Heterologous bone is safe as a gap filler in OWHTO, showing good histological integration in vivo after 3 years.
Dr. Giorgio Princi, Department of Trauma and Orthopaedics, Sant’Andrea Hospital, Sapienza University of Rome, Italy. E-mail: giorgioprinci@gmail.com
Introduction:The open-wedge high tibial osteotomy (OWHTO) is a common technique for the treatment of medial compartmental osteoarthritis of the knee. There are many options to fill the osteotomy site gap. The autologous graft donor site morbidity can be avoided using heterologous bone grafts which represent a valid alternative.
Case Presentation:This case report is about a 52-year-old male with knee osteoarthritis and varus deformity. Due to stiffness, swelling, and painful limitation during daily life activities, the patient underwent OWHTO. The osteotomy gap was filled with an equine cancellous bone wedge and nanohydroxyapatite (NHA) bone paste augmentation. After 3 years, the OWTHO was converted to total knee arthroplasty and a bone biopsy of the previous graft site was performed. The histological examination presented non-viable bone areas surrounded by viable bone without inflammatory cells, suggesting the presence of residual non-viable bone from the bone substitute graft.
Conclusion:The in vivo histology of the graft site after 3 years has shown that heterologous bone is a safe and valid choice as a scaffold for bone regeneration. Augmentation with NHA bone paste achieved good osteoinduction without an inflammatory reaction and good integration of the bone substitute insert.
Keywords: High tibial osteotomy, histology, heterograft.
A common and validated technique for painful medial compartmental osteoarthritis of the knee with varus deformity is the open-wedge high tibial osteotomy (OWHTO) [1, 2]. The purpose of OWHTO is to correct the malalignment creating a medial gap, which can be filled with autologous, homologous, heterologous, or synthetic grafts or which can be left empty [3, 4, 5, 6, 7]. The main complication of OWHTO is the limited bone graft integration rate [8]. Autologous bone grafts are a good option due to their osteogenic, osteoinductive, and osteoconductive effects [9, 10]. They also have some disadvantages, such as prolonged surgical time and donor site morbidity [11, 12]. Heterologous bone grafts represent a valid alternative to autologous bone grafts because they do not come with donor site morbidity. However, despite treatment, the potential risk of disease transmission still remains [3, 13]. Therefore, synthetic bone substitutes, such as bioglass, acrylic bone cement, tricalcium phosphate (TCP), and hydroxyapatite (HA), are increasingly used [5, 14, 15]. HA is widely used due to its good biocompatibility and the absence of an inflammatory reaction [16, 17]. Nanomolecular technologies have allowed the development of biocompatible compounds that can be used as bone substitutes, one of which is the nanohydroxyapatite (NHA) [18, 19]. The NHA has osteoconductive properties and accelerates bone growth and remodeling [20, 21, 22]. This is a case of in vivo histological examination of the graft site 3 years after OWHTO with an equine cancellous bone wedge and NHA bone paste augmentation.
Patient information
A 52-year-old Caucasian male presented in our department in March 2015 with a 5-year history of increasing stiffness, swelling, deformity, and range of motion (ROM) limitation of his right knee, with painful limitation during daily life activities. He did not report any previous trauma, knee sprain, or surgery. The patient reported several treatments in the past years (i.e., physical therapy, painkillers, hyaluronic acid injections, and steroid injections), with partial and temporary benefits.
Physical examination revealed varus deformity of the knee, painful ROM limitation, quadriceps muscular atrophy, and diffuse pain at palpation. Radiographic examination showed moderate-severe osteoarthritis of the knee with varus deformity (Fig. 1). Considering the patient’s young age and his request for less invasive surgery than total knee arthroplasty (TKA), an OWHTO was suggested. The patient was thoroughly informed of the risks, benefits, and low long-term success rate.
