 [box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
Orthopedic surgeons should consider the flexor hallucis longus entrapment as a differential diagnosis of posterior ankle pain.
Case Report | Volume 11 | Issue 4 | JOCR April 2021 | Page 70-74 | Nobuaki Chinzei, Noriyuki Kanzaki, Kanto Nagai, Masahiko Haneda, Tetsuya Yamamoto, Ryosuke Kuroda. DOI: 10.13107/jocr.2021.v11.i04.2158
Authors: Nobuaki Chinzei[1],[2], Noriyuki Kanzaki[1], Kanto Nagai[1], Masahiko Haneda[1],[2], Tetsuya Yamamoto[1], Ryosuke Kuroda[1]
[1]Department of Orthopaedic Surgery, Kobe University Graduate School of Medicine, Kobe, 650-0017, Japan,
[2]Department of Orthopaedic Surgery, Hyogo Rehabilitation Center, Kobe, 651-2181, Japan.
Address of Correspondence:
Dr. Noriyuki Kanzaki,
Department of Orthopaedic Surgery, Kobe University Graduate School of Medicine, 7-5-1 Kusunoki-cho, Chuo-ku, Kobe 650-0017, Japan.
E-mail: kanzaki@med.kobe-u.ac.jp
Abstract
Introduction: Stenosing tenosynovitis is a chronic disorder frequently observed in finger triggering of a digit. Regarding the toes, although entrapment of the flexor hallucis longus (FHL) has already been reported in a few cases among sports players, the clinical condition is uncommon. Besides, the case without any specific causes is particularly rare.
Case Report: We report the case of a 26-year-old male with FHL entrapment. Even though he was unaware of any cause, he felt tenderness on the posteromedial side of his left ankle, and his great toe was locked in the flex position. Magnetic resonance imaging indicated effusion in the tendon sheath of the FHL and the possibility of a partial tear of the FHL. We hypothesized that the scar tissue secondary to the partial tear of the FHL may have been irritated at the retrotalar pulley below the sustentaculum tali, where the FHL glides. Therefore, posterior ankle arthroscopy was performed for the treatment of the FHL entrapment.
Conclusion: Orthopedic surgeons should list this pathology as a differential diagnosis of posterior ankle pain, even in non-athletes.
Keywords: ankle arthroscopy, flexor hallucis longus, stenosing tenosynovitis.
Introduction
Entrapment of the flexor hallucis longus (FHL), also known as the hallux saltans, is relatively uncommon. Such pathology has often been found in ballet dancers and patients engaged in other types of sports activity [1, 2, 3, 4]. Repeated excessive movements of the foot and ankle joint result in irritation, inflammation, and hypertrophy of the FHL tendon [5]. FHL entrapment can cause posteromedial pain and trigger the great toe, disrupting sporting activities among a wide range of athletes, from amateur to professional. Interestingly, we experienced a case of FHL entrapment without any specific causes in a non-athlete male. Here, we report a release of the FHL, treated with posterior ankle arthroscopy, to bring awareness of this case to daily clinical practice.
