Even though the Giant cell tumor of the knee consists a rather rare intra-articular entity, orthopedic surgeons should be aware of this lesion and suspect it following clinical and imaging findings, and furthermore, arthroscopy should be considered as a trustworthy choice.
Dr. Dimitrios A Flevas,
Department of Arthroscopy and Orthopaedic Surgery,
Metropolitan Hospital, Athens, Greece.
E-mail: dflevas@gmail.com
Introduction: Tenosynovial giant-cell tumor (GCT) arising from cruciate ligaments consists a rather rare entity. Predominantly areas where this tumor appears are the palmar sides of fingers and toes. The involvement of larger joints such as the knee or the ankle is rather rare, but, in the case of synovial joints, the knee joint is particularly affected. Furthermore, rare seems to be the intra-articular localization of the tenosynovial GCT of the tendon sheath. Hereby, we present an arthroscopic approach of treatment with two cases.
Case Reports: The first case was a 32-year-old male with a GCT arising from the anterior cruciate ligament (ACL). The second case was a 26-year-old male with a GCT arising from the posterior cruciate ligament (PCL). In the first case, a round-shaped mass with a reddish-brown color was located just anterior to the ACL and impeded the full extension of the knee joint, while, in the second case, a well-circumscribed oval-shaped mass was found with a peduncle attached to the synovium of the PCL. After arthroscopic excision, both patients became asymptomatic, with complete lack of pain and full ROM.
Conclusions: There is a lack of clinical features for the GCT of the knee, and thus, a thorough clinical examination is prudent. Usually, the diagnosis is set after an investigation based on suspicion. This entity can present with symptoms of instability and patients may present signs of mechanical derangement. With the knee joint, meniscal symptoms and locking are often present. The best non-invasive technique to diagnose this tumor has been reported to be the magnetic resonance imaging. Arthroscopic excision has been reported as a safe and effective procedure for treatment.
Keywords: Anterior cruciate ligament, posterior cruciate ligament, knee block, giant cell tumor.
Tenosynovial giant-cell tumor (GCT) arising from cruciate ligaments consists a rather rare entity. Chassiagnac, who first described the tenosynovial GCT, called it “cancer of tendon sheath” [1]. This kind of tumor arises from the synovial of the fibrous tissue surrounding the joints, tendon sheaths, mucosal bursas, and tendons [2, 3]. Predominantly areas where this tumor appears are the palmar sides of fingers and toes [4]. The involvement of larger joints such as the knee or the ankle is not usual, but in the case of synovial joints, the knee joint is particularly affected [4, 5]. In addition, the intra-articular localization of the tenosynovial GCT of the tendon sheath seems to be rather rare [6]. Kim et al. first reported a case of a localized and intra-articular type of tenosynovial GCT of the knee attached to the synovium on the anterior horn of the medial meniscus in 1995 [7], while Otsuka et al., in 1996, first reported a case of intra-articular tenosynovial GCT arising from the anterior cruciate ligament (ACL) [8]. The number of similar cases reported is limited [6, 8, 9]. Furthermore, the GCT arising from the posterior cruciate ligament (PCL) seems to be also rare with six cases presented to the English literature to our knowledge [2, 10, 11, 12, 13, 14]. The GCT of the tendon sheath is morphologically identical to the localized pigmented villonodular synovitis (PVNS) [15], whose most common location is the knee [15, 16, 17]. Although PVNS consists typically a monoarticular proliferative condition that most affects the knee [16], the morphological identical GCT of the tendon sheath arising from the ACL remains an uncommon entity [6]. The tenosynovial GCT has four clinicopathological variants: The localized type, the diffuse extra-articular, the diffuse intra-articular, and the malignant [5, 18]. The localized type of tenosynovial GCT is defined as a circumscribed lesion that is microscopically not infiltrating into the fat of skeletal muscles [5]. GCT of the tendon sheath typically occurs between the ages of 30 and 50 with a female predominance for some researchers [19], while others support a male predominance [9]. Due to the rarity of the GCT arising from the cruciate ligaments [6], the arthroscopic treatment of these entities remains uncommon. Hereby, we present the arthroscopic treatment of two such cases, one of a 32-year-old male with a GCT arising from the ACL and one of a 26-year-old male with a GCT arising from the PCL.
