 [box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
Osteochondritis dissecans of the humeral trochlea can be successfully treated with mosaic-type osteochondral autologous transplantation.
Case Report | Volume 10 | Issue 9 | JOCR December 2020 | Page 106-108 | Yoshifumi Harada, Atsuyuki Inui, Takeshi Kokubu, Yutaka Mifune, Hanako Nishimoto, Ryosuke Kuroda. DOI: 10.13107/jocr.2020.v10.i09.1924
Authors: Yoshifumi Harada[1], Atsuyuki Inui[2], Takeshi Kokubu[2], Yutaka Mifune[2], Hanako Nishimoto[2], Ryosuke Kuroda[2]
[1]Department of Orthopaedic Surgery, Kobe Rosai Hospital, Chuo-Ku, Kobe, Hyogo, Japan,
[2]Department of Orthopaedic Surgery, Kobe University, Graduate School of Medicine, Chuo-Ku, Kobe, Hyogo, Japan.
Address of Correspondence:
Dr. Atsuyuki Inui,
Department of Orthopaedic Surgery, Kobe University, Graduate School of Medicine, 7-5-1 Kusunoki-Cho, Chuo-Ku, Kobe – 650-0017, Japan.
E-mail: ainui@med.kobe-u.ac.jp
Abstract
Introduction: The majority of osteochondritis dissecans (OCD) of the elbow occurs in the humeral capitellum in adolescence while OCD in the humeral trochlea is relatively rare. We report a rare case of OCD in the humeral trochlea, which underwent mosaic-type osteochondral autologous transplantation.
Case Report: A 24-year-old man, who was a gymnastic athlete, complained of severe right elbow pain for 9 years. Image findings revealed a trochlear osteochondral defect with intra-articular loose body. Due to the large defect and duration of the disease, autologous osteochondral transplantation form femoral condyle was performed. Two years after surgery, the range of elbow motion was 0° in extension and 120° in flexion. He had no pain on his elbow.
Conclusion: OCD in the humeral trochlea was treated with mosaic-type osteochondral autologous transplantation form femoral condyle. Despite the large trochlear defect, osteochondral transplantation yielded a satisfactory result and this treatment might be an option for treatment of trochlear OCD.
Keywords: Osteochondritis dissecans, trochlea, arthroscopy.
Introduction
The majority of osteochondritis dissecans (OCD) of the elbow occurs in the humeral capitellum in adolescence. In contrast, OCD in the humeral trochlea is relatively rare [1, 2, 3]. The ideal goal of treatment for OCD lesions is to resurface the osteochondral defect with hyaline cartilage and to prevent osteoarthritis. Various surgical methods had been reported [4, 5, 6] depending on the size and location of the defect. For large defects, mosaic-type osteochondral autologous transplantation has showed successful outcome [6]. However, this treatment has not been reported for the management of OCD of the humeral trochlea. We herein present a case of a patient with OCD in the trochlea, who was successfully treated with mosaic-type osteochondral autologous transplantation from the distal femur.
Case Report
A 24-year-old man, who was a gymnastic athlete, complained of severe right elbow pain. When the patient was 15 years old, he first felt pain at the medial side of the elbow while participating in a gymnastics competition. Since then, he experienced occasional right elbow pain but did not undergo further treatment. Nine years after the onset, the elbow pain became worse than he was referred to our hospital. On physical examination, his right elbow was observed to be swollen. The range of elbow motion was 0° in extension and 120° in flexion, with pain at maximum extension. Forearm pronation range was 90° and that for supination was 75°. Plane radiographic examination revealed a loose body at the medial part of trochlea (Fig. 1a-c).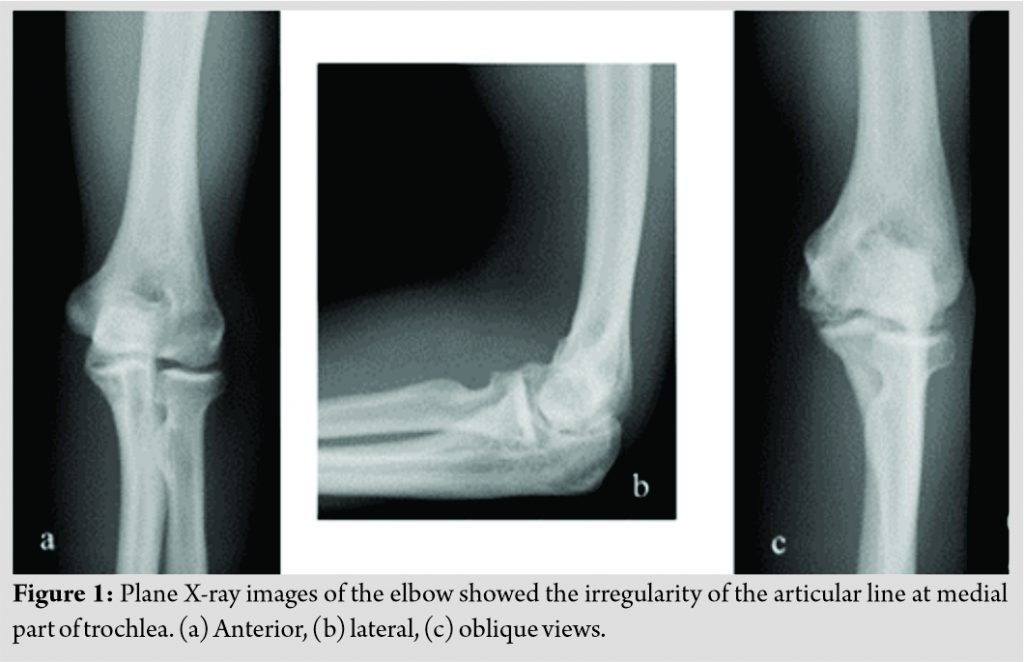 Computed tomography showed a trochlear osteochondral defect with intra-articular loose body. On magnetic resonance imaging (MRI), T2-weighted short inversion time inversion recovery images showed osteochondral fragment separated from the medial part of trochlea with a border showing high signal intensity (Fig. 2a). He was diagnosed with trochlear OCD and treated with oral anti-inflammatory drugs for several months. However, there was no improvement of his elbow pain; therefore, he underwent surgical treatment.
