Myopericytoma is an exceedingly rare subgroup of perivascular tumors of unknown etiology which poses special challenge for the surgeons and may be overlooked on differential diagnosis given their potential for mimicry and malignancy.
Dr. Sameer Panchal,
Department of Orthopaedics,
Grant Government Medical College and Sir JJ Group of Hospitals,
Mumbai, Maharashtra, India.
E-mail: panchalsameer1992@gmail.com
Introduction: Myopericytoma (MPC) is an uncommon benign smooth muscle cell neoplasm which frequently arises in lower extremities, sparsely they can be found in upper extremities and head and neck region. Very few case reports are available in the literature documenting hand localization of this tumor.
Case Presentation: In this report, we present a case of 83-year-old male individual with a mass lesion on the proximal phalanx of index finger of the right hand. Recent trivial trauma led the patient to medical assistance. Imaging mimicked Giant cell tumor of tendon sheath due to site of the lesion. The lesion was excised surgically. The final diagnosis of the specimen confirmed by histopathology was MPC, a benign smooth-muscle cell neoplasm.
Conclusion: MPC is a rare entity; however, definitive diagnosis is often challenging because it mimics some malignant soft-tissue neoplasms. A multidisciplinary approach is required to identify this lesion as being benign and thus define the correct modality of treatment.