Case report 1
Arthroscopic removal of a GCT arising from the ACL
A 32-year old male with a free medical history presented with a right knee injury after a soccer game. He was an amateur player who played a full time game every week. There was no history of trauma before that injury. The patient complained of pain on his right knee, effusion, and locking symptoms. There was no sense of giving way. There were no complaints of pain or swelling of any other joint. On clinical examination, there was a 15° extensor lag in his injured knee, mild signs of effusion, and tenderness along the lateral joint line. In addition, Lachman-Noulis test, Pivot-Shift test, McMurray, and Apley test were negative. Routine laboratory investigations were normal. Anteroposterior and lateral radiographs came up normal and the patient underwent an magnetic resonance imaging (MRI) scan on his right knee. On the MRI examination, there was a lesion with a hypointense signal in the sagittal T1-weighted images that obscured the ACL (Fig. 1, 2).
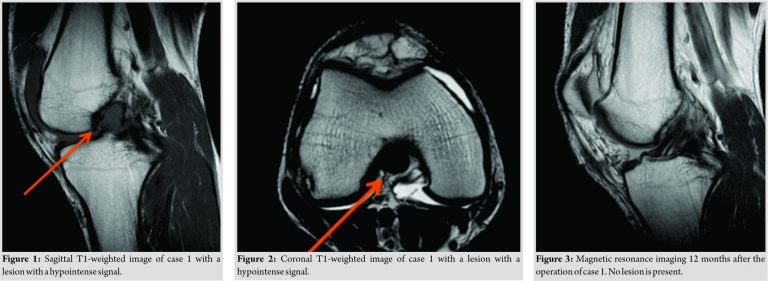
Due to the symptoms, an arthroscopic excision of the lesion was decided. In the arthroscopic examination, the menisci, PCL, and articular cartilage were normal. A round mass with a reddish-brown color was located just anterior to the ACL and impeded the full extension of the knee joint. This lesion was excised with the use of basket forceps and a motorized shaver was used at the end of the removal. After the complete removal of the lesion, a repeat Lachman-Noulis test revealed a stable knee. The microscopic examination reported a GCT of tendon sheath. The presence of multinucleated giant cells was reported, along with a presence of mononuclear cells with low-grade cellular multiplication. Range of motion exercises and partial weight-bearing started the day after the operation. The patient became asymptomatic without pain or loss of extension and returned to full athletic activities 3 weeks post-operatively A second MRI performed 12 months after the operation. In the sagittal plane, the lesion was completely disappeared and the two bundles of the native ACL were clearly defined (Fig. 3). The patient had no further complains following the operation and there was no recurrence on the 36-months follow-up.
Case report 2
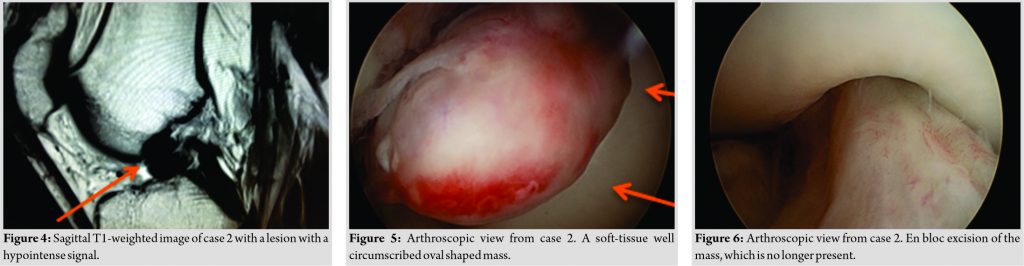
Arthroscopic removal of a GCT arising from the PCL.