Case Report
A 26-year-old male patient became aware of posterior ankle pain before seeking treatment. He was unaware of any cause, such as a history of trauma in the past 6 months. The patient began having difficulty in bending his left great toe 1 month after noticing the posterior ankle pain. In addition, he felt a snapping at his posterior ankle with active and passive ankle motion. Initially, he visited his primary care physician several times and received local anesthetic injections without steroids into his posterior ankle space. However, his symptoms did not improve, and he was referred to our hospital in February 2016. The patient was a licensed cook and had no significant medical history.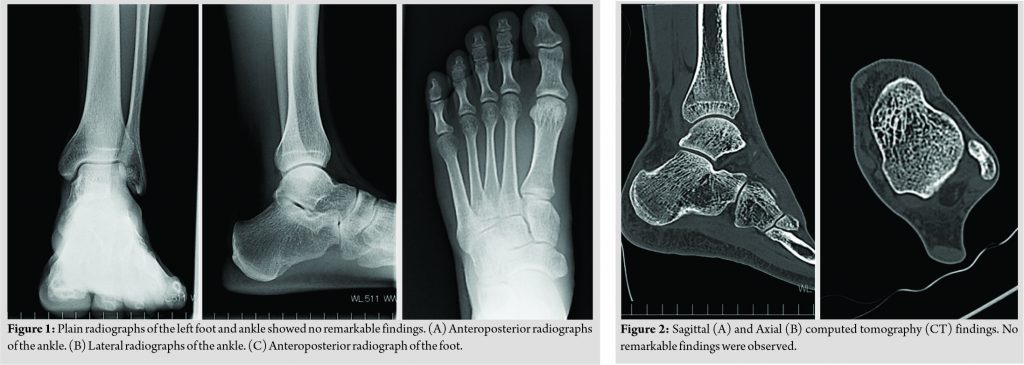
Physical examination revealed tenderness on the posteromedial side of his left ankle. His great toe was locked in the flex position when he actively flexed it. It could be corrected by passive dorsiflexion, associated with local pain, clicking, and popping sounds at the posterior ankle. Neurovascular examination and range of foot and ankle motion were normal. Neither radiographs nor computed tomography (CT) of his left foot and ankle revealed remarkable findings, such as osseous lesions, indicating the cause of his symptoms (Fig. 1a-c and 2a, b). Magnetic resonance imaging (MRI) indicated effusion in the tendon sheath of the FHL and the possibility of a partial tear of the FHL (Fig. 3a, b). Since the patient’s symptoms were not relieved with non-surgical treatments, including the injection of local anesthesia and physical therapies, he received surgery. We hypothesized that the scar tissue secondary to the partial tear of the FHL may have been irritated at the retrotalar pulley below the sustentaculum tali, where the FHL glides.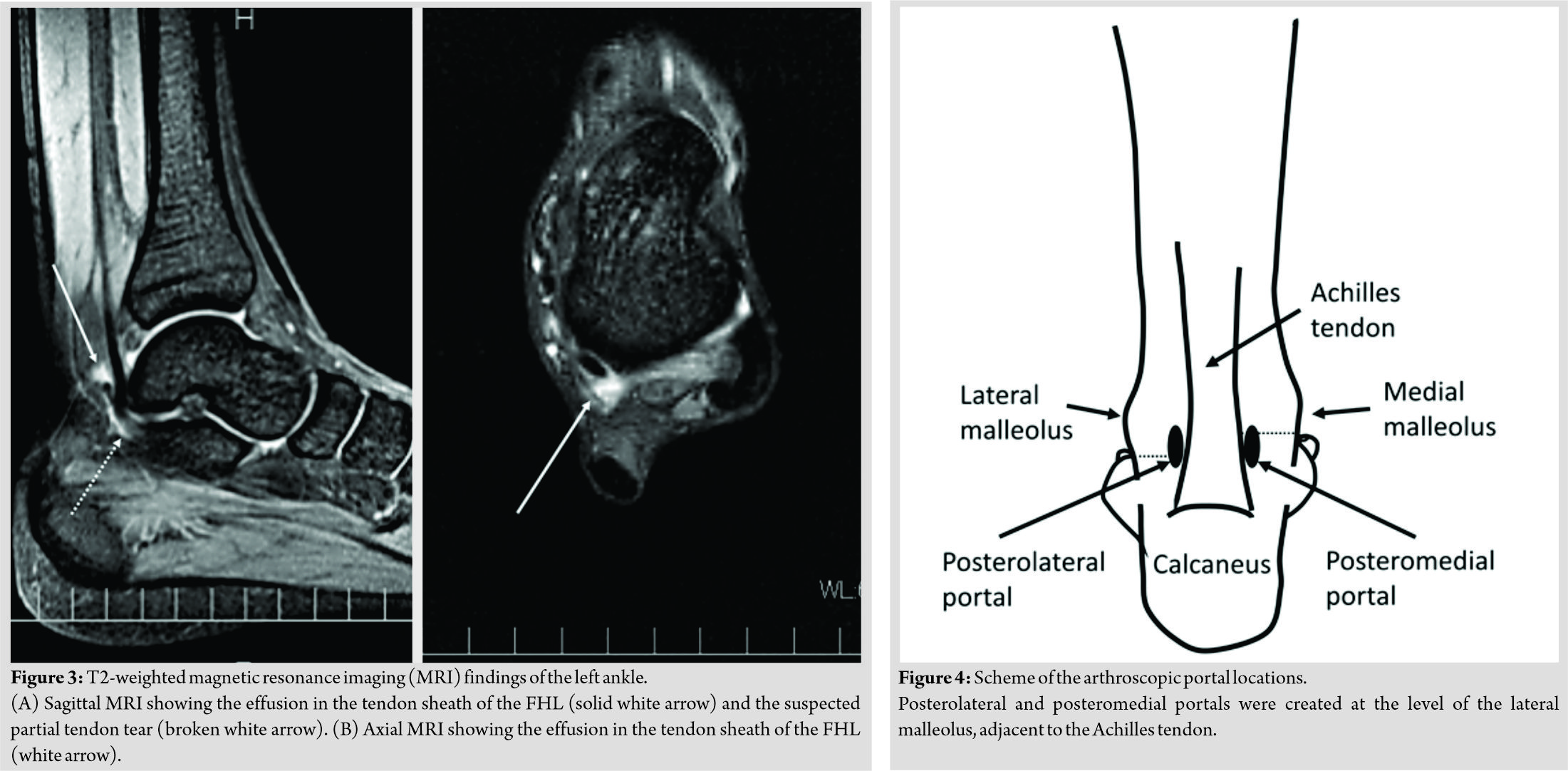
During the surgical procedure, the patient was placed in the prone position, and posterior ankle arthroscopy was performed. Posterolateral and posteromedial portals were created at the level of the lateral malleolus, adjacent to the Achilles tendon (Fig. 4). A 4 mm 30° arthroscope was introduced through the portals to create the working space by removing soft tissues using a shaver. The FHL was identified by dissecting the medial side of the posterior process of the talus (Fig. 5a). The FHL was degenerative, with a partial tear, and the proximal tendon at zone 1 was thickened by forming a pulley-like fibrous band near the fibro-osseous tunnel below the sustentaculum tali. Synovitis was evident around the FHL. The snapping of the FHL at the fibro-osseous tunnel was reproduced by plantarflexion and dorsiflexion of the great toe. Therefore, all fibrous tissues, including the entrance of the fibro-osseous tunnel that compressed the FHL at zone 2, were removed to clarify the FHL tendon itself (Fig. 5b-d and 5e). The FHL tendon was able to glide smoothly with no residual stenosis at the