Any atypical lesion of the foot should be subjected to biopsy and a confirmatory result before initiating any therapy.
Dr. Kamalakar Rao Rachakonda, Department of Orthopaedics, Sunshine Multispeciality Hospital, Secunderabad - 500 003, Telangana, India. E-mail: kamalakarrao4878@gmail.com
Introduction:Osteoblastoma is a rare benign bone-forming tumor but causes considerable morbidity if left untreated. Among them, osteoblastoma of cuboid is very rarely seen and hence poses considerable diagnostic and therapeutic challenges especially when it mimics features of tuberculosis of foot.
Case Report:This case report describes a rare case of cuboid osteoblastoma of the right foot in a 24-year-old female who was initially treated as TB foot elsewhere and presented to our outpatient department with non-resolving pain affecting her daily activities. She was found to have osteoblastoma of cuboid bone along with medial arch collapse and instability of mid foot. She underwent en bloc excision of the cuboid bone with lateral and medial column stabilization procedures. She made an uneventful recovery and reported no recurrence after a follow-up of 2 years.
Conclusion: Cuboid osteoblastoma can present atypically with mid foot collapse and arthritis leading to an erroneous diagnosis of TB due to the concomitant inflammation. Hence, any atypical lesion of the foot should be subjected to biopsy and a confirmatory result before initiating any therapy.
Keywords:Cuboid osteoblastoma, Tuberculosis foot, Medial arch collapse
Osteoblastoma is a rare benign bone tumor similar to osteoid osteoma commonly detected in second and third decades of life. The most common sites of involvement are spine and long tubular bones [1]. These tumors are typically larger than 1.5–2 cm in size and account for approximately 1% of all benign bone tumors [2]. These lesions appear similar to osteoid osteoma except that they are larger in size, more aggressive in nature; do not have pain that is severe in night or relieved by non-steroidal anti-inflammatory drugs [3]. The tumor is highly vascular in nature and appears red to red-brown in color with a gritty appearance macroscopically due to the presence of woven bone [4]. This tumor rarely affects bones of the foot and there is only one case report published in the literature describing the presentation and the management of this tumor in cuboid bone [5]. This case report describes the challenges involved in diagnosis and surgical management of a case of osteoblastoma of cuboid bone, which masqueraded as tuberculosis (TB) on presentation.
A 24-year-old female presented to the outpatient department with complaints of progressively increasing pain and swelling in her left foot since past 3 years. There was no history of antecedent trauma or fever. She visited multiple orthopedic surgeons who managed her conservatively with foot-wear modification, analgesics initially. However, she did not improve and she was finally started on trial anti-tubercular treatment (ATT) after a presumptive diagnosis of TB was made based on magnetic resonance imaging of the foot, reported hyper-intensity on short-tau inversion-recovery sequences in cuboid bone and in the soft tissue on dorsal and plantar aspect of foot (Fig. 1). However, the patient reported no relief of symptoms and noted an increase in swelling of the foot. On examination, the foot was diffusely swollen with the forefoot in eversion and loss of medial arch (Fig. 2a).
There was tenderness in the mid-foot region and along the medial border of the foot but no local rise of temperature was noted. There was significant wasting of the calf muscle but demonstrated normal ankle range of motion (ROM) and her mid-foot AOFAS score was documented to be 24. An X-ray of foot showed diffuse osteopenia with early arthritic changes in the mid-foot (Fig. 2b). A computed tomography scan of foot was performed which reported an expansile osteolytic lesion, eccentrically located in infero-medial aspect of cuboid (Fig. 3). She demonstrated normal blood cell counts, alkaline phosphatase, and acute phase reactants (erythrocyte sedimentation rate and C-reactive protein). Her liver and kidney function tests were normal. Based on the prior history of non-responsiveness to ATT, a core biopsy from the Cuboid bone was taken and the sample sent for histopathology and gene expert test for TB. The histopathology sample showed features suggestive of osteoblastoma and gene expert test reported negative for TB. After a second review in the institute tumor board meeting, a surgical plan of en bloc excision of the Cuboid bone followed by lateral column fusion was planned. Under regional anesthesia and tourniquet control, longitudinal incision was made on the lateral aspect of the dorsum of foot in line with the fourth metatarsal extending from the sinus tarsi to the middle third of the fourth metatarsal. Cuboid bone was removed en-bloc after dissecting from the surrounding soft tissue (Fig. 4).
