Adult hip septic arthritis can be treated successfully with ABMS approach for I&D with less muscle damage than other approaches and without special equipment.
Dr. Connor Zale,
Army Medical Center, Honolulu, Hawaii, United States.
E-mail: connor.l.zale.mil@mail.mil
Introduction: Septic arthritis of a native hip is a relatively uncommon condition in adults. Prompt diagnosis and treatment of septic hip arthritis are imperative to preserve joint integrity, as failure to quickly intervene can allow rapid degenerative changes.
Case Report: This is a case report of a 50-year-old male that presented with right septic hip arthritis in the acute setting. He complained of pain with attempted range of motion and log-roll. Laboratory workup demonstrated no leukocytosis, but elevated inflammatory markers. A hip aspiration under fluoroscopy was performed, revealing a cell count of 100,600/cm3 with 91% neutrophils. His right hip underwent irrigation and debridement with a muscle-sparing anterolateral approach (Rottinger).
Conclusion: This case report describes the successful use of the anterior based muscle-sparing approach for incision and drainage of septic arthritis of the native hip joint in an adult patient. Advantages to this strategy include lower rate of nerve injury compared to classical anterior and lateral approaches, less muscle damage than the posterior approach, and no requirement for special skills or equipment as in the case of hip arthroscopy.
Keywords: Septic arthritis, anterior based muscle sparing and anterolateral
Septic arthritis of a native hip is a relatively uncommon condition in adults. Streptococcus aureus is the most common causative organism [1, 2]. Prompt diagnosis and treatment of septic hip arthritis are imperative to preserve joint integrity, as failure to quickly intervene can allow rapid degenerative changes. Several approaches for irrigation and debridement have been described, though each is associated with drawbacks limiting their utility. This is a case report for the novel use of the muscle sparing anterolateral approach for adult septic hip arthritis.
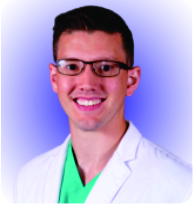
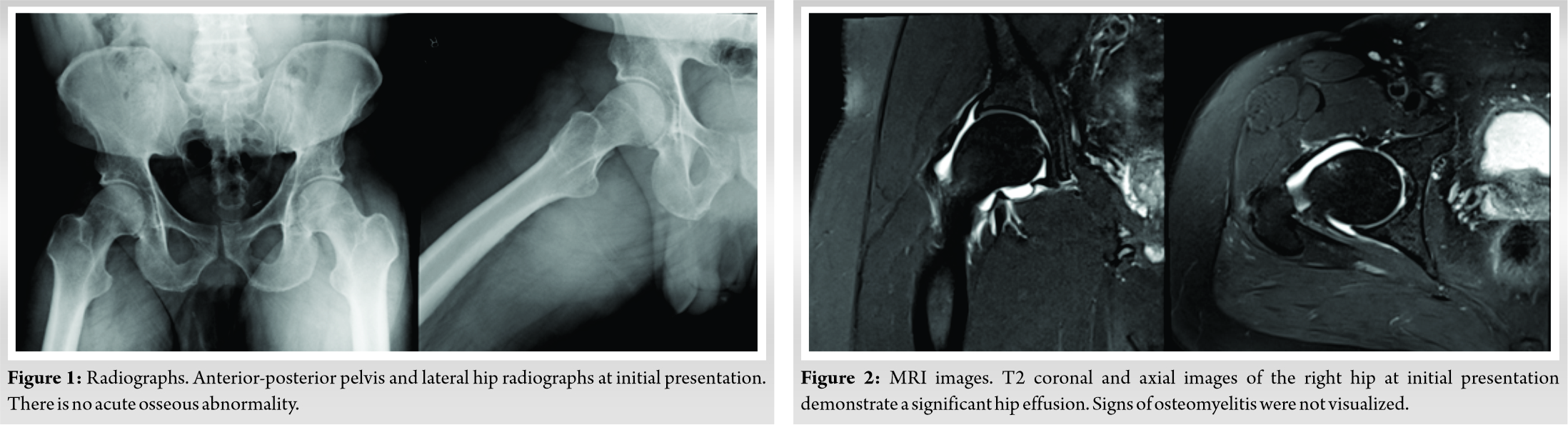