Therapeutic intervention
A kinematics-based image-free navigation system with HTO software was used. The bone substitute graft was a dehydrated equine cancellous bone wedge (Osteoplant; Bioteck, Italy) and NHA bone paste augmentation (Nanostim Synthetic Bone Paste; Medtronic, Tennessee). The fixation was performed using a Position HTO Plate. Post-operative radiographs showed correction of the varus deformity. The patient was dismissed from hospital 2 days after surgery with a knee brace and non-weight-bearing. The patient followed a standard rehabilitation protocol, the knee brace was kept in full extension for the first 2 weeks and unlocked during the following 2 weeks; at the 4th week, it was removed. After 6 weeks, partial weight-bearing with crutches was initiated. Full weight-bearing was permitted in the 8th post-operative week. No intraoperative or post-operative complications occurred. Finalizing the rehabilitation protocol, the patient reported complete symptoms resolution and returned to daily life activities. We did not report any complications during clinical and radiographic follow-up.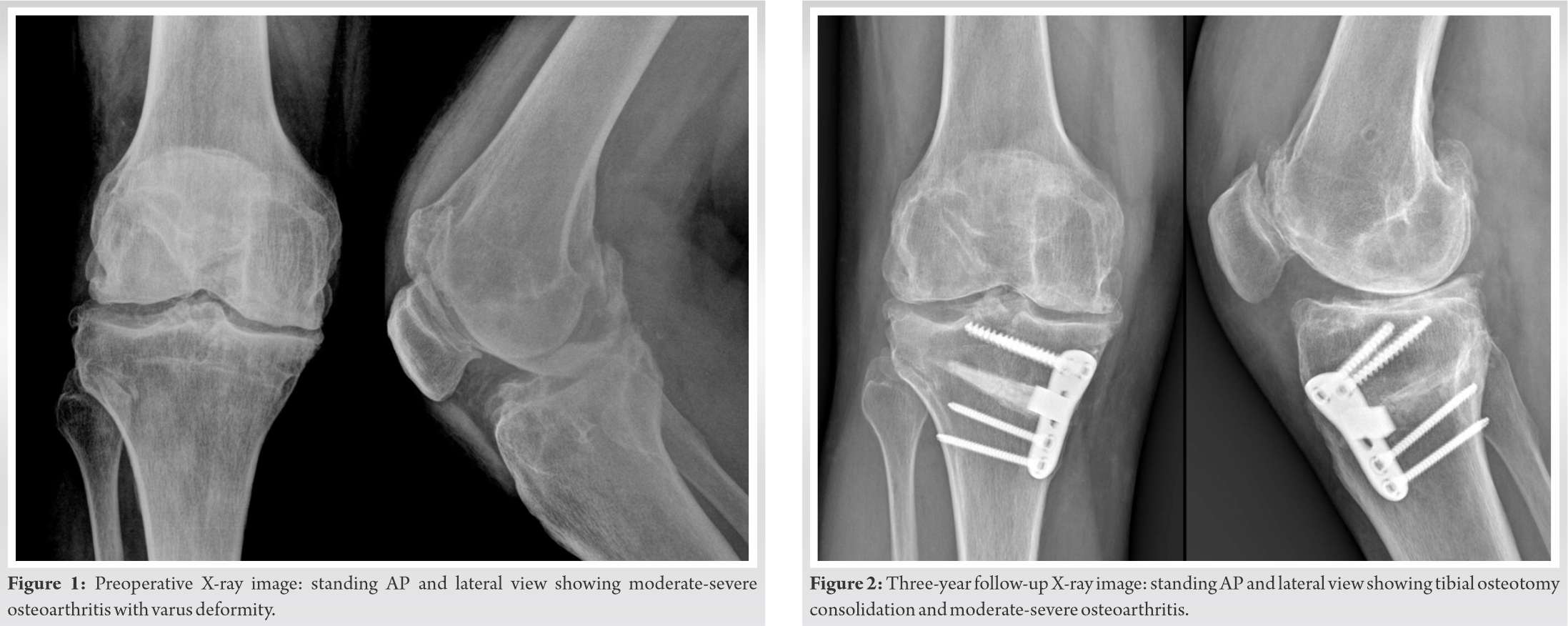
Follow-up and outcomes
At 3-year follow-up, the patient revealed a progressive clinical worsening with stiffness, swelling, and pain that did not respond to medical therapy. Physical examination revealed ROM painful limitation, diffuse pain at palpation, and quadriceps muscular atrophy. Radiographs showed good healing of the osteotomy with moderate-severe osteoarthritis (Fig. 2). Due to the patient’s symptoms, the tibial osteotomy was converted to TKA. During the revision surgery, a bone biopsy of the bone graft site was performed after plate removal. The sample was decalcified using a histological decalcifying agent and cut into 4 µm thick sections using a microtome. The sections were stained with hematoxylin-eosin (HE) and observed at x200, with both polarized light and light microscopy. In Fig. 3 and 4, the same region is shown under light microscopy and under polarized light. Histological findings were as follows: Non-viable bone areas surrounded by viable bone tissue, no inflammatory cells detected around the non-viable bone areas. These findings suggest the presence of residual non-viable bone from the bone substitute graft. Augmentation with NHA bone paste achieved good osteoinduction, the absence of inflammatory infiltrates showed good integration of the bone substitute insert.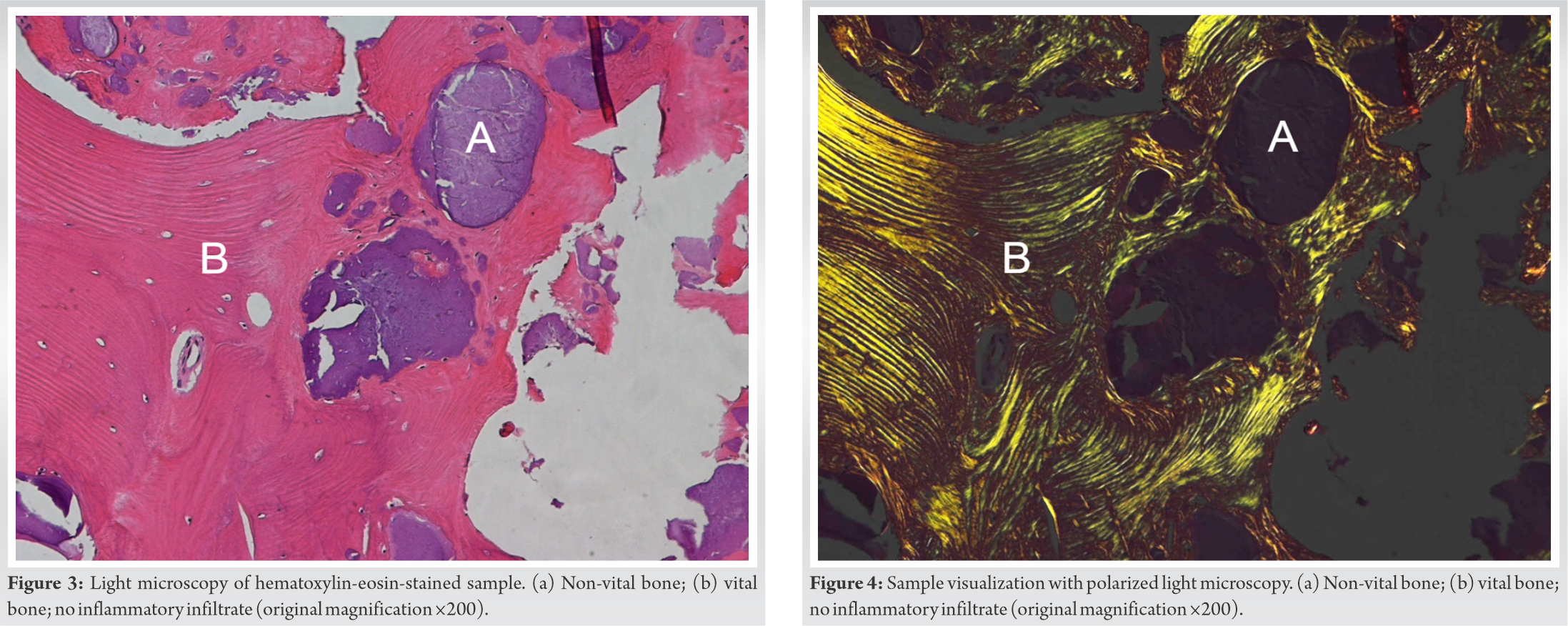