A computed tomography scan of foot was performed which reported an expansile osteolytic lesion, eccentrically located in infero-medial aspect of cuboid (Fig. 3). She demonstrated normal blood cell counts, alkaline phosphatase, and acute phase reactants (erythrocyte sedimentation rate and C-reactive protein). Her liver and kidney function tests were normal. Based on the prior history of non-responsiveness to ATT, a core biopsy from the Cuboid bone was taken and the sample sent for histopathology and gene expert test for TB. The histopathology sample showed features suggestive of osteoblastoma and gene expert test reported negative for TB. After a second review in the institute tumor board meeting, a surgical plan of en bloc excision of the Cuboid bone followed by lateral column fusion was planned. Under regional anesthesia and tourniquet control, longitudinal incision was made on the lateral aspect of the dorsum of foot in line with the fourth metatarsal extending from the sinus tarsi to the middle third of the fourth metatarsal. Cuboid bone was removed en-bloc after dissecting from the surrounding soft tissue (Fig. 4).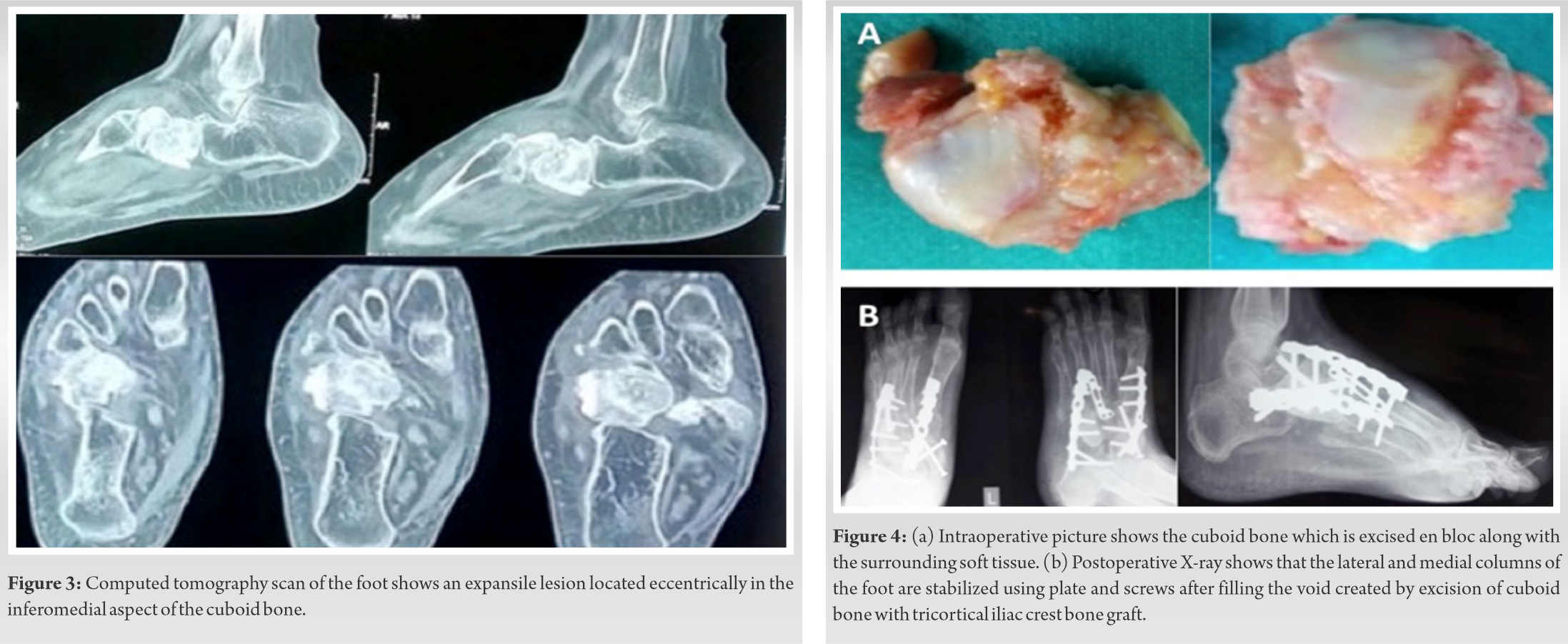 The lateral column was stabilized by filling the void created by removal of Cuboid bone with tricortical iliac crest bone graft and fixed with a 3.5 mm locking reconstruction plate extending from the calcaneum to the fourth metatarsal. Intraoperatively medial column instability was observed and confirmed under fluoroscopy and hence a decision to stabilize the column was made (Fig. 4). A longitudinal incision was made over the dorsum of the foot in the interval between the first and second ray and neurovascular bundle isolated. The medial column was stabilized using a spanning reconstruction locking plate extending from Talus to the first metatarsal which was reinforced by 3.5 mm fully threaded cortical screws passing from Navicular bone to the medial cuneiform bone and 2.7 mm plate (Fig. 4). The histopathology of the excised bone showed features of a bone-forming tumor consisting of anastomosing woven trabeculae lined by a layer of plump osteoblasts in a vascularized stroma and no evidence of pleomorphism or mitoses (Fig. 5). The soft tissue did not demonstrate any tumor deposits or infiltration.