A 50-year-old male presented to the emergency ward with acute right hip pain for 1 day. He was unable to bear weight on his hip, and localized the pain to his right groin. He denied trauma, fevers, chills, numbness, or paresthesia to the right lower extremity. His medical and surgical history was noncontributory. He had no allergies and denied abuse of tobacco, alcohol, or illicit drugs. He was afebrile with stable vital signs at presentation. The right hip was held in a flexed and adducted position. He complained of pain with attempted range of motion (ROM) and log-roll, and he had a normal neurovascular examination. X-rays of the right hip demonstrated no fracture or acute osseous abnormality but MRI revealed a right hip effusion (Fig. 1, 2). Laboratory workup demonstrated no leukocytosis, but elevated inflammatory markers (WBC 7.5 × 10^9/L, ESR 60 mm/h, and CRP 9.04 mg/dL). A hip aspiration under fluoroscopy was performed, revealing a cell count of 100,600/cm3 with 91% neutrophils. There were no crystals on microscopy. PCR was positive for Group B Streptococcus. Both blood cultures and aspiration culture later demonstrated growth of Streptococcus agalactiae.
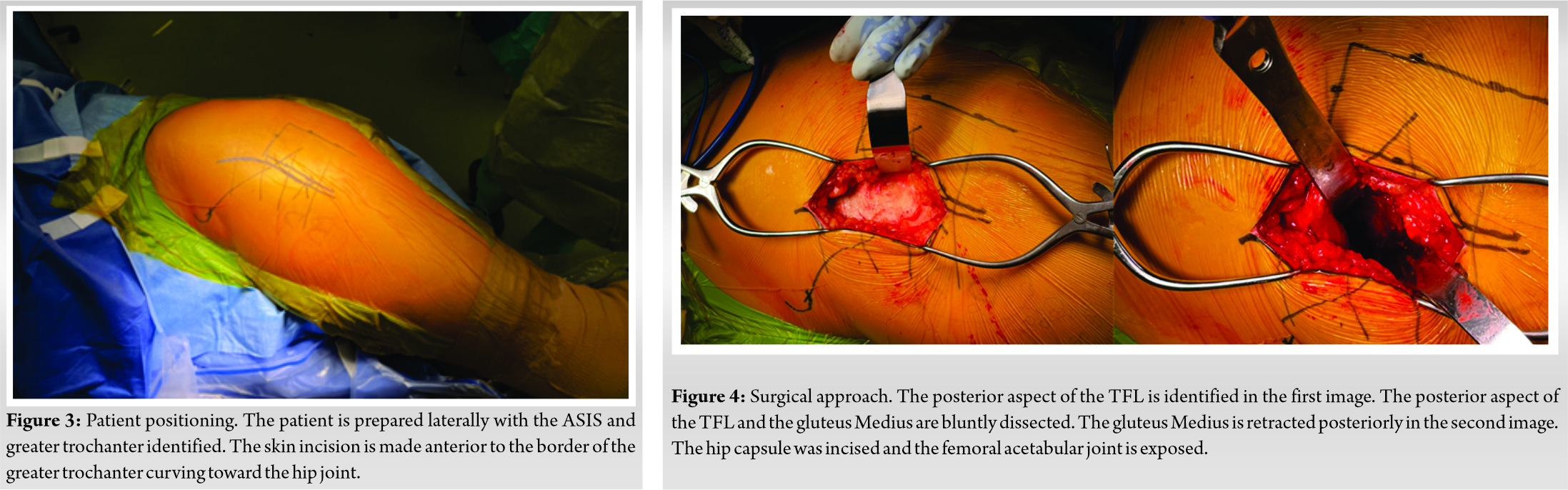
The patient was brought to the operating room for an irrigation and debridement. After administration of anesthesia, he was placed in the left lateral decubitus position (Fig. 3). A muscle-sparing anterolateral approach (Rottinger) was used to gain access to the hip [3]. The fascia was divided, and the plane between the tensor fascia lata (TFL) and gluteus Medius was bluntly developed. The capsule was incised (Fig. 4). Cultures were obtained. Gross purulence was irrigated with 9 L of normal saline. A Hemovac drain was placed and the capsule was left open. The overlying fascia and skin were closed. He was placed on vancomycin and piperacillin-tazobactam as empiric coverage postoperatively. The drain was removed on post-op day 2. He was transitioned oral antibiotics following availability of culture sensitivities for a 4 weeks course, in consultation with an infectious disease specialist. He had pain free ROM of his hip at final follow-up. His gait was symmetric, with equal standing time bilaterally. A radiograph at follow-up was unchanged from his initial examination.