OWHTO has recently become less popular due to the development of TKA, but it still represents a valid choice in relatively young and active patients, thanks to good results in lesions limited to the medial compartment with varus deformity and fewer complications than other techniques [1]. Badawy et al. have recently reported that previous high tibial osteotomy do not impact the revision rate of TKA compared to primary TKA [23]. Historically, Insall et al. reported that 23% of patients who were submitted to OWHTO underwent conversion to TKA [24]. More recently, however, Kim et al., in a meta-analysis, reported 91.6% as the mean 10-year survival rate for OWHTO [25]. Nevertheless, OWHTO also presents complications such as delayed healing and loss of correction [8]. The use of filling grafts has always been the most preferred solution for reducing this complication [3]. Autologous bone graft is still a valid choice; however, iliac crest harvesting entails some risks such as pain, thigh hypoesthesia, infection, and discomfort [11, 12]. For this reason, synthetic bone substitutes, such as bioglass, acrylic bone cement, TCP and HA, are increasingly being used [5, 14, 15]. The histological findings in this case report are consistent with results of the CT study conducted by Conteduca et al. using the same bone substitutes; at 12-month follow-up, better osseointegration of the xenograft was demonstrated when NHA bone paste was added to the graft [26]. Histological comparison between allogeneic bone chips and HA chips as a gap filler in OWHTO made by Lee et al. showed an inferior absorbability of HA chips. However, the author observed mature lamelliform bone in a more significant amount than the HA residues in the radiological unabsorbed area. Clinical and radiological results after OWHTO were similar between the allogeneic bone chips and HA chips [27]. Koshino et al. have radiographically and histologically analyzed bone growth in HA wedges used in OWHTO within 36 months from implantation. Biopsies showed significant bone growth within 300 µm from the interface. However, the radiodensity of the HA wedge did not change during follow-up [16]. Similarly, the use of dehydrated equine cancellous bone wedge and NHA bone paste augmentation did not show absorption areas, and a good osteoinduction was achieved.
