A thorough history and clinical examination are needed for early diagnosis of ohronotic arthropathy and the surgeon should be cautious about the potential complications such as difficult spinal anaesthesia, chance of patellar tendon rupture during total knee replacement and during early rehabilitation period.
Dr. Syam G, Department of Orthopedics, Lourdes Hospital, Kochi, Kerala, India. E-mail: syamgangan@gmail.com
Introduction:Alkaptonuria is a rare autosomal recessive metabolic disorder characterized by accumulation of homogentisic acid (HGA) due to an inherited deficiency of the enzyme HGA oxidase. Unlike rheumatoid arthritis which affects the small joints of the hands and feet, ochronotic arthropathy predominantly involves the large weight-bearing joints such as hips, knees, and spine. The knee is the most common joint to be affected. Ochronotic arthropathy is usually managed conservatively, but for severely affected hip and knee joints, replacement is considered.
Case Report:This report describes a case of 57-year-old male who presented with bilateral knee osteoarthritis who was incidentally diagnosed with ochronosis intraoperatively during total knee arthroplasty, its challenges faced and post-operative functional outcome after 18 months follow-up.
Conclusion:This case report highlights the need for high index of suspicion for preoperative diagnosis of ochronotic arthropathy. Difficult spinal anesthesia should be anticipated. Friable and stiff tendon due to ochronotic involvement can put the extensor tendon at risk of rupture during retraction of patella intraoperatively. Post-operative active quadriceps rehabilitation should be done with caution due to friable tendon.
Keywords:Alkaptonuria, ochronosis, ochronotic arthropathy, autosomal recessive, total knee arthroplasty.