The presentation of adult septic hip arthritis may be unclear at initial presentation. Synovial aspirated WBC is not always diagnostic of septic hip arthritis. Coutlakis et al. found that septic hip arthritis was diagnosed 77% of cases with >100,000 cells and 47% of cases with >50,0000 cells. Septic arthritis is caused by joint inflammation often due to a bacterial cause but can also be fungal, mycobacterial, or viral. S. aureus is the most common cause in adults and children [1]. Strep pneumonia is the second most common cause that was observed by Matthews et al. [2]. Gram negative rods, Group B strep and coagulase negative were the other causes for septic hip arthritis in that same study. Risk factors for repeat irrigation and debridement were found to be inflammatory arthritis, diabetes, synovial cell count >85,000, and staph aureus infection [4]. Group B strep was the etiology for septic hip arthritis in the current case report. The patient denied any preceding illnesses and he denied systemic signs of infection at presentation. He reported not using any illicit drugs and he also had his colonoscopy earlier this year without any masses or lesions. The primary cause of this patient’s septic arthritis is most likely due to hematogenous seeding without an identifiable source. There are several familiar approaches utilized to access the adult hip joint, most commonly for performance of total hip arthroplasty. Although arthroscopy of the hip has proliferated over the last two decades, orthopedic surgeons may lack significant experience in this area. Lack of familiarity with equipment may make emergent and urgent cases challenging for the surgeon, as well as the OR staff. Arthroscopic irrigation and debridement have been found to have comparable outcomes as open irrigation and debridement [4]. Relative advantages of these approaches are outlined in (Table 1). Open surgical approaches to the hip that has been described include anterior (Smith Peterson or Modified Heuter), posterior approach, anterolateral (Watson-Jones), and lateral (Hardinge or Harris) [5]. The anterior approach (Smith-Peterson) does not involve detaching the abductor mechanism. The lateral femoral cutaneous nerve (LFCN) is also at risk with the anterior approach. LFCN injuries are reported for 3.4–81.1% of patients that had an anterior approach [6]. The learning curve with the anterior approach has been documented for arthroplasty literature [7, 8]. The lateral approach can be performed direct lateral (Hardinge) or trans-trochanteric (Harris). The superior gluteal nerve and artery are at risk with these methods. Superior gluteal nerve injuries occur in 2.2–42.5% of patients, resulting in abductor weakness and Trendelenburg gait. Trochanteric nonunion, bursitis, and heterotopic ossification are risks with the trochanteric osteotomy. The posterior approach (Southern) has an increased risk of avascular necrosis (AVN) with damage to the ascending branch of the medial femoral circumflex femoral artery. It requires detachment of the piriformis and short external rotators, necessitating repair. This proves to be a dilemma in the setting of infection, forcing surgeons to decide between leaving these muscles detached, or leaving suture material deep in an infected field. In addition, the fibers of the gluteus maximus are split in the posterior approach, which can complicate rehabilitation. The anterior based muscle-sparing (ABMS) approach, based on the classic anterolateral Watson-Jones interval, avoids many of the problems associated with other open approaches to the hip. Its use of a more posterior interval decreases problems associated with the LFCN seen in the anterior approach. In addition, it avoids violation of the abductor musculature and superior gluteal neurovascular bundle associated with the direct lateral (Hardinge) approach, decreasing the rate of subsequent gait abnormality [3]. There is a lower risk for dislocation