The lateral column was stabilized by filling the void created by removal of Cuboid bone with tricortical iliac crest bone graft and fixed with a 3.5 mm locking reconstruction plate extending from the calcaneum to the fourth metatarsal. Intraoperatively medial column instability was observed and confirmed under fluoroscopy and hence a decision to stabilize the column was made (Fig. 4). A longitudinal incision was made over the dorsum of the foot in the interval between the first and second ray and neurovascular bundle isolated. The medial column was stabilized using a spanning reconstruction locking plate extending from Talus to the first metatarsal which was reinforced by 3.5 mm fully threaded cortical screws passing from Navicular bone to the medial cuneiform bone and 2.7 mm plate (Fig. 4). The histopathology of the excised bone showed features of a bone-forming tumor consisting of anastomosing woven trabeculae lined by a layer of plump osteoblasts in a vascularized stroma and no evidence of pleomorphism or mitoses (Fig. 5). The soft tissue did not demonstrate any tumor deposits or infiltration.
After surgery, the patient was given a below knee slab for 6 weeks. After 6 weeks, an Air Cast Boot (Donjoy, USA) was applied and ankle ROM exercises were started. Weight bearing mobilization with air boot support started at around 3 months and weaning from the boot done gradually. Patient was on regular follow-up and was evaluated clinically and radiographically with X-rays (Fig. 6).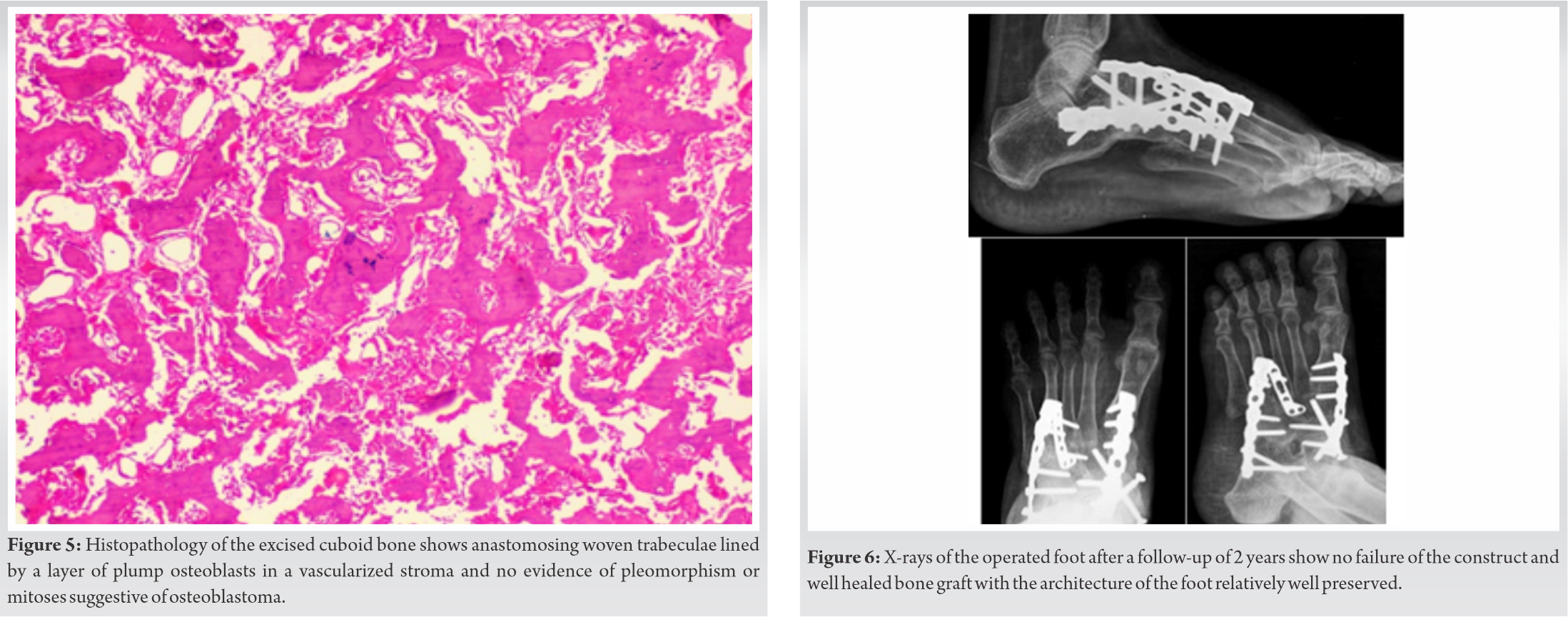 A positron emission tomography scan was performed after 2 years and showed no evidence of recurrence. After a follow-up period of 2 years, the patient is ambulatory and demonstrates complete ankle ROM and her mid-foot AOFAS score improved to 81.
A positron emission tomography scan was performed after 2 years and showed no evidence of recurrence. After a follow-up period of 2 years, the patient is ambulatory and demonstrates complete ankle ROM and her mid-foot AOFAS score improved to 81.
TB of bones is often described as a great mimic often presenting with clinical features similar to other disorders thereby causing significant confusion in obtaining a clinical diagnosis [6]. By virtue of its extensive prevalence in developing countries, many clinicians often tend to over diagnose atypical bone lesions as TB and treat accordingly leading to delayed diagnosis and management of the original pathology. Osteoblastoma of the cuboid is a very rare