fibro-osseous tunnel. The movement of the great toe was improved. Finally, the procedure was completed with skin closure. An elastic bandage was placed around the lower extremity, and the patient was encouraged to move his ankle and toes actively. Weight-bearing was allowed as tolerated after surgery. Six months following surgery, his symptom remained asymptomatic with a good clinical course. Neither intraoperative nor postoperative complications were observed. The patient provided informed consent to publish his case.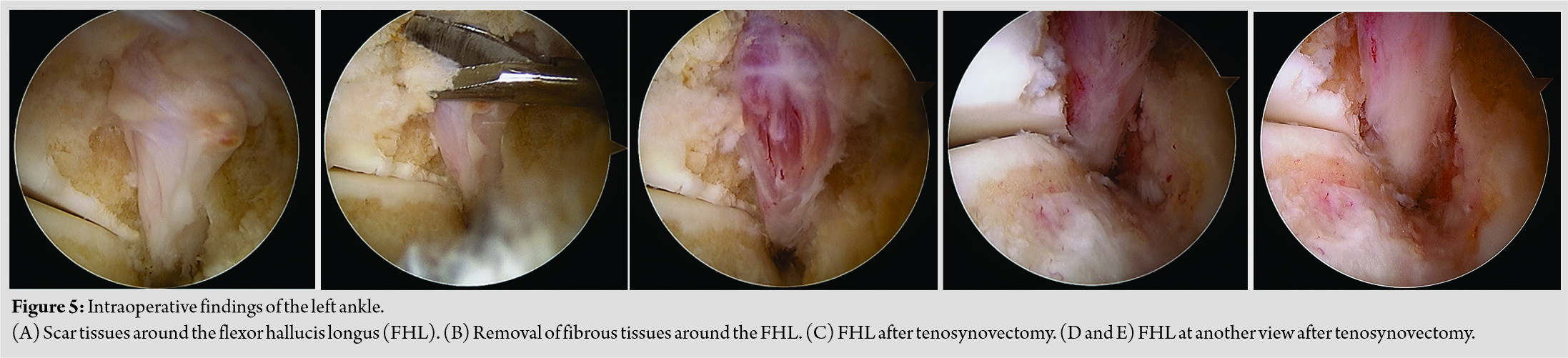
Discussion
Herein, we experienced FHL entrapment caused by scar formation associated with a partial tear of the FHL, without any apparent predisposing factors in a non-athletic male. Stenosing tenosynovitis is a chronic disorder frequently observed in finger triggering of a digit during flexion and subsequent snapping at extension [6]. Trigger finger is mainly caused by the inflammation in the flexor tendon sheath and thickening of the pulleys [6, 7]. Regarding the toes, although stenosing tenosynovitis of the FHL has already been reported in a few cases, the clinical condition is rare [7, 8]. It is recognized as hallux saltans, and most cases are observed among sports players, especially ballet dancers [4, 9]. Purushothaman et al. described details of specific postures such as demi pointe and en pointe that ballet dancers repeat [10]. Demi pointe is the position where the dancer stands on the ball of the foot, and the entire body weight is borne by the head of the metatarsals and the toes. En pointe is the position where the dancer stands on the tip of the toes. The authors mentioned that such repetitive postures burden the FHL tendon and maybe the reason why most cases of FHL entrapment are reported in ballet dancers. Anatomy of the FHL is also well summarized by Purushothaman et al. [10]. Briefly, the FHL is a muscle of the deep posterior compartment of the leg, which arises from the lower two-thirds of the posterior surface of the fibula and the adjacent interosseous membrane. Fibers pass obliquely downward and medially to form the tendon that passes distally through a groove on the posterior surface of the tibia. The tendon then passes between the lateral and medial tubercles of the talus. Beyond the talus, it enters a groove on the undersurface of the sustentaculum tali, where the groove is converted into a fibro-osseous tunnel by a fibrous sheath. Beyond this tunnel, the tendon passes between the two heads of the flexor hallucis brevis. Close to the base of the first phalanx of the big toe, the tendon passes between the medial and lateral sesamoids present within the two heads of the flexor hallucis brevis. The tendon gets inserted into the base of the second phalanx. In this pathway, another perspective of the cause of FHL entrapment is that it is compressed by anatomic variants such as os trigonum and Stieda’s process [10]. Respectively, os trigonum is an accessory ossicle separated from the talus, and Stieda’s process is the long lateral tubercle of the talus. Knot of Henry is also recognized as one of the causes of FHL entrapment, which is a fibrous thickening at the crossing area of FHL and flexor digitorum longus [11]. In our case, the patient’s great toe was locked in flexion when he actively flexed it. It was possible to correct the position by passive dorsiflexion, but this was associated with local pain, clicking, and popping sounds at the posterior ankle. Similar preoperative physical findings have been reported by Funasaki et al., which strongly indicated the existence of FHL entrapment [12]. Nevertheless, the possibility of another disease such as Hallux limitus should be considered when the limited flexibility of the great toe is encountered [13]. Hallux limitus puts the great toe at risk of developing osteoarthritic changes, even though it still allows the great toe some mobility. These changes can make the great toe completely rigid, a condition known as hallux rigidus [14]. Another rare cause of FHL entrapment, as reported by Chang et al., is the presence of the plantar capsular accessory ossicle at the interphalangeal joint of the great toe [15]. They concluded that ultrasonography was a better diagnostic method than radiographs to visualize the plantar capsular accessory ossicle due to its lack of ossification. Martinez-Salazar et al. also demonstrated the FHL entrapment by using dynamic sonography, indicating the thickening of the FHL adjacent to the fibrous band at the medial ankle [7]. Although we did not perform dynamic sonography in this study, we agree with these authors that this evaluation will provide valuable information like real-time inspection of tendon motion and visual confirmation of the entrapment [7, 15]. Therefore, the diagnostic efficacy should be enhanced by combining imaging modalities, such as ultrasonography, radiographs, CT, and MRI. In our case, no specific causes, such as a history of trauma or sports activity, were observed. Furthermore, no anatomic variance was detected by both preoperative images including radiographs, CT, MRI, and intraoperative findings. Because of the absence of degenerative changes in the first metatarsophalangeal joint, our case was also described as one of the examples of pseudo hallux rigidus as reported elsewhere [16, 17]. Therefore, it is worth reporting our case of a patient with FHL entrapment, even with no specific causes. In addition, clinicians should be aware of this pathology as a preoperative differential diagnosis of posterior ankle pain. Concerning treatment options, non-surgical treatment is the first choice for FHL entrapment, as recommended by Hamilton [18]. If non-surgical treatment fails to provide adequate results, surgical treatment can be considered. Failure or recurrence of the symptoms may indicate the