Alkaptonuria is an autosomal recessive disorder of phenylalanine and tyrosine metabolism caused by the deficiency of homogentisate 1,2 dioxygenase activity. It is caused by a mutation in the HGD gene for the enzyme homogentisate 1,2-dioxygenase. This condition is rare, affecting 1 in 250,000 to 1 million people World Wide. Alkaptonuria is more common in certain areas of Slovakia (where it has an incidence of about 1 in 19,000 people) and in the Dominican Republic [1]. The deficiency of enzymes results in the accumulation of melanin-like pigmented phenols such as homogentisic acid (HGA) and hydroquinone in the connective tissues primarily the cartilaginous joint surfaces, ribs, intervertebral disks, ear cartilage, etc.; the latter is termed ochronosis [2]. The term ochronosis is derived from the word “ochre” in the Greek language, which refers to yellow discoloration [3]. Patients are usually asymptomatic as children or young adults, whose only symptoms being brownish discoloration of urine if left exposed to air for some time [1].
A 57-year-old male patient presented with bilateral knee pain of 7 years duration, which was more on the right knee. Pain was gradually progressing over years which was aggravated on exertion and relieved on rest and pain medication during the initial years. At the time of presentation, the pain was affecting his day-to-day activities and not responding to conservative management. No cutaneous signs of ochronosis were noticed at the time of presentation. Patient had a history of darkening of urine and staining of clothes which was revealed by patient only after surgery when asked. The same history is present in patients father and his son. Patient had previous history of spontaneous rupture of Achilles tendon on both sides while climbing down the stairs 5 years apart which was treated surgically elsewhere. Patient also has a history of triggering of the index finger and thumb for which surgery was advised by some orthopedecian but was refused by the patient.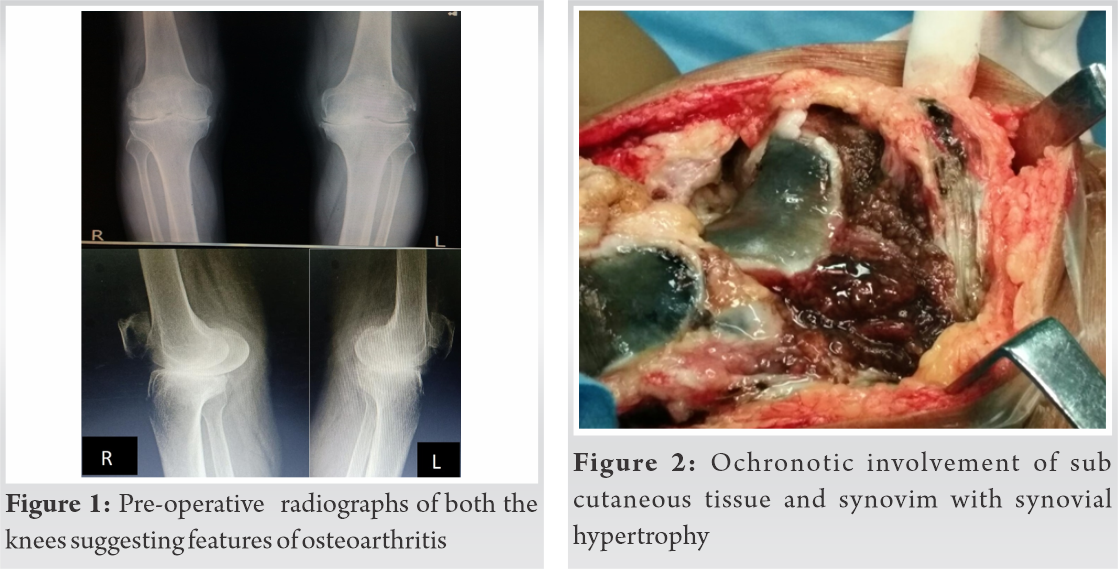
On physical examination, he had a stable gait with antalgic component. There was neutral alignment of both the knees. There was no swelling or effusion. On deep palpation, there was medial and lateral joint line tenderness. The range of motion of the right knee was 0°–100° and left knee was 0°–85° and was painful. Anteroposterior and lateral standing radiographs were taken which demonstrated concentric joint spaces narrowing, peripheral new bone formation, subchondral bone sclerosis, and arthritic changes of the patella (Fig. 1).