A 26-year-old male with a free past medical history presented with a right knee injury after a soccer game. He was an amateur soccer player who got injured during his 24th game of the season with any prior injury. Immediately after the injury, he presented with pain and effusion on his right knee and locking symptoms and he was unable to continue his athletic activities and began limping. There were no complaints of pain or swelling of any other joint. On clinical examination, there were mild signs of effusion, a significant 20° extensor on his injured knee, while no signs of ligament rupture or meniscal tear were present. In addition, Lachman-Noulis test, Pivot-Shift test, McMurray, and Apley test were negative, while routine laboratory tests were normal. Anteroposterior and lateral radiographs came up normal and the patient underwent an MRI scan on his right knee. The MRI reported a well-circumscribed soft-tissue mass with dimensions of 1.3 × 1.9 cm. The mass was regular contoured and localized in the fossa intercondyloidea, in front of the ACL and behind the transverse meniscal ligament. On T1-weigted MRI sequences, the lesion was hypointense (Fig. 4), while on T2-weighted MRI sequences, the lesion was hyperintense. Furthermore, a mild effusion (Grade I) was noticed. No other findings from the cruciate ligaments and the menisci or any lesions to the articular cartilage were noticed. After assessing the patient’s clinical findings and the MRI findings, an arthroscopy was scheduled. Arthroscopy was performed using the standard anterolateral and anteromedial portals. A soft-tissue well-circumscribed oval-shaped mass was found (Fig. 5). It was encapsulated and its size was similar to the MRI findings, approximately 1.3 × 1.9 cm. The mass was mobile and had a peduncle attached to the synovium of the PCL. During the extension of the knee, the mass was impinged between the femoral trochlea and the anterior tibial plateau in front of the ACL. At the area of the femoral trochlea, there was a cartilage lesion Grade II-III according to Outerbridge [20] classification, probably due to the impact of the mass during the knee extension. No lesions were found on the menisci, the popliteal tendon or the ACL. The mass was excised en bloc (Fig. 6) using the anterolateral portal and was sent for histopathological examination. Microscopic examination reported a GCT of tendon sheath with presence of multinucleated giant cells and plenty of mononuclear cells with low-grade cellular multiplication, blending with collagen matrix (Fig. 7).

The patient’s recovery was uneventful. He underwent physiotherapy with immediate load bearing of the operated limb, progressive enforcement, and proprioception exercises. He was able to return to his sports activities within a month. At 6-month follow-up after arthroscopic removal, the patient was asymptomatic and had a full range of motion of his right knee without pain, effusion, or extension lack.
The two cases presented here describe an unusual entity in an even more rare form. The description we provided regarding their location and the arthroscopic removal that we selected, we believe that will help orthopedic surgeons in their decision-making. The etiology of GCT of the tendon sheath remains unclear. There are many names given to this entity that reflects its clinicopathologic heterogeneity and historical differences. The various terms used to describe the tumor are: Tenosynovial giant cell, nodular tenosynovitis, PVNS, fibroxanthoma, and fibrous histiocytoma [21]. Many factors have been proposed as possible causes of GCT of the tendon sheath, including inflammation, trauma, toxin, allergy, clonal chromosomal abnormalities, and aneuploidy [22, 23]. Initially, the entity regarded as an inflammatory disease; however, the finding of aneuploidy in certain cases and the demonstration of clonal chromosomal abnormalities strongly support a neoplastic origin [24]. GCT of tendon sheath consists the most common form of tenosynovial GCTs. About 75% of these tumors are found in the digits, especially on the volar surfaces of the fingers and are the second most common tumors of the hand after the ganglion [15]. There is a lack of clinical features for the GCT of the knee, and thus, a thorough clinical examination is prudent in such cases. Usually, the diagnosis is set after an investigation based on suspicion [4, 8]. This entity can present with symptoms of instability and can be misdiagnosed as an ACL tear [9]. Patients present signs of mechanical derangement. With the knee joint, meniscal symptoms and locking are often present. Both our patients presented with this kind of symptoms. They both had lack of extension and effusion after knee injury. The clinical appearance of the injured knees was suspicious, and further, investigation with MRI scans was decided. The best non-invasive technique to diagnose this tumor has been reported to be the MRI [25, 26]. A finding that should rise the suspicion of such a tumor and place it in the differential diagnosis is a hypointense lesion in T1-weigted MRI sequences which obscure the cruciate ligaments and in T2-weighted MRI sequences that the lesion is hyperintense. Malignant tumors, such as synovial sarcoma and benign soft-tissue tumors, should be kept in mind in differential diagnosis. MRI diagnosis must be confirmed by histopathological examination. The tumor typically presents as a slowly growing, painless mass of size between 0.5 and 4.0 cm. Lesions of the knee are usually intra-articular and may cause pain and joint effusion. Following local excision, the digital tumors have some tendency to recur at 10–20%, but the intra-articular tumors in the knee joint recur with a greater frequency [6, 27]. The pathogenesis of GCT is not known. In some cases, post-traumatic reaction is the cause of this condition, whereas inflammation or metabolic disorders are other causes of this tumor [28]. These two patients were amateur soccer players with many traumatic episodes every year. Therefore, these cases may support the hypothesis of traumatic genesis of GCT. Arthroscopic excision has been reported as a safe and effective procedure for the treatment of these tumors [29, 30, 31, 32]. To the authors’ knowledge, there is a limited number of cases of tenosynovial giant cell tumors arising from the ACL published [6, 8, 9]. In all these cases, arthroscopic excision of the tumor was performed and that is the treatment method followed in our case.
