In case of pseudomeingocele rupture during brachial plexus surgery, to confirm the fluid is CSF or pleural fluid, beta-2-transferrin levels from fluid is mandatory and consideration of lumbar puncture for drainage of CSF is required depending upon worsening of symptoms post operatively.
Dr. Sanket Tanpure,
DNB Orthopaedic Resident, Jupiter Lifeline Hospital, Mumbai, Maharashtra, India.
E-mail: sankettanpure55@gmail.com
Introduction: Formation of meningocele in brachial plexus injury is known and can be diagnosed on magnetic resonance imaging (MRI). It is mainly reported in brachial plexus root avulsion injuries and does not require specific treatment. We report accurate diagnosis and management of dreadful complication due to rupture of meningocele post-brachial plexus exploration.
Case Report: A 23-year-old engineer presented at 4 months post-bike accident right side extended brachial plexus injury involving C5, C6, and C7. On MRI, he had meningocele in C6-7 root region. We performed supraclavicular exploration of brachial plexus and distal nerve transfers for shoulder abduction and elbow flexion. During surgery, the meningocele was ruptured. As the cyst was deep and extending toward apex of lung, the diagnosis of fluid drained had to be distinguished from pleural fluid with cerebrospinal fluid (CSF). We found hemo-glucose test and beta-2-transferrin levels are mandatory to confirm the diagnosis. Post-surgery, the patient had drainage of almost 500 cc of CSF from wound every day for 3 days. This was managed by repeat MRI and finally lumbar puncture drainage helped to seal the meningocele in neck.
Conclusion: Meningocele in brachial plexus injury is common but rupture of cyst can be fatal. To confirm the origin of fluid, beta-2-transferin level is more specific test than the hemo-glucose test. Lumbar puncture and drainage away from neck can be more reliable modality of treatment in case of intraoperative rupture of such cysts if drainage is excessive postoperatively.
Keywords: Meningocele rupture, cerebrospinal fluid leak, accurate diagnosis, management.
Formation of meningocele in avulsion of roots of brachial plexus is known. Magnetic resonance imaging (MRI) can confirm location of such cysts along with cervical spine injury if present [1]. Patients who have head injury with brachial plexus injury having pseudomeningocele may require primary management for such types of cysts [2]. Injury to meningocele intraoperatively during brachial plexus surgery is not reported so far. We have found meningocele in the neck with ruptured C5, C6 roots. We aim to discuss treatment if it gets injured during surgery.
A case of a 23-year-old male presented with weakness in the right upper limb due to brachial plexus injury involving C5, C6, and C7 roots because of motor bike accident. He was treated for lower end humerus fracture with plating after the same accident. MRI of brachial plexus and CT scan of cervical spine showed meningocele and displaced fracture of spinous and transverse process of C7-D1 on the right side. We planned for exploration of brachial plexus and distal nerve transfers. On supraclavicular exploration of roots of brachial plexus, the meningocele was ruptured and clear fluid drained out (Fig. 1). The cyst was closed with non-absorbable sutures and distal nerve transfers (spinal accessary nerve to suprascapular nerve and ulnar nerve fascicle to biceps branch of musculocutaneous nerve) were performed to complete the surgery. As clear fluid drained through the cyst which was located near spinal roots and apex of lung, it was necessary to distinguish whether it is communicating from lung or cerebrospinal fluid. The hemo-glucose test (HGT) was performed with the fluid to confirm whether it was cerebrospinal fluid (CSF) or pleural fluid. The HGT of CSF is usually <25 mg/dl than blood HGT. As the difference was <10 mg/dl than blood value, the diagnosis of CSF was not confirmed.
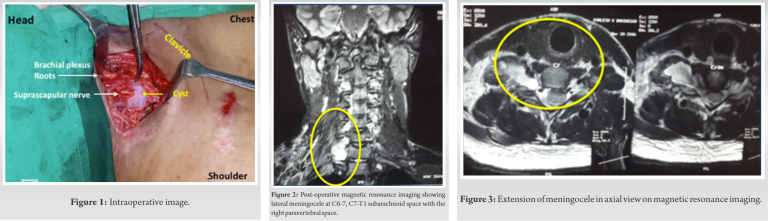
On post-operative day 1, the patient started getting orthostatic headache, nausea, and hypotension and there was more than 500 cc of clear fluid drainage from operative site. Conservative treatment in the form of higher antibiotics, IV fluids was started and head low position was given. MRI of spine and neck was repeated and revealed lateral meningocele at C6-C7 and C7-T1 in subarachnoid space communicating with paravertebral space (Fig. 2, 3). As suggested by neurologist, beta-2-transferrin level was done with the fluid which is more specific test to prove CSF [3]. The test confirmed to be CSF. On post-operative day 2, the drainage was more than 1 L and symptoms of CSF leak worsened. We discussed two options with patient. One was to reexplore the neck and close the cyst again or as per neurosurgeon’s suggestion to consider lumbar puncture to drain the fluid away from its source. Finally, anesthetist did a lumbar puncture and kept an indwelling drain in subarachnoid space L3-L4 level and fluid started draining from there. From post-procedure day 2 of lumbar puncture, the neck drainage started reducing and patient improved symptomatically. Drain was removed after 5 days and the patient was discharged after 1 week.