Computed tomography showed a trochlear osteochondral defect with intra-articular loose body. On magnetic resonance imaging (MRI), T2-weighted short inversion time inversion recovery images showed osteochondral fragment separated from the medial part of trochlea with a border showing high signal intensity (Fig. 2a). He was diagnosed with trochlear OCD and treated with oral anti-inflammatory drugs for several months. However, there was no improvement of his elbow pain; therefore, he underwent surgical treatment.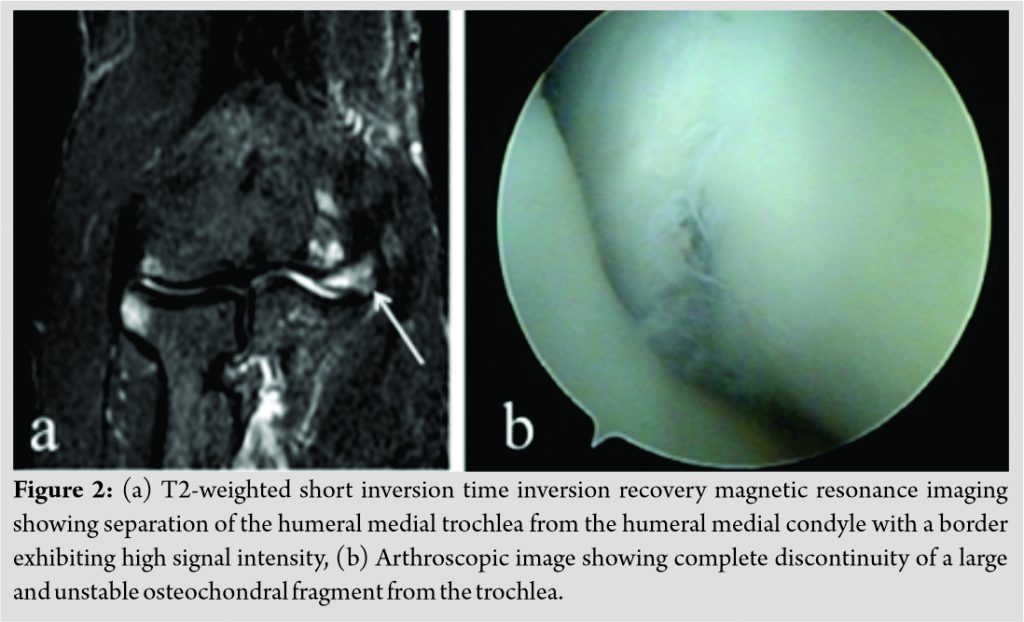
Elbow arthroscopy was performed before osteochondral transplantation. The arthroscopy revealed complete discontinuity of a large and unstable osteochondral fragment from the trochlea (Fig. 2b). After arthroscopy, the trochlea was exposed through a transolecranon approach. The fragment of the trochlea, which was 30 mm in length, 10 mm in width, and 4 mm in thickness, was very unstable (Fig. 3a). Bone marrow stimulation at the osteochondral defect in the trochlea was performed; however, there was no bleeding from the lesion. Hence, we concluded that osteosynthesis would not lead to union of the fragment and the osteochondral fragment was excised from the trochlea. After excision of the fragment, the surrounding degenerative cartilage was curetted until normal bone marrow was exposed. Using a lateral parapatellar approach, three cylindrical osteochondral grafts, each 6.5 mm in diameter, were harvested from the lateral periphery of the femoral condyle. The grafts were transplanted into the trochlear defect (Fig. 3b). The transected olecranon was fixed with K-wire and soft wire by tension band wiring procedure. After 2 weeks of immobilization with a long arm splint at 90° of elbow flexion, active range of motion exercise was commenced. Six months after the surgery, the MRI showed continuity of the cartilage layer between the osteochondral graft and surrounding bone (Fig. 3c). At 2 years after the transplantation, he returned to his job as an athletic medical trainer without elbow pain. Plain radiography showed no progression of the degenerative change.