GCT of the knee consists a rather rare inrtra-articular entity, which can be misdiagnosed or may require extensive investigation because of its lack of clinical characteristics. Other tumors must be considered in the differential diagnosis and excluded while MRI may prove very useful. After diagnosis arthroscopy is the choice for treatment.
We believe that though the GCT of the knee consists a rather rare intra-articular entity, orthopedic surgeons be should be aware of this lesion and should suspect it following clinical and imaging findings. Furthermore regarding treatment of this entity, arthroscopy should be considered as a trustworthy choice.
References
- 1.Enzinger FM, Weiss SW. Benign tumors and tumor-like lesions of synovial tissue. In: Tissue Tumors. 2nd ed. St. Louis: Mosby; 1988. p. 638-58. [Google Scholar]
- 2.Kim R, Lee J, Lee K. Localized pigmented villonodular synovitis attached to the posterior cruciate ligament of the knee. Arthroscopy 2003;19:E32-5. [Google Scholar]
- 3.Sun C, Sheng W, Yu H, Han J. Giant cell tumor of the tendon sheath: A rare case in the left knee of a15-year-old boy. Oncol Lett 2012;3:718-20. [Google Scholar]
- 4.Kuhnen C, Muller KM, Rabstein S, Kasprzynski A, Herter P. Tenosynovial giant cell tumor. Pathologe 2005;26:96-110. [Google Scholar]
- 5.Miettinen MM. Diagnostic Soft Tissue Pathology. New York, USA: Churchill Livingstone; 2002. [Google Scholar]
- 6.Lee JH, Wang SI. A tenosynovial giant cell tumor arising from femoral attachment of the anterior cruciate ligament. Clin Orthop Surg 2014;6:242-4. [Google Scholar]
- 7.Kim SJ, Choi NH, Lee SC. Tenosynovial giant-cell tumor in the knee joint. Arthroscopy 1995;11:213-5. [Google Scholar]
- 8.Otsuka Y, Mizuta H, Nakamura E, Kudo S, Inoue S, Takagi K. Tenosynovial giant-cell tumor arising from the anterior cruciate ligament of the knee. Arthroscopy 1996;12:496-9. [Google Scholar]
- 9.Agarwala S, Agrawal P, Moonot P, Sobti A. A rare case of giant cell tumour arising from anterior cruciate ligament: Its diagnosis and management. J Clin Orthop Trauma 2015;6:140-3. [Google Scholar]
- 10.Sayed W, Daghfous E, Salah MB, Mahjoub S, Dridi M, Annabi H, et al. Intra-articular tenosynovial giant cell tumor arising from the posterior cruciate ligament. Tunis Med 2015;93:109-10. [Google Scholar]
- 11.Xu Z, Mao P, Chen D, Shi D, Dai J, Yao Y, et al. Tenosynovial giant cell tumor arising from the posterior cruciate ligament: A case report and literature review. Int J Clin Exp Pathol 2015;8:6835-40. [Google Scholar]
- 12.Camillieri G, Di Sanzo V, Ferretti M, Calderaro C, Calvisi V. Intra-articular tenosynovial giant cell tumor arising from the posterior cruciate ligament. Orthopedics 2012;35:e1116-8. [Google Scholar]
- 13.Aksoy B, Ertürer E, Toker S, Seçkin F, Sener B. Tenosynovial giant cell tumour of the posterior cruciate ligament and its arthroscopic treatment. Singapore Med J 2009;50:e204-5. [Google Scholar]
- 14.Sheppard DG, Kim EE, Yasko AW, Ayala A. Giant-cell tumor of the tendon sheath arising from the posterior cruciate ligament of the knee: A case report and review of the literature. Clin Imaging 1998;22:428-30. [Google Scholar]
- 15.Lucas DR. Tenosynovial giant cell tumor: Case report and review. Arch Pathol Lab Med 2012;136:901-6. [Google Scholar]