condition and only one case report has been published in the literature recently [5] and none reported from the Indian subcontinent. Due to the paucity of literature, there are no definite management guidelines for the treatment of this condition in this location. Furthermore, due to similar presentation such as TB foot, the treatment was delayed in our case leading to osteopenia, medial column instability, and early mid-foot arthritis leading to a more complicated surgical solution.
The differential diagnosis of osteoblastoma is most commonly an osteoid osteoma [3]. Both these tumors present with similar clinical and histological features such as increased osteoid tissue surrounded by vascular fibrous tissue and perilesional sclerosis. However, osteoblastomas tend to present as larger size lesions predominantly in the axial skeleton and they are often less painful with the pain not relieved by NSAIDS. Furthermore, osteoblastomas are more aggressive in nature and often require surgical treatment [7]. The other differential diagnoses of osteoblastoma are osteoblastoma like osteosarcoma (OBLOS) [8] and acrometastasis of foot [9]. OBLOS of the foot is a rare condition that shares similar clinical and radiological characteristics of osteoblastoma but behaves more aggressively like an osteosarcoma. The diagnosis is often made based on histological examination in which OBLOS displays increased mitotic activity with atypical mitotic figures and permeation in the surrounding tissues [10]. The treatment of OBLOS is similar to osteosarcoma and includes surgery along with chemotherapy. Acrometastases of foot often present radiologically as osteolytic lesions with ill-defined margins and bear close similarities to osteoblastoma, which can occasionally present radiologically as a lytic lesion with or without matrix mineralization surrounded by a zone of sclerosis. TB of the foot is seldom considered in the differential diagnosis of osteoblastoma as the clinical, radiological presentation is different but an osteolytic variety of TB foot has been reported which can often lead to clinical confusion [11]. We suspect the possible clinical conundrum in our case report may be due to the coexistence of osteoblastoma of cuboid along with TB foot and hence the radiological suspicion would have pointed more toward TB than an osteoblastoma. This is probably the reason the patient may have had persistent pain even after starting ATT and did not report complete pain relief.