Keywords: Myopericytoma, proximal phalanx, smooth muscle neoplasm, giant cell tumor.
Myopericytomas (MPCs) are rare, benign perivascular neoplasms that show a hemangiopericytoma-like vascular pattern. It predominantly affects middle-aged patients with no sex predisposition. Few cases have been reported in the literature describing this condition and its imaging characteristics. Pre-operative magnetic resonance imaging and ultrasound are often insufficient or misleading. Excisional biopsy and histopathological confirmation are must for definitive diagnosis. Digital subtraction angiography aids in diagnosis because of the hyper-vascular nature of the tumor and immunohistochemical staining further strengthens the diagnosis of MPC.
A 83-year-old male individual was admitted for evaluation of a mass lesion on the dorsal aspect of the proximal phalanx of index finger of the right hand. The mass had grown insidiously over the past 40 years and initially was not painful. The lesion had become painful after a history of recent trivial trauma. He had no other issues other than pain.
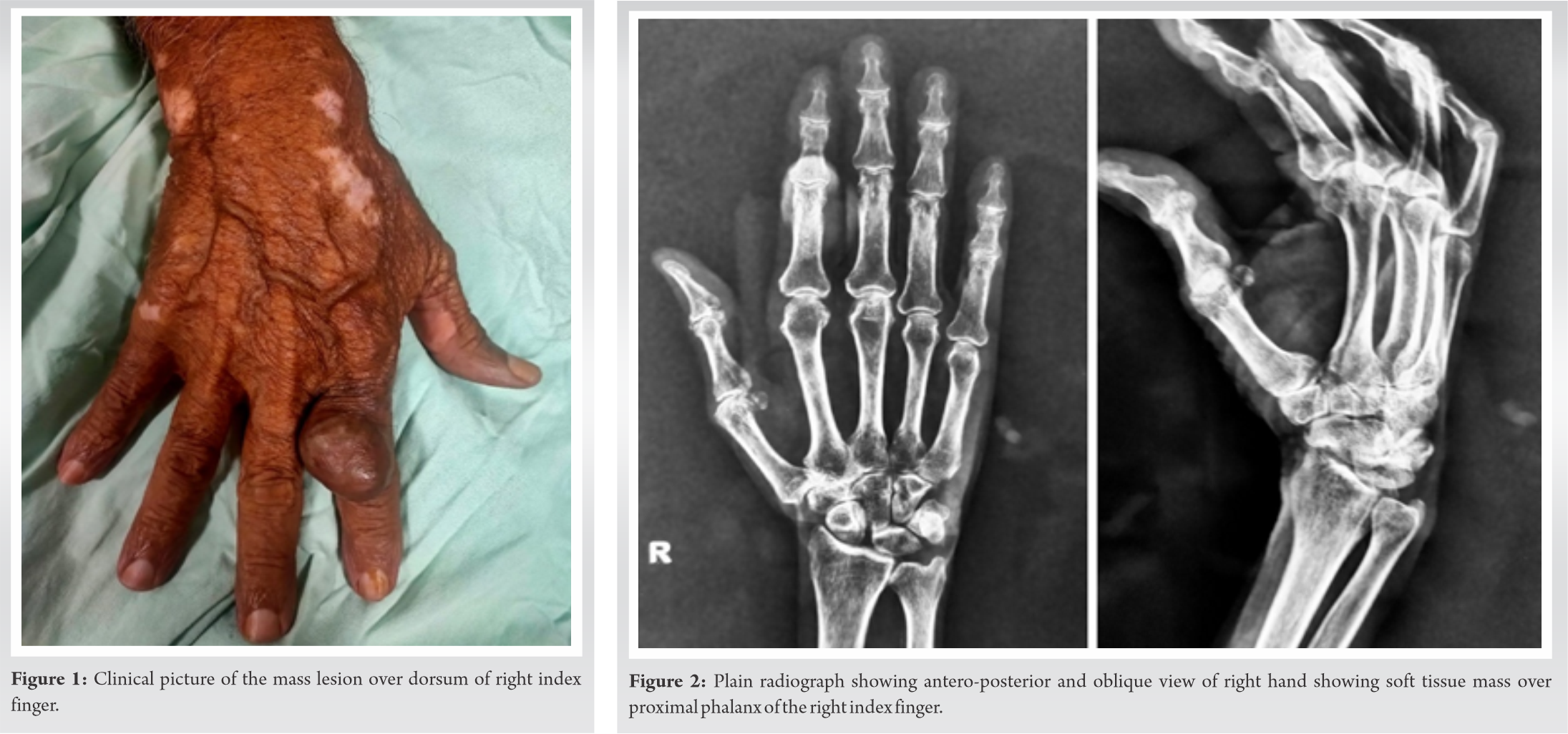
Clinical examination localized the lesion to the dorsal aspect of the proximal phalanx of index finger of right hand (Fig. 1). The mass did not seem fixed to the overlying skin, underlying tendon, or bone. The mass was firm in consistency and