Learn to identify and treat scaphoid dislocations according to its classification and disrupted structures.
Dr. Maria R. Vaz, Serviço de Ortopedia e Traumatologia, Centro Hospitalar Tondela, Viseu, Portugal. E-mail: mritacvaz@gmail.com
Introduction:Scaphoid dislocations are rare injuries, usually resulting from high-energy trauma and therefore associated to other lesions which may obscure the diagnosis.
Case Presentation:The authors present a case of a 59-year-old man with a partial complex dislocation of the scaphoid, diagnosed 6 days after the initial injury. Closed reduction was unsuccessfully attempted, so the patient was submitted to open reduction and internal fixation. The functional and radiological results were good.
Conclusion: Physicians should be aware of this rare lesion, because a delayed diagnosis may rend the treatment more difficult and compromise the results. The threshold for an open treatment should be low because rotatory subluxations of the scaphoid may not be detectable in simple radiographs and be responsible for the appearance of degenerative changes in the long term.
Keywords: Scaphoid dislocation, carpal dislocation, wrist trauma.
Isolated scaphoid dislocation is a rare injury, with few case reports described in literature [1]. They usually result from high-energy trauma and, therefore, can be associated with other injuries, which sometimes obscure its diagnosis.
We present a case report of a scaphoid bone dislocations treated in our institution, as well as a review of the cases described in literature.
A 59-year-old man who works as a police officer presented at the emergency department 6 days after sustaining a fall from a bicycle with trauma to his right wrist. On the day of the injury, he had been evaluated for a head and face trauma, so no other lesions were investigated.
He complained of mild pain and functional impairment. At clinical examination, there was a palpable mass immediately distal to the radial styloid, tender to palpation. Passive mobilization was painful and restricted, and no neurologic deficit was present.
Plain radiographs and computed tomography (CT) scans revealed a palmar dislocation of the proximal pole of the scaphoid (Scapho-trapezium-trapezoid [STT] joint intact), a disruption of capitohamate (CH), and intermetacarpal joint (between the 3rd and 4th metacarpals) with concomitant proximal migration of the capitate. In addition, a Chauffeur-type fracture of the radial styloid was present (Fig. 1 and 2).
After trying closed reduction with no success, the patient was taken to the operating theater, and an open reduction was performed through a dorsal approach. The scaphoid was fixed with two Kirschner wires (from the scaphoid to the lunate and capitate). Repair of the dorsal scapholunate (SL) ligament was made with two suture anchors (Fig. 3). The wrist was immobilized in a scaphoid-type cast for 6 weeks, after which the Kirschner wires were removed, and mobilization was permitted.
Twelve months after surgery, the patient reported no pain nor functional limitation. Range of motion (ROM) of his right wrist ranges from 50° of flexion to 35° of extension, radial and ulnar inclination 25° and 10°, respectively (Fig. 4, 5). He returned to work as a police officer with no limitations 5 months after injury.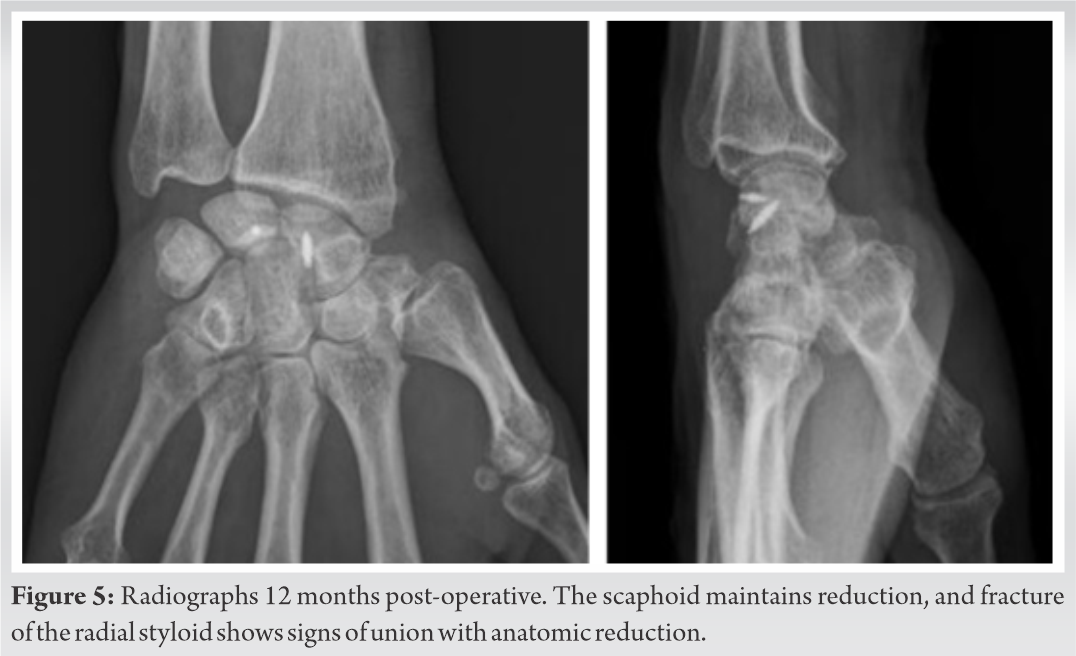
Dislocation of the scaphoid bone was first described by Higgs in 1930 [1]. Since then, to the best of our knowledge, there are 63 case reports in the literature.