longitudinal tears in the tendon [4]. Open procedures have been performed for releasing the FHL tendon [5, 10]. However, current trends have shifted from open surgeries to arthroscopic procedures because of their reduced invasiveness, leading to less postoperative pain, shortening hospitalization, and enabling an early return to daily activities [7]. On the other hand, we should be aware that there are potential limitations and complications associated with arthroscopic procedures, such as the difficulty in repairing a ruptured tendon, the damage to the medial branch of the tibial nerve, and the damage to the Achilles tendon as previously reported [12]. Taking this fact into consideration, we chose posterior ankle arthroscopy for the treatment of this patient, paying careful attention to prevent such complications. Intraoperative findings showed synovitis around the FHL, a degenerative and partially torn FHL, and thickening of the proximal FHL due to a fibro-osseous tunnel below the sustentaculum tali, as indicated by the failure of the conservative treatment. In general, the FHL abruptly changes its direction at this level of the talus, increasing the risk of tendon degeneration and inflammation. Petersen et al. performed a cadaveric study to investigate the blood supply of the FHL [19]. They revealed one avascular zone in which the tendon passed behind the talus and a second, in which the tendon wrapped around the first metatarsal head. Therefore, reduced vascularity behind the talus and the unconscious repetitive overloading of the FHL might contribute to the pathology in our case. By ankle arthroscopy, we removed all fibrous tissues around the FHL, including a fibro-osseous tunnel that compressed the FHL, and achieved a free FHL tendon, gliding with no residual stenosis. The clinical recovery was quick and uneventful until the final follow-up at 6 months after surgery.
Conclusion
We report a rare case of entrapment of the FHL, with no specific causes. Although the actual pathology was unclear, it was plausible that repetitive strain to the FHL might be a predisposing factor in this case. Therefore, orthopedic surgeons should list this situation as a differential diagnosis of posterior ankle pain, even in non-athletes.
Clinical Message
Although stenosing tenosynovitis of the FHL has already been reported in a few cases among athletes, the clinical condition is uncommon. In addition, the case without any specific causes is particularly rare. However, orthopedic surgeons should list this pathology as a differential diagnosis of posterior ankle pain, even in non-athletes.
References
1. Theodore GH, Kolettis GJ, Micheli LJ. Tenosynovitis of the flexor hallucis longus in a long-distance runner. Med Sci Sports Exerc 1996;28:277-9.
2. Cooper ME, Wolin PM. Os trigonum syndrome with flexor hallucis longus tenosynovitis in a professional football referee. Med Sci Sports Exerc 1999;31:S493-6.