The treatment of choice in osteoblastoma is complete excision of tumor followed by bone grafting or bone cement [12]. Studies have reported that these cases need wide excision and extended curettage compared to osteoid osteoma as they have a possibility of recurrence [13]. Due to the delay in the diagnosis and the presence of mid foot instability, the surgical procedure in our case was more complicated and involved en bloc excision of the cuboid with tricortical Iliac crest bone grafting and fusion of the lateral and medial columns of the foot using locking plates. The results after en bloc excisions of the Cuboid are often good and patients can resume normal function in most cases but these patients should be under a long term regular follow-up due to the possibility of recurrence or malignant transformation [14].
Cuboid osteoblastoma can present atypically with mid foot collapse and arthritis leading to en erroneous diagnosis of TB due to the concomitant inflammation. Hence, any atypical lesion of the foot should be subjected to biopsy and a confirmatory result before initiating any therapy.
Osteoblastoma of cuboid is a very rare presentation of this tumor with only one case report published previously . It can lead to mid foot collapse and lead to considerable morbidity if neglected. In view of the prevalence of TB foot in the Indian subcontinent which can often present with an infective arthritis and arch collapse, clinicians should be vigilant about the diagnosis and should confirm their diagnosis by biopsy.
References
- 1.Lucas DR. Osteoblastoma. Arch Pathol Lab Med 2010;134:1460-6. [Google Scholar]
- 2.Lucas DR, Unni KK, McLeod RA, O’Connor MI, Sim FH. Osteoblastoma: Clinicopathologic study of 306 cases. Hum Pathol 1994;25:117-34. [Google Scholar]
- 3.Healey JH, Ghelman B. Osteoid osteoma and osteoblastoma. Clin Orthop Relat Res 1986;204:76-85. [Google Scholar]
- 4.Marsh BW, Bonfiglio M, Brady LP, Enneking WF. Benign osteoblastoma: Range of manifestations. J Bone Joint Surg 1975;57-A:1-9. [Google Scholar]
- 5.Rovere G, Stramazzo L, Pavan D, Cioffi A, Orlando E, D’Arienzo A, et al. Isolated osteoblastoma of the cuboid bone: A case report and review of the literature. Foot 2020;45:101691. [Google Scholar]
- 6.Dhillon MS, Nagi ON. Tuberculosis of the foot and ankle. Clin Orthop Relat Res 2002;398:107-13. [Google Scholar]
- 7.Chandra S, Puri N, Harsh M, Juyal AK. Cytological diagnosis of osteoblastoma of the talus: Case report with unusual presentation and diagnostic pitfalls. Cytojournal 2018;15:20. [Google Scholar]
- 8.Kumar NL, Rosenberg AE, Raskin KA. Osteoblastoma-like osteosarcoma of the cuboid: A case report. J Orthop Surg Res 2010;5:52-6. [Google Scholar]
- 9.Maccauro G, Esposito M, Muratori F, Gebert C, Gosheger G, Logroscino CA. A report of a very rare localization of bone metastasis to the talus Eur J Orthop Surg Traumatol 2006;16:67-9. [Google Scholar]
- 10.Wu W, Zhao G, Chen J, Qian S, Shu Q. Osteoblastoma like osteosarcoma of the cuboid and skull: A case report and review of the literature. J Foot Ankle Surg 2020;59:156-61. [Google Scholar]
- 11.Dhillon MS, Aggarwal S, Prabhakar S, Bachhal V. Tuberculosis of the foot: An osteolytic variety. Indian J Orthop 2012;46:206-11. [Google Scholar]
- 12.Saglik Y, Atalar H, Yildiz Y, Basarir K, Gunay C. Surgical treatment of osteoblastoma: A report of 20 cases. Acta Orthop Belg 2007;73:747-53. [Google Scholar]
- 13.Günel U, Dağlar B, Günel N. Long-term follow-up of a hip joint osteoblastoma after intralesional curettage and cement packing: A case report. Acta Orthop Traumatol Turc 2013;47:218-22. [Google Scholar]
- 14.Padubidri AA, Bertrand TE. Transformation of ischial osteoblastoma into high-grade osteoblastoma-like osteosarcoma. Orthopedics 2019;42:e343-5. [Google Scholar]