Rheumatology consultation was done to rule out inflammatory etiology but the routine inflammatory markers were negative. Cemented total knee replacement of left knee was done initially since it was more symptomatic, followed by the right knee after 1 month interval.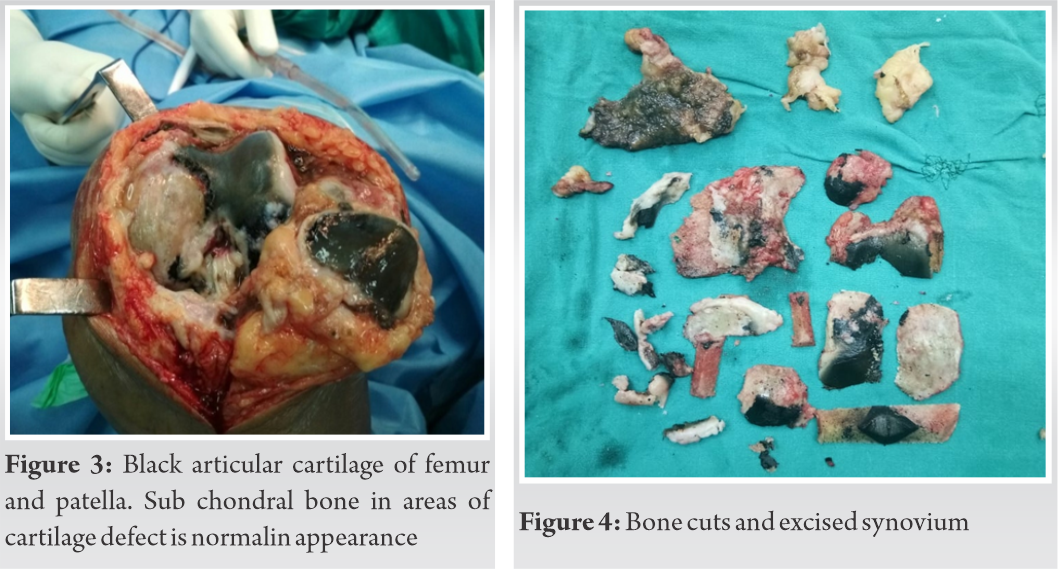
During the first surgery, spinal anesthesia was obtained with great difficulty, and second surgery was done under general anesthesia due to failed attempt for spinal anesthesia. Intraoperatively, anterior midline incision with medial para-pattelar approach was used. As the incision was deepened blackish staining of subcutaneous tissue was noted. There was marked synovial hypertrophy. The joint capsule was contracted and partially black with a hard consistency (Fig. 2). The patellar tendon had black discoloration and was difficult to retract and while retracting a popping sound was heard but no obvious extensor mechanism disruption was noted. The quadriceps tendon, articular cartilage of femur, tibia, and patella were blackened with patchy area of normal subchondral bone over the medial femoral condyle where articular cartilage was deficient (Fig. 3). Both the menisci were also blackened and were very stiff. While taking bone cuts black discoloration was seen up to the thickness of cartilage only and subchondral bone was of normal appearance but soft inconsistency (Fig. 4). Standard cementing technique was performed without difficulty (Fig. 5, 6).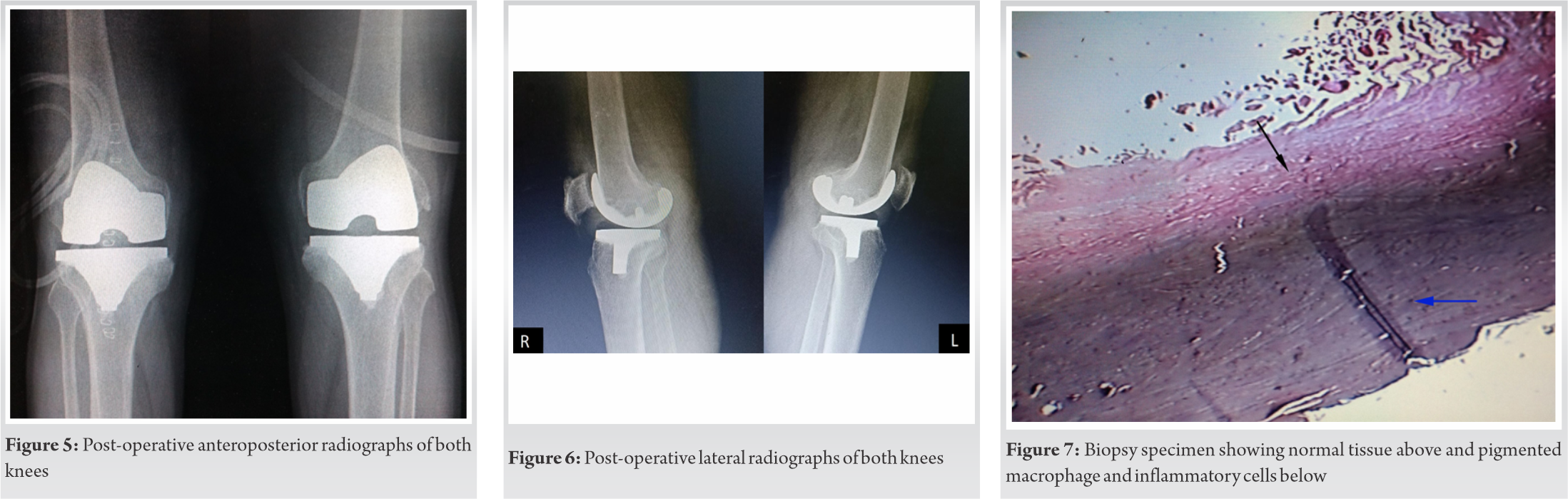
Biopsy of the resected specimen was proved to be Ochronosis (Fig. 7). Preoperatively spinal anesthesia was given with great difficulty as the anesthetist was not able to palpate the interspinous space. No major complications were experienced during the surgery. Knee was mobilized on the first post-operative day. Post-operatively active