3. Moorman CT 3rd, Monto RR, Bassett FH 3rd. So-called trigger ankle due to an aberrant flexor hallucis longus muscle in a tennis player. A case report. J Bone Joint Surg Am 1992;74:294-5.
4. Hamilton WG. Posterior ankle pain in dancers. Clin Sports Med 2008;27:263-77.
5. Tokgoz MA, Kanatli U, Vural A, Ataoglu MB, Yapar A, Ergisi Y. Endoscopic treatment of bilateral hallux saltans in an ordinary woman. Eklem Hastalik Cerrahisi 2019;30:322-4.
6. Adams JE, Habbu R. Tendinopathies of the hand and wrist. J Am Acad Orthop Surg 2015;23:741-50.
7. Martinez-Salazar EL, Vicentini JR, Johnson AH, Torriani M. Hallux saltans due to stenosing tenosynovitis of flexor hallucis longus: Dynamic sonography and arthroscopic findings. Skeletal Radiol 2018;47:747-50.
8. Ozkan K, Goksan B, Ozkan FU, Bilsel K, Bilgic B, Ciftci F. A previously unreported etiology of trigger toe. J Am Podiatr Med Assoc 2006;96:356-8.
9. Lereim P. Trigger toe in classical-ballet dancers. Arch Orthop Trauma Surg 1985;104:325-6.
10. Purushothaman R, Karuppal R, Inassi J, Valsalan R. Hallux saltans due to flexor hallucis longus entrapment at a previously unreported site in an unskilled manual laborer: A case report. J Foot Ankle Surg 2012;51:334-6.
11. Boruta PM, Beauperthuy GD. Partial tear of the flexor hallucis longus at the knot of Henry: Presentation of three cases. Foot Ankle Int 1997;18:243-6.
12. Funasaki H, Hayashi H, Sakamoto K, Tsuruga R, Marumo K. Arthroscopic release of flexor hallucis longus tendon sheath in female ballet dancers: Dynamic pathology, surgical technique, and return to dancing performance. Arthrosc Tech 2015;4:e769-74.
13. Grady JF, Axe TM, Zager EJ, Sheldon LA. A retrospective analysis of 772 patients with hallux limitus. J Am Podiatr Med Assoc 2002;92:102-8.
14. Shurnas PS. Hallux rigidus: Etiology, biomechanics, and nonoperative treatment. Foot Ankle Clin 2009;14:1-8.
15. Chang SH, Matsumoto T, Naito M, Tanaka S. Stenosing tenosynovitis of the flexor hallucis longus tendon associated with the plantar capsular accessory ossicle at the interphalangeal joint of the great toe. Case Rep Orthop 2017;2017:2146762.
16. Hamilton WG. Foot and ankle injuries in dancers. Clin Sports Med 1988;7:143-73.
17. Vallotton J, Echeverri S, Dobbelaere-Nicolas V. Functional hallux limitus or rigidus caused by a tenodesis effect at the retrotalar pulley: Description of the functional stretch test and the simple hoover cord maneuver that releases this tenodesis. J Am Podiatr Med Assoc 2010;100:220-9.
18. Hamilton WG. Differential diagnosis and treatment of posterior ankle pain in dancers and equinus athletes. J Back Musculoskelet Rehabil 1995;5:201-7.
19. Petersen W, Pufe T, Zantop T, Paulsen F. Blood supply of the flexor hallucis longus tendon with regard to dancer’s tendinitis: Injection and immunohistochemical studies of cadaver tendons. Foot Ankle Int 2003;24:591-6.
 |
 |
 |
 |
 |
 |
| Dr. Nobuaki Chinzei | Dr. Noriyuki Kanzaki | Dr. Kanto Nagai | Dr. Masahiko Haneda | Dr. Tetsuya Yamamoto | Dr. Ryosuke Kuroda |
| How to Cite This Article: Chinzei N, Kanzaki N, Nagai K, Haneda M, Yamamoto T, Kuroda R. Posterior Ankle Arthroscopy for Flexor Hallucis Longus Entrapment: A Case Report. Journal of Orthopaedic Case Reports 2021 April;11(4): 70-74. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




