 [box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
Necrotizing fasciitis can initially present as a benign injury with abnormal laboratory values that mandates close clinical observation.
Case Report | Volume 10 | Issue 9 | JOCR December 2020 | Page 52-55 | Zachary P Herzwurm, Cameron S Murphy, B Gage Griswold, Colton R J Webber, Kyle M Mahoney. DOI: 10.13107/jocr.2020.v10.i09.1900
Authors: Zachary P Herzwurm[1], Cameron S Murphy[1], B Gage Griswold[1], Colton R J Webber[1], Kyle M Mahoney[1]
[1]Department of Orthopaedic Surgery, Augusta University Medical Office Building, Augusta, Georgia.
Address of Correspondence:
Dr. Zachary P Herzwurm,
Department of Orthopaedic Surgery, Augusta University Medical Office Building, Second Floor, 1447 Harper St, Augusta, Georgia 30912.
E-mail: zherzwurm@gmail.com
Abstract
Introduction: Necrotizing fasciitis, also referred to necrotizing soft-tissue infection (NSTI), is an infrequent entity that results in orthopedic consultation. It is a rapidly spreading typically associated with a contaminated wound that spreads rapidly along fascial planes resulting in significant morbidity and mortality. However, it is a rare occurrence that such pathology occurs in an atraumatic fashion, which is without a wound through the skin.
Case Report: A 33-year-old female with no significant medical history presented to a walk-in orthopedic clinic with increasing ankle pain after a lateral ankle sprain 2 days prior. Patient denies any fevers, chills, shortness of breath, numbness, tingling, paresthesia, or any additional trauma since the initial ankle sprain. The patient was afebrile, maintaining oxygenation, normotensive, but tachycardic to just over 100. Physical examination was only significant for moderate swelling and ecchymosis about the lateral malleolus. X-rays and venous ultrasound were negative for any associated pathology. After a period of observation, the patient acutely decompensated with a significant increase in pain in the lower leg on passive stretch, an increase in compartment firmness and a worsening tachycardia up to the 120’s. The patient was taken emergently for fasciotomies for presumed compartment syndrome. The patient was hemodynamically unstable during the case and transferred to the intensive care unit where she continued to decompensate, requiring multiple vasopressors. The affected extremity became necrotic at the level of the foot and her hemodynamic instability continued, causing a return to the operating room for an emergent guillotine above-knee amputation. The patient progressively stabilized and underwent a formal above-knee amputation 2 days later. Cultures obtained during the second case were positive for Group A Streptococcus.
Conclusion: This case highlights the variable presentation of NSTIs as well as has having a high index of suspicion to ensure this highly morbid and fatal disease process is diagnosed expeditiously. This case is also unique in that it developed without any obvious wounds and that monomicrobial Group A Streptococcus was the culprit, while most NSTIs are polymicrobial.
Keywords: Necrotizing fasciitis, non-penetrating, amputation.
Introduction
Necrotizing soft-tissue infections represent a spectrum of infection that can be distributed throughout the different layers of soft tissues. This includes cellulitis, myositis, and fasciitis. Necrotizing fasciitis is the most severe and life threatening. Commonly, it is caused by a local skin infection, trauma, or a contaminated wound. The progression is patient dependent, but the most common initial symptom is local pain, followed by fever, and can then progress to fulminant sepsis [1, 2]. Further, these infections are likely more aggressive in patients with serious medical comorbidities such as diabetes, obesity, kidney disease, vascular disease, drug/alcohol abuse, or advancing age sepsis [3, 4]. Mortality rate is variable but approaches 100% without any treatment which is why prompt diagnosis is vital [5]. These infections can be grouped into polymicrobial and monomicrobial with polymicrobial representing 75% sepsis. Monomicrobial infections are primary caused by Group A Streptococcus, MRSA, or clostridium species. Both of which likely are likely caused by injury or hematogenous spread from pharyngeal colonization or infection 3. Polymicrobial infections almost always involved a relative immunocompromised host due to medical comorbidities. Monomicrobial infections, however, may not have any risk factors [6]. The authors would like to present an unusual and rare case presentation of necrotizing fasciitis in a young healthy patient that developed after an ankle sprain. This highlights the importance of having a high index of suspicion for a diagnosis of necrotizing fasciitis, regardless of the initial presentation.