There is not any other relevant literature concerning human in vivo histological examination of the bone substitutes used in this case report.
In a histological study of animal samples (rats), Kubasiewicz-Ross et al. analyzed osteoconductive potential and regeneration of bone defects treated with NHA. The histomorphometric analysis showed a greater amount of bone regenerated in the NHA group than in the control group. Furthermore, no particles of the NHA material were found after 8 weeks [28]. In this case, residual graft areas were still present at 3 years without inflammatory reaction. Okazaki et al. analyzed the osteoinductive function of HA in an animal model (rats) with collagen-induced arthritis. The bone formation around the HA block was more significant in the arthritis group than in the control group, suggesting that it might be enhanced even in conditions associated with highly activated bone turnover [29].
In this case, a bone biopsy of the graft site was performed 3 years after the osteotomy, when a revision to TKA was required. Histological examination using optical microscopy with HE-stained specimen presented no inflammatory cells within the sample, suggesting that there were no active remodeling processes. Non-viable bone areas were highlighted, surrounded by viable bone areas, probably due to the residual presence of the graft.
The in vivo histology after 3 years has shown that heterologous bone is a safe and valid choice as a scaffold for bone regeneration. Augmentation with NHA bone paste showed good consolidation, also displaying good osteoinduction and partial replacement of the heterologous bone graft.
References
- 1.Yoo MJ, Shin YE. Open wedge high tibial osteotomy and combined arthroscopic surgery in severe medial osteoarthritis and varus malalignment: Minimum 5-year results. Knee Surg Relat Res 2016;28:270-6. [Google Scholar]
- 2.Ryu SM, Park JW, Na HD, Shon OJ. High tibial osteotomy versus unicompartmental knee arthroplasty for medial compartment arthrosis with kissing lesions in relatively young patients. Knee Surg Relat Res 2018;30:17-22. [Google Scholar]
- 3.Lash NJ, Feller JA, Batty LM, Wasiak J, Richmond AK. Bone grafts and bone substitutes for opening-wedge osteotomies of the knee: A systematic review. Arthroscopy 2015;31:720-30. [Google Scholar]
- 4.Amendola A, Fowler PJ, Litchfield R, Kirkley S, Clatworthy M. Opening wedge high tibial osteotomy using a novel technique: Early results and complications. J Knee Surg 2004;17:164-9. [Google Scholar]
- 5.Koshino T, Murase T, Saito T. Medial opening-wedge high tibial osteotomy with use of porous hydroxyapatite to treat medial compartment osteoarthritis of the knee. J Bone Joint Surg Am 2003;85:78-85. [Google Scholar]
- 6.van Hemert WL, Willems K, Anderson PG, van Heerwaarden RJ, Wymenga AB. Tricalcium phosphate granules or rigid wedge preforms in open wedge high tibial osteotomy: A radiological study with a new evaluation system. Knee 2004;11:451-6. [Google Scholar]
- 7.Zorzi AR, da Silva HG, Muszkat C, Marques LC, Cliquet A Jr., de Miranda JB. Opening-wedge high tibial osteotomy with and without bone graft. Artif Organs 2011;35:301-7. [Google Scholar]
- 8.Martin R, Birmingham TB, Willits K, Litchfield R, Lebel ME, Giffin JR. Adverse event rates and classifications in medial opening wedge high tibial osteotomy. Am J Sports Med 2014;42:1118-26. [Google Scholar]
- 9.Lee OS, Lee KJ, Lee YS. Comparison of bone healing and outcomes between allogenous bone chip and hydroxyapatite chip grafts in open wedge high tibial osteotomy. J Mater Sci Mater Med 2017;28:189. [Google Scholar]
- 10.Slevin O, Ayeni OR, Hinterwimmer S, Tischer T, Feucht MJ, Hirschmann MT. The role of bone void fillers in medial opening wedge high tibial osteotomy: A systematic review. Knee Surg Sports Traumatol Arthrosc 2016;24:3584-98. [Google Scholar]