not compressible. Some hyperpigmentation was noticed over the swelling. When performing clinical tests, it was noted that normal active and passive movements were possible in the concerned finger. He had normal arterial pulsations in both radial and ulnar arteries. His medical history was unremarkable. Pre-operative blood parameters such as complete blood count, erythrocyte sedimentation rate, and C-reactive protein values were within normal range.
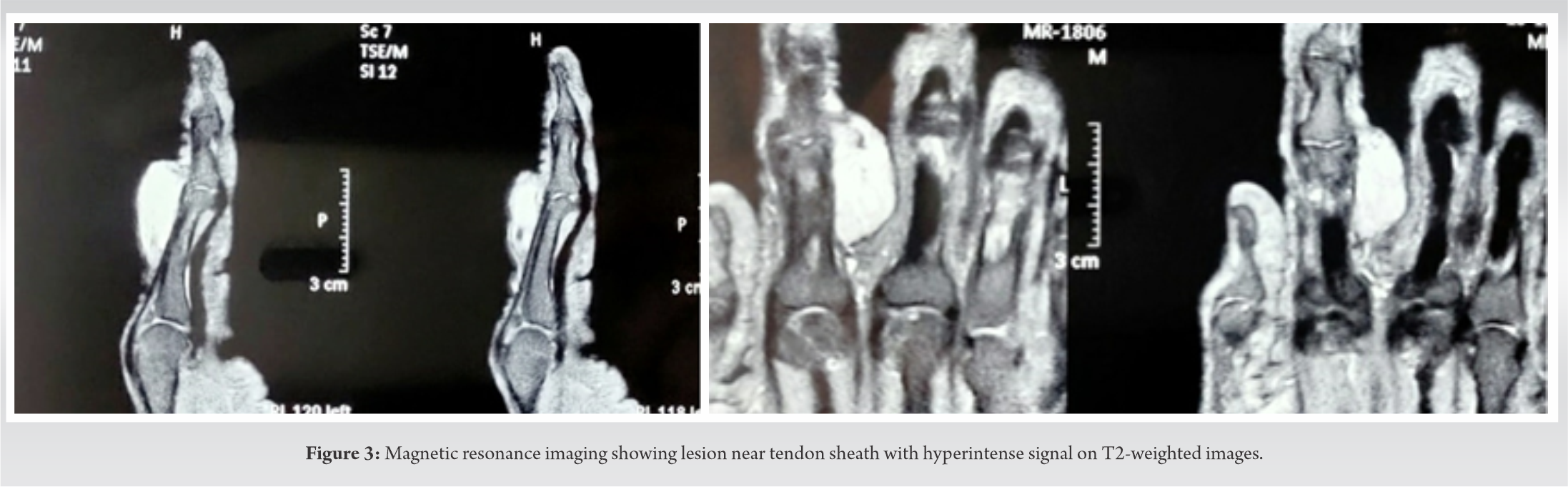
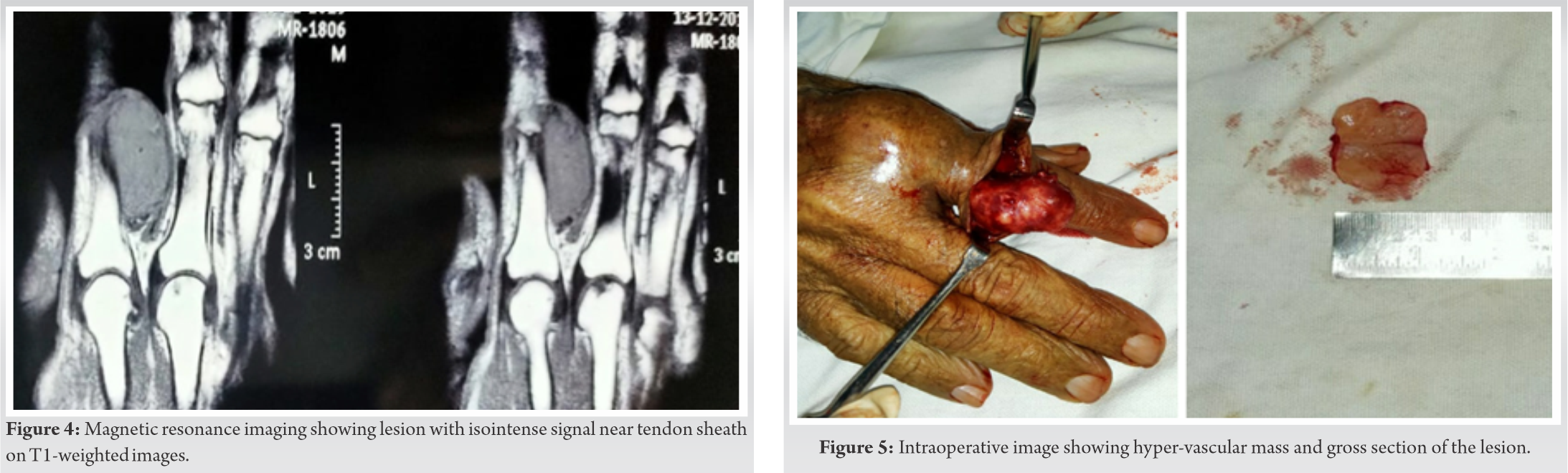
Plain X-ray (Fig. 2) of the right hand was performed and it showed no bony abnormalities apart from soft-tissue shadow at the site of the swelling which was consistent with the clinical evaluation. No calcifications were seen. On magnetic resonance imaging (MRI), the lesion was well-circumscribed and showed no invasion of bone . This lesion was homogeneously hyperintense on the T2-weighted images (Fig. 3). An isointense signal compared with muscle was noted on the T1-weighted images (Fig. 4). The lesion showed no cystic components. No central necrosis was seen. Axial and sagittal T1-weighted images with fat saturation after administration of gadolinium showed avid and homogeneous enhancement. The position of the tumor and its imaging characteristics were consistent with giant cell tumor of tendon sheath. Hence, surgical excision of the lesion was planned.