due to limited soft tissue disruption. The gluteus medius, gluteus minimus, posterior capsule, and short external rotators are preserved [3]. AVN can be avoided with this approach since the retinacular vessels remain undisturbed with this method. D’Arrigo et al. performed a prospective randomized trial comparing the first 20 arthroplasty cases done by the same surgeon with the modified Hardinge, Rottinger, and direct anterior approaches. The overall complication rate was 10% without any complications with the Rottinger approach [8]. Wohlrab et al. conducted a prospective randomized trial with 20 total hips with the Rottinger approach and 20 hips with the lateral approach [9]. There were improved Harris hip scores at 6 and 12 weeks for the ABMS approach. Another prospective randomized study by Martin et al. found only a significant difference in longer operative time and decreased blood loss using the ABMS compared to the lateral approach with 1 year follow-up [10]. Modifications of the ABMS required for exposure in total joint arthroplasty (extended dissection, more extensive release of the rectus femoris origins, use of a split-leg peg board, and articulating table) are not required for the more limited exposure necessary for incision and drainage (I&D) of the hip joint. The ABMS provides a reliable approach without disruption of the abductor mechanisms that allows for minimal post-operative recovery.
This case report describes the successful use of the ABMS approach for I&D of septic arthritis of the native hip joint in an adult patient. Advantages to this strategy include lower rate of nerve injury compared to classical anterior and lateral approaches, less muscle damage than the posterior approach, and no requirement for special skills or equipment as in the case of hip arthroscopy. The AMBS can be successfully performed by the general orthopedic surgeon, and provides an excellent exposure for this purpose.
Adult hip septic arthritis can be treated successfully with ABMS approach for I&D with less muscle damage than other approaches and without special equipment.
References
- 1.Momodu II, Savaliya V. Septic arthritis. In: Stat Pearls. Treasure Island, FL: Stat Pearls Publishing; 2019. [Google Scholar]
- 2.Matthews PC, Dean BJ, Medagoda K, Gundle R, Atkins BL, Berendt AR, et al. Native hip joint septic arthritis in 20 adults: Delayed presentation beyond three weeks predicts need for excision arthroplasty. J Infect 2008;57:185-90. [Google Scholar]
- 3.Hansen BJ, Hallows RK, Kelley SS. The Rottinger approach for total hip arthroplasty: Technique and review of the literature. Curr Rev Musculoskelet Med 2011;4:132-8. [Google Scholar]
- 4.Lum ZC, Shieh AK, Meehan JP. Native adult hip with bacterial septic arthritis. JBJS Rev 2018;6:e2. [Google Scholar]
- 5.Onyemaechi N, Anyanwu E, Obikili E, Ekezie J. Anatomical basis for surgical approaches to the hip. Ann Med Health Sci Res 2014;4:487-94. [Google Scholar]
- 6.Moretti VM, Post ZD. Surgical approaches for total hip arthroplasty. Indian J Orthop 2017;51:368-76. [Google Scholar]
- 7.Lee SH, Kang SW, Jo S. Perioperative comparison of hip arthroplasty using the direct anterior approach with the posterolateral approach. Hip Pelvis 2017;29:240-6. [Google Scholar]
- 8.D’Arrigo C, Speranza A, Monaco E, Carcangiu A, Ferretti A. Learning curve in tissue sparing total hip replacement: Comparison between different approaches. J Orthop Traumatol 2009;10:47-54. [Google Scholar]
- 9.Wohlrab D, Droege JW, Mendel T, Brehme K, Riedl K, Leuchte S, et al. Minimally invasive vs. transgluteal total hip replacement. A 3-month follow-up of a prospective randomized clinical study. Orthopade 2008;37:1121-6. [Google Scholar]
- 10.Martin R, Clayson PE, Troussel S, Fraser BP, Docquier PL. Anterolateral minimally invasive total hip arthroplasty: A prospective randomized controlled study with a follow-up of 1 year. J Arthroplasty 2011;26:1362-72. [Google Scholar]