Case Presentation
The patient originally presented as a 33 year-old Caucasian female with no significant medical history with the exception of generalized anxiety disorder who presented in an afterhours orthopedic clinic with a chief complaint of the right ankle pain and edema after a fall at a wedding 2 days prior. Over a 48 h course, her edema had increased and migrated proximally to involve her right leg. Elevation, range of motion of her ankle, and weight-bearing exacerbated her pain. The patient did complain of paresthesia throughout her entire foot. The patient denied any associated fever, chills, shortness of breath, or systemic symptoms. Initial X-rays are obtained in (Fig. 1a, 1b). No evidence of acute osseous pathology or soft-tissue gas was noticed. Patient’s original physical examination was as follows – significant edema and erythema of the right foot and leg, tenderness to palpation along the entirety of the right lower extremity distal to the knee, large amount of ecchymosis over the lateral malleolus, compartments firm but compressible, mild pain with passive stretch, triphasic dorsalis pedis and posterior tibial artery pulses, sensation intact but diminished as compared to the left lower extremity in a global nerve distribution distal to her ankle joint, motor function intact for gastroc-soleus complex, extensors, and flexors. The patient was referred to the emergency department where subsequent venous duplex ultrasound showed no evidence of deep venous thrombosis. Initial vital signs and laboratory work are shown in (Table 1, 2). The patient was admitted to the emergency room observation unit where serial compartments checks were performed. The patient initially had improvement in the emergency room; however, 12 h after admission, the patient became hypotensive and tachycardic necessitating an emergent trip to the operating room for compartment releases. A dual incision fasciotomy was carried out on the right lower extremity as well as two incisions on the dorsum of the right foot. During the fasciotomy, dishwater fluid was encountered as well as weakened fascia. A 1 1 cm tissue biopsy from the leg and the dorsal foot was sent to pathology. The fasciotomy sites were copiously irrigated and a wound VAC was placed at the fasciotomy sites of the leg. The patient was immediately transferred to the surgical intensive care unit (SICU) requiring norepinephrine pressors. After transfer to the SICU, the patient’s blood cultures were reported positive for Gram-positive cocci and broad-spectrum antibiotics of vancomycin, clindamycin, and penicillin were started by guidance of infectious disease. In the SICU, the patient continued to deteriorate, becoming further hemodynamically unstable and requiring addition of vasopressin. Reevaluation 5 h post-operative revealed a necrotic right foot, as shown in (Fig. 2). In addition, our biopsy results revealed “Acute inflammation and necrosis of deep subcutaneous tissue and focal skeletal muscle necrosis, consistent with necrotizing fasciitis.” Due to the patient’s clinical status, biopsy results, and right foot, the patient was again taken to the operative room as an emergent case. The right dorsal foot revealed complete necrosis of the fascia, subcutaneous fat, and muscle leading to a through tibia guillotine amputation. However, the patient’s muscle, fat, and fascia appeared necrotic at this amputation level. A 5 cm incision was then made over the medial thigh, which also revealed an ascending infection, necrotic muscle, fat, and fascia. A guillotine amputation was performed through the mid-thigh. Postoperatively, the patient stabilized and was managed on ceftriaxone 2 weeks postoperatively. The patient returned to the operative room for a repeat irrigation and debridement 1 day post-operative of the guillotine above-knee amputation and had a finalized above-knee amputation 3 days post-operative of initial presentation. Eight months postoperatively, the patient is doing well, ambulating with a prosthesis. Her final X-ray is shown in (Fig. 3).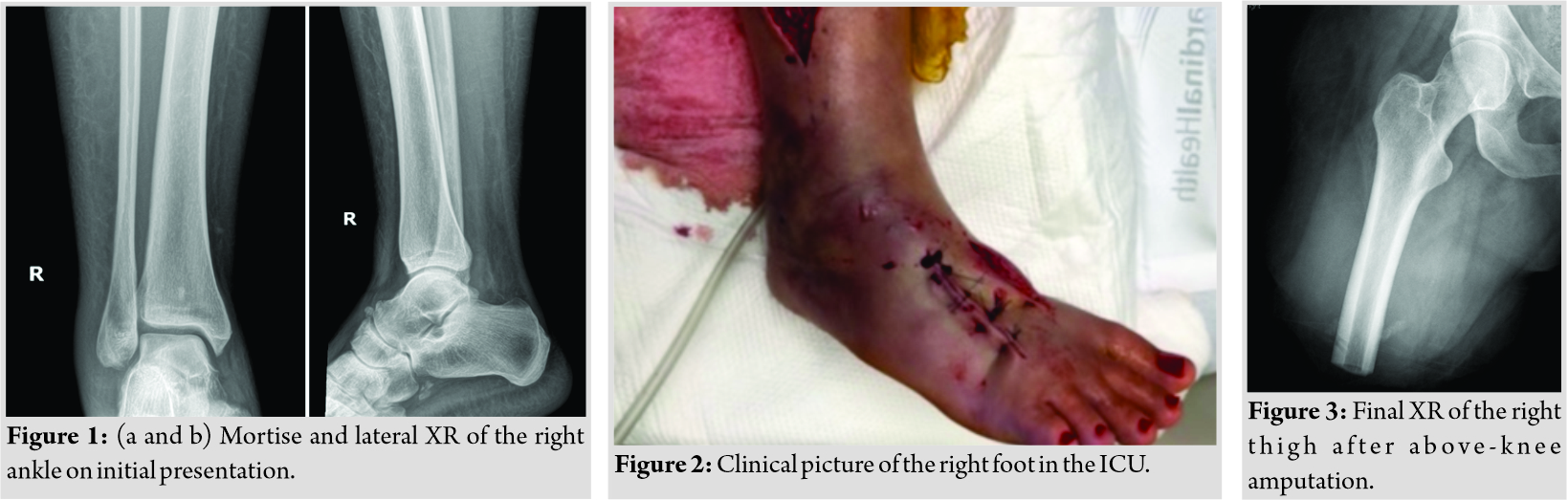
Discussion