Surgical excision of the mass was performed under local anesthesia, during the procedure a well encapsulated, hyper-vascular mass was found (Fig. 5). The mass and vascular pedicle could not be differentiated from each other and the tumor was removed en-masse. Histopathology demonstrated a well-defined, encapsulated soft-tissue lesion with abundant vascular structures and MPC-like appearance (Fig. 6). Proliferating spindle cells were found, with clear perivascular, concentric growth. These spindle cells seem to be myopericytes. No nuclear atypia was found and only normal mitotic activity was seen.
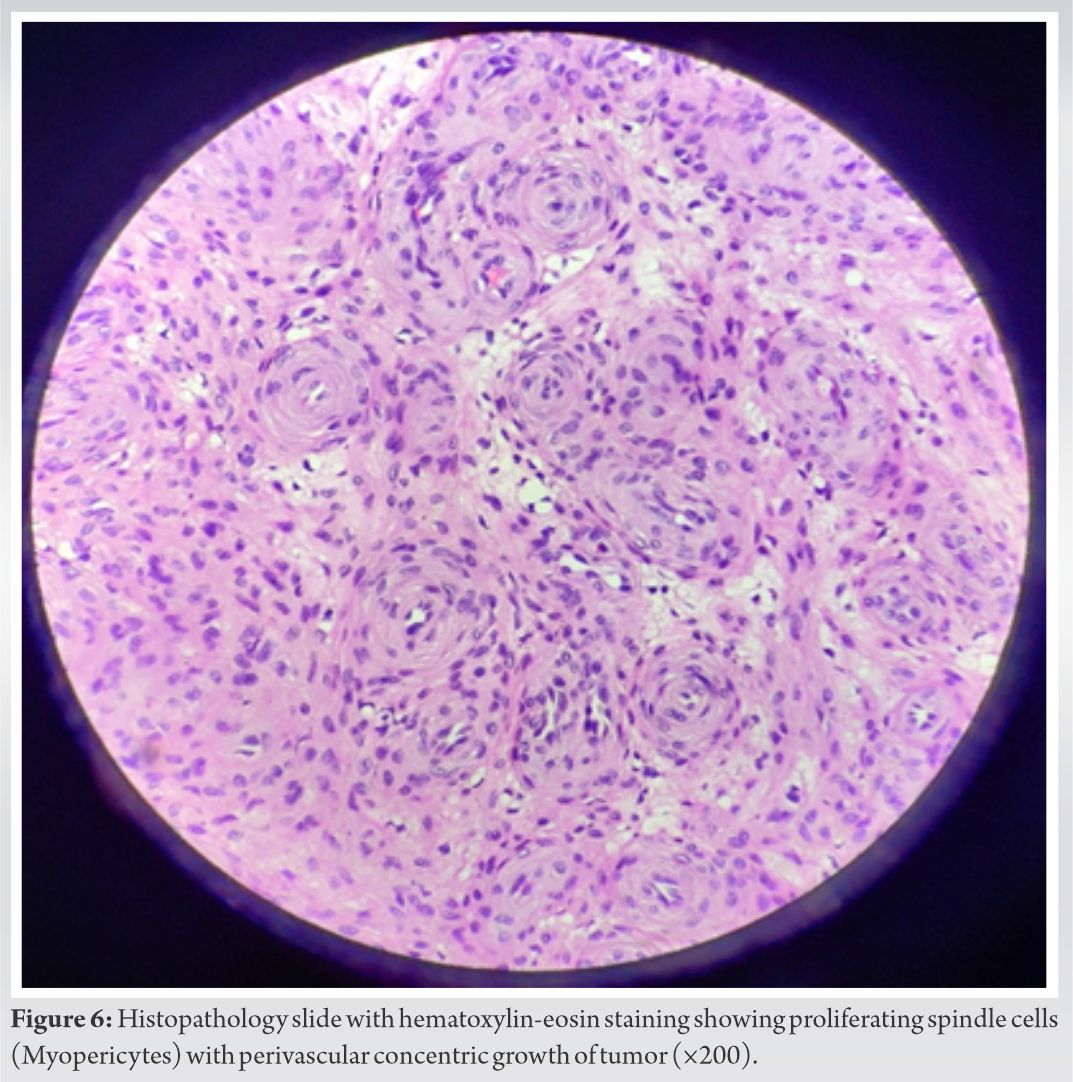
The final histopathological diagnosis was MPC, a rare and benign smooth-muscle cell tumor. Post-operative follow-up for period of 3 years showed normal sensory and motor function and there has been no recurrence. Immunohistochemical testing could not be performed because of financial constraints.
Perivascular neoplasms traditionally consist of glomus tumor and hemangiopericytoma (HPC). Glomus tumor represents a well-defined entity whereas existence of HPC as a separate entity has been questioned because a number of tumors of different lines of differentiation are recognized by HPC-like vascular growth pattern [1]. MPC is a rare benign tumor, recently delineated entity showing HPC-like vascular pattern. A number of lesions named previously HPC actually represent cases of MPC, perivascular tumors showing radial and perivascular arrangement of ovoid, plump spindled to round neoplastic cells with expression of myogenic markers [2, 3]. The term myopericyte was first coined by Dictor et al., describing an unusual case of metastasizing “myofibromatosis like hemangiopericytoma” in a young child, and the authors emphasized that myopericyte represents a transitional form between pericytes and smooth muscle cells of vessels [4]. Myopericytes are ovoid cells with an eosinophilic cytoplasm and typical perivascular growth pattern. Ultra-structurally, these cells have transitioned phenotype and are intermediate cells between pericytes and vascular smooth muscle cells [5]. However, very few reports have been published in the literature about this condition. MPC is a soft-tissue neoplasm originating from myopericytes. They are solitary tumors found in middle aged adults usually localized to the lower extremities [6]. In our case, the lesion was present at proximal phalanx of right index finger which is an uncommon site for this