- 11.Heary RF, Schlenk RP, Sacchieri TA, Barone D, Brotea C. Persistent iliac crest donor site pain: Independent outcome assessment. Neurosurgery 2002;50:510-7. [Google Scholar]
- 12.Ahlmann E, Patzakis M, Roidis N, Shepherd L, Holtom P. Comparison of anterior and posterior iliac crest bone grafts in terms of harvest-site morbidity and functional outcomes. J Bone Joint Surg Am 2002;84:716-20. [Google Scholar]
- 13.Lee SC, Jung KA, Nam CH, Jung SH, Hwang SH. The short-term follow-up results of open wedge high tibial osteotomy with using an Aescula open wedge plate and an allogenic bone graft: The minimum 1-year follow-up results. Clin Orthop Surg 2010;2:47-54. [Google Scholar]
- 14.Hernigou P, Ma W. Open wedge tibial osteotomy with acrylic bone cement as bone substitute. Knee 2001;8:103-10. [Google Scholar]
- 15.Rejda BV, Peelen JG, de Groot K. Tri-calcium phosphate as a bone substitute. J Bioeng 1977;1:93-7. [Google Scholar]
- 16.Koshino T, Murase T, Takagi T, Saito T. New bone formation around porous hydroxyapatite wedge implanted in opening wedge high tibial osteotomy in patients with osteoarthritis. Biomaterials 2001;22:1579-82. [Google Scholar]
- 17.Johnson KD, Frierson KE, Keller TS, Cook C, Scheinberg R, Zerwekh J, et al. Porous ceramics as bone graft substitutes in long bone defects: A biomechanical, histological, and radiographic analysis. J Orthop Res 1996;14:351-69. [Google Scholar]
- 18.Zhu W, Xiao J, Wang D, Liu J, Xiong J, Liu L, et al. Experimental study of nano-HA artificial bone with different pore sizes for repairing the radial defect. Int Orthop 2009;33:567-71. [Google Scholar]
- 19.Zhu W, Wang D, Zhang X, Lu W, Han Y, Ou Y, et al. Experimental study of nano-hydroxyapatite/recombinant human bone morphogenetic protein-2 composite artificial bone. Artif Cells Blood Substit Immobil Biotechnol 2010;38:150-6. [Google Scholar]
- 20.Young AT, Kang JH, Kang DJ, Venkatesan J, Chang HK, Bhatnagar I, et al. Interaction of stem cells with nano hydroxyapatite-fucoidan bionanocomposites for bone tissue regeneration. Int J Biol Macromol 2016;93:1488-91. [Google Scholar]
- 21.Cholas R, Kunjalukkal Padmanabhan S, Gervaso F, Udayan G, Monaco G, Sannino A, et al. Scaffolds for bone regeneration made of hydroxyapatite microspheres in a collagen matrix. Mater Sci Eng C Mater Biol Appl 2016;63:499-505. [Google Scholar]
- 22.Gong T, Xie J, Liao J, Zhang T, Lin S, Lin Y. Nanomaterials and bone regeneration. Bone Res 2015;3:15029. [Google Scholar]
- 23.Badawy M, Fenstad AM, Indrekvam K, Havelin LI, Furnes O. The risk of revision in total knee arthroplasty is not affected by previous high tibial osteotomy. Acta Orthop 2015;86:734-9. [Google Scholar]
- 24.Insall JN, Joseph DM, Msika C. High tibial osteotomy for varus gonarthrosis. A long-term follow-up study. J Bone Joint Surg Am 1984;66:1040-8. [Google Scholar]
- 25.Kim JH, Kim HJ, Lee DH. Survival of opening versus closing wedge high tibial osteotomy: A meta-analysis. Sci Rep 2017;7:7296. [Google Scholar]
- 26.Conteduca F, Di Sette P, Iorio R, Caperna L, Argento G, Mazza D, et al. Nanohydroxyapatite promotes the healing process in open-wedge high tibial osteotomy: A CT study. Knee 2016;23:763-9. [Google Scholar]
- 27.Lee SS, So SY, Jung EY, Seo M, Lee BH, Shin H, et al. The efficacy of porous hydroxyapatite chips as gap filling in open-wedge high tibial osteotomy in terms of clinical, radiological, and histological criteria. Knee 2020;27:436‐43. [Google Scholar]
- 28.Kubasiewicz-Ross P, Hadzik J, Seeliger J, Kozak K, Jurczyszyn K, Gerber H, et al. New nano-hydroxyapatite in bone defect regeneration: A histological study in rats. Ann Anat 2017;213:83-90. [Google Scholar]
- 29.Okazaki A, Koshino T, Saito T, Takagi T. Osseous tissue reaction around hydroxyapatite block implanted into proximal metaphysis of tibia of rat with collagen-induced arthritis. Biomaterials 2000;21:483-7. [Google Scholar]