The patient was successfully treated non-operatively for rupture of lateral meningocele by lumbar puncture. At 10 months post-distal nerve transfers, he got 30° of shoulder abduction and Grade 3+ biceps as per MRC grading. In view of distal humerus fracture, he had 40° of elbow flexion deformity.
In literature, use of coils and embolizing by endovascular technique has been described for pseudomeningocele in root avulsions of brachial plexus [4] agents. Dural cystic lesions are very common findings to give false-positive or false-negative result on computed tomography (CT) myelography or MRI [5]. Therefore, in cases of root avulsions, such lesions are required to be dealt very carefully. Gass et al. had suggested direct laminectomy with suturing of dural tears in 1972 in one of the case reports [6]. Lumbar puncture drainage is used as a treatment of choice in CSF leak while operating large thoracic meningocele successfully by Kim et al. [8]. The neuraminidase activity of brain produces beta-2-transferrin which is a protein variant. So far, it is found only in CSF. Therefore, sensitivity and specificity of detection of beta-2-transferring levels in CSF are very high in comparison with other tests [3]. Glucose detection test for diagnosis of CSF lean is not recommended as bacterial contamination and patients know to have diabetes may provide false readings [8]. Pre-operative analysis of each muscle responsible for diagnosis of root avulsion is very essential and one cannot be relied on CT myelography or MRI findings suggestive of pseudomeningocele [9]. The usual symptoms of post-operative pseudomeningocele leak are postural headache, localized neck pain, and radiculopathy. Early post-operative meningocele ruptures with or without CSF leak can be managed either by CSF drainage by lumbar puncture or percutaneous subarachnoid drainage [10, 11]. This helps in creating a seal and healing of leak site.
Pre-operative MRI is necessary in case of suspicion of root avulsion injury. Meningocele rupture can be fatal. Beta-2-transferin level is more specific test for diagnosing CSF than the HGT. Lumbar puncture and drainage away from neck can be more reliable modality of treatment in case of intraoperative rupture of such cysts. Final result of distal nerve transfer is not affected in such complication and during the management.
Rupture of meningocele during brachial plexus surgery may happen. To confirm the CSF from pleural fluid, beta-transferrin levels and intraoperative HGT have to be done. Repairing of sac with non-absorbable sutures may control the CSF leak but if it does not stop, then epidural drainage must be considered.
References
- 1.Fuzari HK. Diagnostic accuracy of magnetic resonance imaging in post traumatic brachial plexus injuries: A systematic review. Clin Neurol Neurosurg 2018;164:5-10. [Google Scholar]
- 2.Ganaha S. Cervical pseudomeningocele-induced hydrocephalus following traumatic brachial plexus injury. J Spine 2017;6:362. [Google Scholar]
- 3.Oberascher G, Arrer E. Immunologic cerebrospinal fluid diagnosis using beta-2-transferrin principles and methods. Laryngol Rhinol Otol 1986;65:158-61. [Google Scholar]
- 4.Pascual-Gallego M, Zimman H, Gil A, López-Ibor L. Pseudomeningocele after traumatic nerve root avulsion. A novel technique to close the fistula. Interv Neuroradiol 2013;19:496-9. [Google Scholar]
- 5.Carvalho GA, Nikkhah G, Matthies C, Penkert G, Samii M. Diagnosis of root avulsions in traumatic brachial plexus injuries: Value of computerized tomography myelography and magnetic resonance imaging. J Neurosurg 1997;86:69-76. [Google Scholar]
- 6.Gass HH, Devadiga KV, Taptas JN. Epanchement de liquide céphalo-rachidien sus-claviculaire après arrachement du plexus brachial. [Supraclavicular cerebrospinal liquid effusion after brachial plexus avulsion]. Neurochirurgie 1972;18:541-2. [Google Scholar]
- 7.Kim YJ, Cho HM, Yoon CS, Lee CK, Lee TY, Seok JP. Surgical treatment of thoracic meningocele associated with neurofibromatosis and kyphoscoliosis. Korean J Thorac Cardiovasc Surg 2011;44:383-6. [Google Scholar]
- 8.Mantur M, Łukaszewicz-Zając M, Mroczko B, Kułakowska A, Ganslandt O, Kemona H, et al. Cerebrospinal fluid leakage–reliable diagnostic methods. Clin Chim Acta 2011;412:837-40. [Google Scholar]
- 9.Laohaprasitiporn P, Wongtrakul S, Vathana T, Limthongthang R, Songcharoen P. Is pseudomeningocele an absolute sign of root avulsion brachial plexus injury? J Hand Surg Asian Pac 2018;23:360-3. [Google Scholar]
- 10.McCormack BM, Zide BM, Kalfas IH. Spine Surgery, techniques, complication avoidance and management. In: Edward C, Benzel EC, editors. Cerebrospinal Fluid Fistula and Pseudomeningocele after Spine Surgery. Vol. 2. ???: ???; 2005. p. 2033-42. [Google Scholar]
- 11.Pau A. Postoperative “meningocele spurius’. Report of two cases. J Neurosurg Sci 1974;18:150-2. [Google Scholar]