tumor. The lesions exhibit painless, indolent growth, and rarely have malignant characteristics or degeneration. Most of these neoplasms follow a benign course; however, rare cases of malignant MPC have been reported recently [7]. Recurrence is rare. Ultrasound will demonstrate a hypoechoic lesion that is well-defined and can be delineated from the surrounding tissues. The hypervascular nature of the lesion sometimes can be seen on ultrasound. Plain X-ray shows that the absence of bony alterations suggests the benign nature of the mass. The absence of phleboliths helps in differentiating highly vascular lesions. Differentiating this neoplasm from malignant lesions such as sarcoma is difficult with MRI. MPCs are normally isointense to muscle on T1-weighted images and are hyperintense on fat saturated images and T2-weighted images. Enhancement is seen after administration of gadolinium contrast, due to the hypervascular nature of this lesion [8]. Digital subtraction angiography can be performed to depict the vascular nature of the lesion better, to assess the pre-operative vascular status and aid the surgeon in planning [8]. The lesions are usually excised and recurrence is rare. Chemotherapy or radiotherapy has no role. Histopathology is extremely important to identify the lesion as being a MPC (benign lesion) because the extent of surgical resection will be based on these results. Histopathological examination will show a circumscribed soft-tissue tumor with prominent vascular structures; surrounding spindle cells, the myopericytes, create a characteristic tumor appearance [8, 9]. No nuclear atypia will be seen. Immunohistochemistry further strengthens the diagnosis. Alpha-Smooth-muscle actin and h-caldesmon staining are always positive. Desmin is usually negative except few cases [9]. The only drawback of our report was immunohistochemical staining could not be performed because of limited resources and financial constraints. The neoplasm that most closely resembles MPC represents glomus tumor and overlapping morphologic features are frequently present. Immunohistochemical staining are also not of help in differentiating both these entities because tumor cells in glomus tumor stain positively for h-caldesmon, and neoplastic cells in MPC express Type IV collagen as well. However, spindle shaped cells are usually not seen in glomus tumor and glomangioma, which are composed of round uniform tumor cells containing round, well demarcated nuclei [9].