Necrotizing soft-tissue infections include necrotizing fasciitis, necrotizing cellulitis, Fournier’s gangrene, and necrotizing myositis and are primarily caused by Clostridium species and Group A Streptococcus species [1, 3, 7]. Lower limb infections are often preceded trauma that can be as minor as skin abrasions or diabetic foot ulcers [8]. However, in our literature review, we were unable to identify a case of an immunocompetent host who developed necrotizing fasciitis without a penetrating injury or inciting infection. Unique cases have been reported that include necrotizing fasciitis in an atraumatic immunocompromised host, another case from an intestinal perforation of a toothpick, and a another case from a simple cat bite [5, 9, 10]. Studies have shown the inaccuracy of relying solely on laboratory values [11, 12], which encourages physicians to utilize physical examinations and investigate suspected deadly infections. While this case proves extremely rare, our suspicion led us to perform a tissue biopsy for an emergent pathology analysis. This decision proved vital in preserving the life of our patient as the diagnosis directed our management to amputation to prevent further infectious spread. Over 80% of patients will present with a painful limb and edema, but <50% present with the more critical symptoms of skin discoloration, crepitus, and vesicles [1]. Therefore, we recommend a small tissue biopsy when a concern exists for a necrotizing soft-tissue infection when physical examination and laboratory values do not provide a clear diagnosis. Ozalay et al. discussed management of debridement versus amputation-based on proximal limb involvement [8]. Due to our patient’s thigh involvement, a formal above-knee amputation was performed.
Conclusion
While extremely rare, non-penetrating necrotizing fasciitis can occur through simple soft-tissue damage – even as mild as an ankle sprain. No other immunocompetent patients were identified with this type of mechanism that transitioned to necrotizing fasciitis in our research. Our goal in reporting this case was to provide an example of maintaining a broad differential in potentially life-preserving cases.
Clinical Message
Necrotizing soft-tissue infections have extreme potential to become a very deadly infection with high morbidity and mortality rates, even if detected early. Thus, it is imperative to maintain a high index of suspicion for atypical presentations of necrotizing fasciitis through a combination of physical examination findings, laboratory values, and biopsy results.
References
1. Fontes RA, Ogilvie CM, Miclau T. Necrotizing soft-tissue infections. J Am Acad Orthop Surg 2000;8:151-8.
2. Stoneback JW, Hak DJ. Diagnosis and management of necrotizing fasciitis. Orthopedics 2011;34:196-202.
3. Lee A, May A, Obremskey WT. Necrotizing soft-tissue infections: An orthopaedic emergency. J Am Acad Orthop Surg 2019;27:e199-206.
4. Stevens DL, Bryant AE. Necrotizing soft-tissue infections. N Engl J Med 2017;377:2253-65.
5. Rupp M, Knapp G, Weisweiler D, Heiss C, Alt V. Intestinal perforation by a toothpick as reason for necrotizing fasciitis. J Bone Jt Infect 2018;3:226-9.
6. Lindsey RW, Resnick L. The clinical challenges of necrotizing fasciitis. JBJS Case Connect 2016;6:e46.
7. Bellapianta JM, Ljungquist K, Tobin E, Uhl R. Necrotizing fasciitis. J Am Acad Orthop Surg 2009;17:174-82.
8. Ozalay M, Ozkoc G, Akpinar S, Hersekli MA, Tandogan RN. Necrotizing soft-tissue infection of a limb: Clinical presentation and factors related to mortality. Foot Ankle Int 2006;27:598-605.
9. Nambiar S, Karippot A, Devasahayam J, Oliver T. Group A streptococci-associated necrotizing fasciitis following cat bite in an immunocompromised patient. Case Rep Crit Care 2017;2017:3718360.
10. Thompson KM, Kruse BT, Hedges MA. Atraumatic clostridial myonecrosis in an immunocompromised host. J Emerg Med 2018;54:e121-3.
11. Neeki M, Dong F, Au C, Toy J, Khoshab N, Lee C, et al. Evaluating the laboratory risk indicator to differentiate cellulitis from necrotizing fasciitis in the emergency department. West J Emerg Med 2017;18:684-9.
12. Wong CH, Khin LW, Heng KS, Tan KC, Low CO. The LRINEC (laboratory risk indicator for necrotizing fasciitis) score: A tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med 2004;32:1535-41.
 |
 |
 |
 |
 |
| Dr. Zachary P Herzwurm | Dr. Cameron S Murphy | Dr. B Gage Griswold | Dr. Colton R J Webber | Dr. Kyle M Mahoney |
| How to Cite This Article: Herzwurm ZP, Murphy CS, Griswold BG, Webber CR, Mahoney KM. From Lateral Ankle Sprain to Above-Knee Amputation: A Unique Case Report of Group A Streptococcus Necrotizing Soft-tissue Infection. Journal of Orthopaedic Case Reports 2020 December;10(9): 52-55. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