Although the exact mechanism of dislocation is unknown [2], most dislocations are caused by violent extension of the wrist while the hand is grasping a fixed object in ulnar inclination [3], for example, in a motor vehicle crash in which there is an axial loading to a wrist while holding a steering wheel or a handlebar. However, other mechanisms have been described, like a fall from height [4, 5, 6] or compressive trauma to the wrist [2, 7, 8].
The rarity of scaphoid dislocations is explained by the fact that the amount of energy needed to dislocate the scaphoid most commonly results in fractures of the radial styloid or waist of the scaphoid [9]. This high-energy trauma may result in massive soft-tissue trauma and present with open injuries [6], as well with associated fractures of the radial styloid or other carpal bones [1, 2, 10, 11, 12, 13].
Patients usually complain of pain and functional limitation of the wrist. On physical examination, the wrist is swollen and a bony prominence corresponding to the dislocated scaphoid may be present, as well as an empty anatomical snuffbox. Passive and active mobilizations are restricted and very painful [2]. Signs of median nerve compression may be present, especially in palmar-ulnar dislocations [14].
Plain radiographs are usually sufficient for accurate diagnosis [13]. Initial evaluation must include anteroposterior (AP) and lateral views, and additional views such oblique or AP with ulnar inclination may aid the diagnosis. AP view of the wrist may show the “signet ring sign,” indicating rotation of the scaphoid and suggesting injury to the SL ligament [13].
Arthrogram or magnetic resonance imaging can be used to assess subtle ligament injury. Arthroscopy can be used as both diagnostic and therapeutic modalities if other imaging tools are non-diagnostic. CT scan will help in assessing associated bony injury [10].
Leung et al. [14] have proposed a classification system to scaphoid dislocations:
1. Primary versus secondary. Primary dislocations result directly from the injury, whereas in secondary injuries, the dislocation occurs after a closed reduction of another carpal dislocation
2. Simple versus complex. Simple dislocations involve only the scaphoid bone. In complex dislocations, there are also disruptions of the distal carpal row (CH and 3rd/4th metacarpal joints)
3. Partial versus total, depending on which ligaments are disrupted. In total dislocations, no soft tissues remain attached to the scaphoid. Alternatively, in the partial type, the proximal pole of the scaphoid may lose contact with the lunate and radius, while the STT joint remains intact
4. Direction of dislocation is described as pure radial, palmar-radial, palmar-straight, palmar-ulnar, or dorsal. The position of the wrist at the moment of the injury may be related to the direction of dislocation of the proximal pole of the scaphoid.
The severity of the dislocation depends on the number of ligaments disrupted [1, 2, 15] and consequently the reducibility and stability of the carpus [16]. Szabo described a sequence of ligamentous failure, beginning in the radiopalmar aspect of the proximal pole of the scaphoid (radioscaphocapitate [RSC] and SL ligaments), followed by long radioulnar ligament and last by STT ligaments [1]. Avulsion fractures may be present and are equivalent to ligament injury, for example, a radial styloid fracture remains attached to the scaphoid and is equivalent to an injury to the RSC ligament [13].
Primary scaphoid dislocations represent a spectrum of injuries [14]. An axial force transmitted to an extended and ulnar inclined wrist exerts pressure from the 3rd and 4th metacarpals through the capitate and the medial column of the carpus. The first structure to be injured is the SL ligament (without dislocation). With persistence of the force, there is a rupture of RSC ligament, allowing the proximal pole of the scaphoid to dislocate (partial dislocation). Finally, injury to the STT joints will lead to a complete dislocation of the scaphoid [14]. If the axial force is sufficient, the capitate is forced to dislocate proximally, leading to an axial radial dislocation of the carpus, with disruption of the CH and intermetacarpal joint [11].
In our review of the literature, we found 53 cases of primary dislocations of the scaphoid, and 10 were secondary to dorsal periulnar dislocations.
Of the primary dislocations, 14 were classified as complex, associated with a CH and intermetacarpal dissociation or a fracture of the hamate. Complete dislocation (with injury to all the ligament attachments to the scaphoid) was described in 16 patients.
Being such an uncommon injury, all published literature are case reports with no randomized controlled studies, and consequently, there are no evidence-based guidelines for its treatment.
First published data report good results with closed reduction and immobilization, but in more recent years, open reduction and fixation with Kirschner wires, associated or not with ligament repair or reconstruction, has been more and more advocated. This change of paradigm is due to the awareness that residual rotatory subluxation may be a long-term complication of closed reduction [17].