quadriceps rehabilitation was started the next day itself but with extreme caution due to the stiff and friable tendon. The drain was removed on the 2nd postoperative day. Patient had mild postoperative pain. Post-operative wound healing was uneventful. Patient had improved and painless range of movement (0–110) of both knees. Post-operatively on examination patient had hyperpigmentation in the cornea and thenar and hpothenar eminence which was missed during pre-operative clinical examination (Fig. 8, 9). The knee society score was 84 on the past follow-up 18 months post-operatively.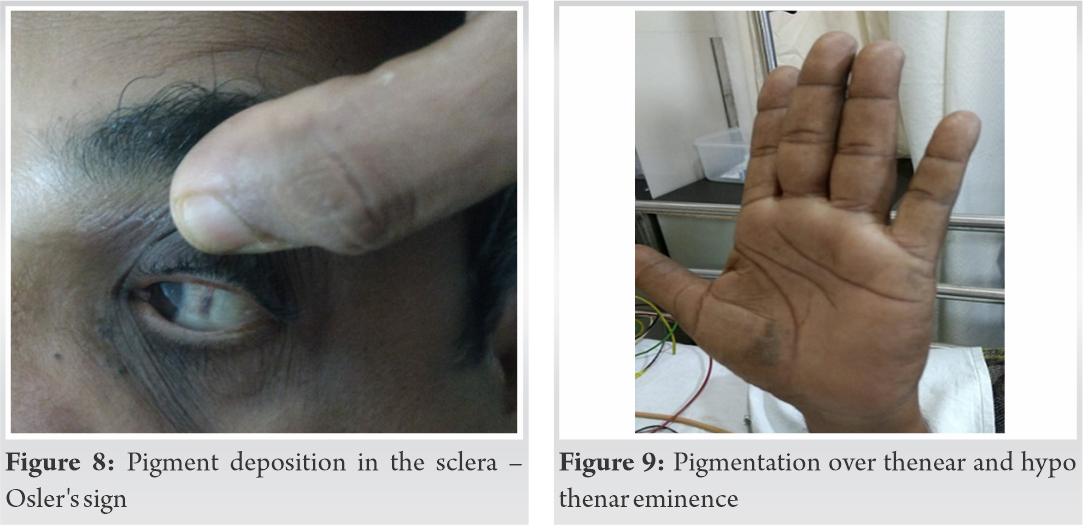
Alkaptonuria, is a rare autosomal recessive metabolic disorder characterized by accumulation of HGA due to an inherited deficiency of the enzyme HGA oxidase. The clinical symptoms usually appear by the third or fourth decade since the renal clearance of homogentesic acid decreases with aging. Males are more symptomatic than females [4].
In the urine, homogentesic acid is oxidized to benzoquinone acetate (BQA). Urine is normal in color when freshly passed, but on exposure to air BQA is rapidly oxidized which darkens urine to assume brownish-black color [4]. Other clinical signs include pigmentation affecting the cartilage of the ear as well as other cartilage, and the sclera and corneal limbus of the eye [5]. In skin, even though the pigment is deposited throughout, it usually becomes apparent only in certain locations where connective tissue is thick (joints, tympanic membrane) or close to the surface of the skin (thenar and hypothenar eminences and the sides of the fingers. In the eye, the most obvious change is brownish black pigmentation around the palpebral fissure. Hoarseness of voice can occur due to pigmentation and hardening of laryngeal cartilage. There is an increased chance for intervertebral disc prolapse. Stenosis of heart valves can results from the increased rigidity of the connective tissue as well as chronic inflammation. Ligaments and tendons are stiffened due to pigment deposition and are prone for rupture.