- 16.Muscolo D, Makino A, Costa-Paz M, Ayerza M. Localized pigmented villonodular synovitis of the posterior compartment of the knee: Diagnosis with magnetic resonance imaging. Arthroscopy 1995;11:482-5. [Google Scholar]
- 17.Dines JS, DeBerardino TM, Wells JL, Dodson CC, Shindle M, DiCarlo EF, et al. Long-term follow-up of surgically treated localized pigmented villonodular synovitis of the knee. Arthroscopy 2007;23:930-7. [Google Scholar]
- 18.Weiss S, Goldblum J, Folpe A. Enzinger and Weiss’s Soft Tissue Tumors. 4th ed. Philadelphia, PA, USA: Mosby, Elsevier; 2008. [Google Scholar]
- 19.Ushijima M, Hashimoto H, Tsuneyoshi M, Enjoji M. Giant cell tumor of the tendon sheath (nodular tenosynovitis): A study of 207 cases to compare the large joint group with the common digit group. Cancer 1986;57:875-84. [Google Scholar]
- 20.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br 1961;43-B:752-7. [Google Scholar]
- 21.Jones FE, Soule EH, Coventry MB. Fibrous xanthoma of synovium (giant-cell tumor of tendon sheath, pigmented nodular synovitis). A study of one hundred and eighteen cases. J Bone Joint Surg Am 1969;51:76-86. [Google Scholar]
- 22.Reilly KE, Stern PJ, Dale JA. Recurrent giant cell tumors of the tendon sheath. J Hand Surg Am 1999;24:1298-302. [Google Scholar]
- 23.Abdul-Karim FW, El-Naggar AK, Joyce MJ, Makley JT, Carter JR. Diffuse and localized tenosynovial giant cell tumor and pigmented villonodular synovitis: A clinicopathologic and flow cytometric DNA analysis. Hum Pathol 1992;23:729-35. [Google Scholar]
- 24.Fletcher CD, Unni KK, Mertens F, editors. World Health Organization Classification of Tumors, Pathology and Genetics of Tumors of Soft Tissue and Bone, Giant Cell Tumour of Tendon Sheath. Lyon: IARC Press; 2002. p. 110-1. [Google Scholar]
- 25.Kramer DE, Frassica FJ, Frassica DA, Cosgarea AA. Pigmented villonodular synovitis of the knee: Diagnosis and treatment. J Knee Surg 2009;22:243-54. [Google Scholar]
- 26.Wan JM, Magarelli N, Peh WC, Guglielmi G, Shek TW. Imaging of giant cell tumour of the tendon sheath. Radiol Med 2010;115:141-51. [Google Scholar]
- 27.Wood GS, Beckstead JH, Medeiros LJ, Kempson RL, Warnke RA. The cells of giant cell tumor of tendon sheath resemble osteoclasts. Am J Surg Pathol 1988;12:444-52. [Google Scholar]
- 28.Spahn G, Bousseljot F, Schulz HJ, Bauer T. Arthroscopic resection of an extra-articular tenosynovial giant cell tumor from the ankle region. Arthroscopy 2003;19:E8-11. [Google Scholar]
- 29.Bojanic I, Ivkovic A, Dotlic S, Ivkovic M. Localized pigmented villonodular synovitis of the knee: Diagnostic challenge and arthroscopic treatment: A report of three cases. Knee Surg Sports Traumatol Arthrosc 2001;9:350-4. [Google Scholar]
- 30.Kubat O, Mahnik A, Smoljanovic A, Bojanic I. Arthroscopic treatment of localized and diffuse pigmented villonodular synovitis of the knee. Coll Antropol 2010;34:1467-72. [Google Scholar]
- 31.Loariaut P, Dijan P, Boyer T, Bonvarlet J, Delin C, Makridis K. Arthroscopic treatment of localized pigmented villonodular synovitis of the knee. Knee Surg Sports Traumatol Arthrosc 2012;20:1550-3. [Google Scholar]
- 32.de Ponti A, Sansone V, Malchere M. Result of arthroscopic treatment of pigmented villonodular synovitis of the knee. Arthroscopy 2003;19:602-7. [Google Scholar]