MPC is a benign soft-tissue neoplasm, often difficult to distinguish from other soft tissue lesions just on the basis of clinical and radiographic evidence alone. Hand localization of this tumor as in our case further makes the diagnosis difficult as clinically and radiologically it mimics common tumor such as giant cell tumor of synovial sheath. A multidisciplinary approach helps to guide the evaluation, diagnosis and management.
Myopericytoma is a rare perivascular tumor with predilection for distal extremities that is often difficult to differentiate from other benign or malignant soft tissue neoplasms. A collaborative attitude can precisely lead towards the pathology and surgical excision is the gold standard for diagnosis and treatment.
References
- 1.Granter SR, Badizadegan K, Fletcher CD. Myofibromatosis in adults, glomangiopericytoma, and myopericytoma: A spectrum of tumors showing a perivascular myoid differentiation. Am J Surg Pathol 1998;22:513-25. [Google Scholar]
- 2.Kempson RL, Fletcher CD, Evans HL, Henrickson MR, Sibley RS. Perivascular tumors. In: Rosai J, Sobin LH, editors. Tumors of the Soft Tissues: Atlas of Tumor Pathology. Washington, DC: Armed Forces Institute of Pathology; 2001. p. 371-85. [Google Scholar]
- 3.McMenamin ME. Myopericytoma. In: Fletcher CD, Unni KK, Mertens F, editors. WHO Classification of Tumours: Tumours of Soft Tissue and Bone. Lyon, France: IARC Press; 2002. [Google Scholar]
- 4.Dictor M, Elner A, Andersson T, Fernö M. Myofibromatosis-like hemangiopericytoma metastasizing as differentiated vascular smooth-muscle and myosarcoma: Myopericytes as a subset of myofibroblasts. Am J Surg Pathol 1992;16:1239-47. [Google Scholar]
- 5.Dıaz-Flores L, Gutierrez R, Garcıa MP, Dıaz-Flores L Jr., Valladares F, Madrid JF. Ultrastructure of myopericytoma: A continuum of transitional phenotypes of myopericytes. Ultrastruct Pathol 2012;36:189-94. [Google Scholar]
- 6.Dray MS, McCarthy SW, Palmer AA, Bonar SF, Stalley PD, Marjoniemi V, et al. Myopericytoma: A unifying term for a spectrum of tumours that show overlapping features with myofibroma. A review of 14 cases. J Clin Pathol 2006;59:67-73. [Google Scholar]
- 7.McMenamin ME, Fletcher CDM. Malignant myopericytoma: Expanding the spectrum of tumours with myopericytic differentiation. Histopathology 2002;41:450-60. [Google Scholar]
- 8.van Camp L, Goubau J, van den Berghe I, Mermuys K. Myopericytoma of the base of the finger: Radiological and pathological description of a rare benign entity. J Hand Surg Am 2019;44:69.e1-5. [Google Scholar]
- 9.Mentzel T, Dei Tos AP, Sapi Z, Kutzner H. Myopericytoma, of skin and soft tissues: Clinicopathologic and immunohistochemical study of 54 cases. Am J Surg Pathol 2006;30:104-13. [Google Scholar]