Arthropathy is common due to pigment deposition, chronic inflammation, and microruptures. The knee is the most common site of orthopedic abnormality. Other sites of involvement are the hips, shoulders, sacroiliac joints, and the pubic symphysis [6]. There is no definitive cure for the disease but Nitisinone, an inhibitor of 4-hydroxyphenyl pyruvate dioxygenase has been shown to decrease urinary excretion of homogentisic acid. The effectiveness of Nitisinone in treating ochronotic arthropathy is unknown [7]. Premature degenerative arthritis affecting large joints is common in these of patients. Early stages of ochronotic arthropathy are managed conservatively, but for severely affected hip and knee joints, only replacement can improve the quality of life [8]. Since most of the time the affected bone may be of poor quality, the success and longevity of replacement arthroplasty can be a concern [9] but many literature reports good results for joint arthroplasty, similar to osteoarthritis patients without ochronosis. Jonathan Spencer et al. in 2009 published 6–12 year follow-up of 11 replacements in three ochronotic arthritis patients and found no prosthetic failures in 12 year follow-up period [9]. Aydoğdu et al. reported 4 years follow-up of cementless Total knee replacement and found no bone ingrowth deficits that might be detrimental for the stabilization of cementless prostheses in ochronotic arthropathy because the bone tissue is not primarily affected by the disease. The 4-year follow-up was satisfactory without any evidence of loosening [8].
Ochronotic arthropathy is an unusual type of arthritis occurring in patients with alkaptonuria. Because of the rarity of the disease and paucity of clinical symptoms until middle age, the diagnosis of alkaptonuria is delayed and is occasionally discovered intraoperatively [10]. In the present case also the diagnosis of ochronosis was not made until during surgery which was confirmed by biopsy. So high index of suspicion is required for preoperative diagnosis. Difficult spinal anesthesia should be anticipated. Friable and stiff tendon due to ochronotic involvement can put the extensor at risk of rupture during retraction of the patella. We need more such case reports to prove real incidence of such involvement. As there is a lack of data suggesting choice between cemented or non-cemented prosthesis, we proceeded with cemented total knee replacement as a part of routine procedure.
High index of suspicion is needed for the diagnosis of ohronosis particularly in relatively young patients presenting with arthritis of large joints. A thorough history and screening of family members are needed for early diagnosis of the disease. General anesthesia may be preferred due to the involvement of the intervertebral disk. Tendon can be friable and stiff and hence care should be needed while everting the patellar tendon to avoid rupture and during post-operative rehabilitation.
References
- 1.Ranganath L, Taylor AM, Shenkin A, Fraser WD, Jarvis J, Gallagher JA, et al. Identification of alkaptonuria in the general population: A United Kingdom experience describing the challenges, possible solutions and persistent barriers. J Inherit Metab Dis 2011;34:723-30. [Google Scholar]
- 2.La JD. Alcaptonuria and ochronotic arthritis. Mol Biol Med 1991;8:31-8. [Google Scholar]
- 3.Bhattar PA, Zawar VP, Godse KV, Patil SP, Nadkarni NJ, Gautam MM. Exogenous ochronosis. Indian J Dermatol 2015;60:537. [Google Scholar]
- 4.Fisher AA, Davis MW. Alkaptonuric ochronosis with aortic valve and joint replacements and femoral fracture: A case report and literature review. Clin Med Res 2004;2:209-15. [Google Scholar]
- 5.Koska L, Srsen S. A simple urine screening test for alcaptonuria. N Engl J Med 1977;297:1471-2. [Google Scholar]
- 6.Findlay GH. Ochronosis. Clin Dermatol 1989;7:28-35. [Google Scholar]
- 7.Patel VG. Total knee arthroplasty in ochronosis. Arthroplast Today 2015;1:77-80. [Google Scholar]
- 8.Aydogdu S, Cullu E, Ozsoy MH, Sur H. Cementless total knee arthroplasty in ochronotic arthropathy: A case report with a 4-year follow-up. J Arthroplast 2000;15:539-43. [Google Scholar]
- 9.Spencer J, Gibbons CM, Sharp R, Carr A, Athanasou N. Arthroplasty for ochronotic arthritis No failure of 11 replacements in 3 patients followed 6-12 years. Acta Orthop Scand 2004;75:355-8. [Google Scholar]
- 10.Gil JA, Wawrzynski J, Waryasz GR. Orthopedic manifestations of ochronosis: Pathophysiology, presentation, diagnosis, and management. Am J Med 2016;129:536-e1. [Google Scholar]