Discussion
OCD in the humeral trochlea is relatively rare. Trochlear lesions account for 0.5% of OCD lesions that were discovered with plain radiographic evaluation. The etiology for this lesion remains unclear. Yamaguchi et al. demonstrated that the distal aspect of the humerus is relatively hypovascular despite dense profusion proximally [7]. Marshall et al. speculated that repeated forced elbow extension could cause impairment of normal blood supply with resultant chondral/subchondral edema. The edema could lead to increased intraosseous pressure, resulting in decreased blood supply of the watershed area of the trochlea [1]. We suggested this as the causal process of OCD in the intra-articular distal aspect of the humerus. In the present case, we hypothesize that the reiterative bearing pressure, during gymnastics, might have impaired the interosseous blood supply and have caused trochlear OCD. For the treatment of trochlear osteochondral lesions, there are several options such as arthroscopic debridement, drilling, osteosynthesis, and cartilage transplantations depending on the patients’ age and defect size [2]. According to a previous report, a 17-year-old patient who had elbow pain for 12 months was treated using osteosynthesis with autologous bone graft, achieving bone union at 10 months postoperatively [2]. In the present case, we thought that osteosynthesis was not possible because of the age and disease duration. Arthroscopic debridement, drilling, and cartilage transplantation are common solutions for superficial articular defects but are not recommended in deep articular lesions involving subchondral bone. Due to the large size of the bony fragment in the present case, we did not perform arthroscopic debridement or drilling. Osteochondral autologous transplantation has been reported to achieve good clinical result for the treatment of articular cartilage defects of the knee joint [3]. Recently, this technique has been used to reconstruct advanced capitellar OCD lesions in adolescent athletes, and good clinical results have been reported [8, 9]. In our case, the trochlear articular defect had the size of 300 mm2, which was larger compared to the mean defect size (147–183 mm2) previously reported in capitellum OCD [8, 9]. We performed autologous osteochondral transplantation because of the large defect and the disease duration from the onset. Despite the large defect, osteochondral transplantation yielded a satisfactory result and this treatment might be an option for the treatment of trochlear OCD.
Conclusion
OCD in the humeral trochlea was treated with mosaic-type osteochondral autologous transplantation form femoral condyle. Despite the large trochlear defect, osteochondral transplantation yielded a satisfactory result and this treatment might be an option for the treatment of trochlear OCD.
Clinical Message
Mosaic-type osteochondral transplantation yielded a satisfactory result and this treatment might be an option for the treatment of trochlear OCD.
References
1. Marshall KW, Marshall DL, Busch MT, Williams JP. Osteochondral lesions of the humeral trochlea in the young athlete. Skeletal Radiol 2009;38:479-91.
2. Joji S, Murakami T, Murao T. Osteochondritis dissecans developing in the trochlea humeri: A case report. J Shoulder Elbow Surg 2001;10:295-7.
3. Patel N, Weiner SD. Osteochondritis dissecans involving the trochlea: Report of two patients (three elbows) and review of the literature. J Pediatr Orthop 2002;22:48-51.
4. Wiesler ER, Sarlikiotis T, Rogers S, Papadonikolakis A, Poehling G. Arthroscopic debridement for osteochondral injury of the elbow trochlea: A case report with a long-term follow-up. J Shoulder Elbow Surg 2011;20:e18-22.
5. Iwsaki N, Yamane S, Ishikawa J, Majima T, Minami A. Osteochondritis dissecans involving the trochlea of the humerus treated with transplantation of tissue-engineered cartilage: A case report. J Shoulder Elbow Surg 2008;17:e22-5.
6. Weigelt L, Siebenlist S, Hensler D, Imhoff B, Vogt S. Treatment of osteochondral lesions in the elbow: Results after autologous osteochondral transplantation. Arch Orthop Trauma Surg 2015;135:627-34.
7. Yamaguchi K, Sweet FA, Bindra R, Morrey BF, Gelberman RH. The extraosseous and intraosseous arterial anatomy of the adult elbow. J Bone Joint Surg Am 1997;79:1653-62.
8. Iwasaki N, Kato H, Ishikawa J, Masuko T, Funakoshi T, Minami A. Autologous osteochondral mosaicplasty for osteochondritis dissecans of the elbow in teenage athletes. J Bone Joint Surg Am 2009;91:2359-66.
9. Yamamoto Y, Ishibashi Y, Tsuda E, Sato H, Toh S. Osteochondral autograft transplantation for osteochondritis dissecans of the elbow in juvenile baseball players: Minimum 2-year follow-up. Am J Sports Med 2006;34:714-20.
 |
 |
 |
 |
 |
| Dr. Yoshifumi Harada | Dr. Takeshi Kokubu | Dr. Yutaka Mifune | Dr. Hanako Nishimoto | Dr. Ryosuke Kuroda |
| How to Cite This Article: Harada Y, Inui A, Kokubu T, Mifune Y, Nishimoto H, Kuroda R. Osteochondritis Dissecans of the Humeral Trochlea Treated with Mosaic-type Osteochondral Autologous Transplantation. Journal of Orthopaedic Case Reports 2020 December;10(9): 106-108. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




