journal of Orthopaedic Case Reports 2020 October;10(7): 6-10. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