Chloros et al. [2] proposed an algorithm for treatment, based on the classification of the injury: Open reduction and fixation with Kirschner wires is primarily indicated in complex dislocations, and simple ulnar dislocations (the latter with carpal tunnel release), because they are invariably associated with a compression of the median nerve [14]. For dislocations with more than a week, attempts of closed reduction would be unsuccessful, so open reduction is also advisable. As for the remainder simple dislocations, closed reduction can be attempted. If resulting SL interval is inferior to 2 mm, one can perform fixation with Kirschner wires. If closed reduction is not achieved or there is an increased SL interval, either an open reduction or an arthroscopy is indicated.
Correct anatomic reduction can be difficult with closed reduction methods, and incorrect alignment may predispose to complications as pin failure, poor functional outcomes, and secondary dislocation. The previous case reports treated with closed reduction alone had a 43% chance of needing a revision surgery [9].
Use of Kirschner wires to fix the carpal bones after satisfactory reduction may not be necessary and it seems not to affect the outcome [14]. There are authors that advocate the use of K-wires if the reduction is not very stable, especially in late cases and complex dislocations – it assures good healing of the ligaments and prevents future rotatory subluxation [14].
In our review of the literature, 19 patients have been treated with closed reduction and three of them with additionally percutaneous fixation with Kirschner wires, being the most frequent complication described a mild-to-moderate loss of flexion-extension range of movement of the wrist. Four cases of SL dissociation were described, and one patient had dorsal intercalated segment instability (DISI) deformity and degenerative changes at the CH joint, however, no other surgeries were performed as the patient did not have any complaints of pain of functional impairment.
Sides and Szabo reported two cases of closed reduction with arthroscopic support [2, 9]. Arthroscopy before open reduction can be useful to evaluate the presence of soft-tissue interposition and attempt to free them, anatomically reduce the scaphoid, and repair the torn ligaments before new percutaneous pinning [2]. In our review of literature, two patients were treated with closed reduction aided by arthroscopy and fixation with Kirschner wires.
Open reduction was performed in 37 patients: 10 without additional fixation and 26 with Kirschner wires (of the latter, one with additional arthrodesis of the CH joint, one case with arthrodesis of the STT joint, and one with a SL transarticular Herbert screw). In one case, after open reduction, only osteosynthesis of a lunate avulsion-type fracture was made. As for soft-tissue repair, it was performed in 13 patients, mostly associated with bone fixation (by means of simple suture or anchors, and two cases of osteosynthesis of avulsion fractures of the lunate or scaphoid).
In long-standing cases, arthrodesis or excision of the scaphoid may be necessary [18]. Proximal row carpectomy was performed in three patients (one of them associated with radiocapitate arthrodesis). It is said to provide functional ROM and adequate grip strength with good outcomes: In literature, the range of flexion-extension and grip strength compared to the contralateral side was 62% and 80%, respectively, with patient satisfaction ranging from 80% to 100% [10].
The most frequent complication described was loss of motion compared to the contralateral side in variate degrees (27 patients), mostly on flexion-extension and ulnar inclination. Pain and loss of grip strength were also reported (especially in extremes of movement or after efforts) and usually described as mild to moderate.
As for radiographic follow-up, an increased SL interval was reported in six patients (submitted to open reduction) and one case of DISI deformity was observed after closed reduction and pinning. Arthritic changes were only described in three cases: This small number of cases can be due to a short period of follow-up in most studies.
There are two cases of avascular necrosis described in literature, described by Szabo [6, 14] and Lichtman [11]. This complication is believed to be unlikely, because in partial dislocations, the remaining ST and capsular attachments provide sufficient blood supply [7, 14, 19]. In case of complete dislocation where the STT ligament is also disrupted, the intact intraosseous channels inside de scaphoid bone are believed to allow rapid revascularization from the surrounding soft tissues [3, 7]. Other proposed explanation for the low prevalence of avascular necrosis is the rapid revascularization of the scaphoid once continuity of the ligamentous structures is achieved [20].
The most significant risk factor for poor prognosis is delayed diagnosis and treatment, especially if it is longer than 1 week [3, 14]. A delay of several weeks will inevitably result in the presence of fibrotic tissue that will ultimately lead to stiffness and degenerative changes in intercarpal and radiocarpal joints. In literature, there were 27 cases where the diagnosis was delayed (from 2 days to 8 months), because of late presentation of the patient or overlooking of the lesion at the day of injury. This delay will influence the treatment strategy, almost certainly precluding the success of closed reduction.
Globally accepted guidelines for the treatment of scaphoid dislocations are not yet defined, due to the paucity of data and absence of randomized controlled trials in the literature. It seems that, in acute cases, closed or open reduction will lead to similar clinical results. However, in delayed diagnosed cases, open reduction is generally indicated, as closed reduction will be almost certainly unsuccessful. Long-term results were only evaluated in a few studies, so we cannot assess if instability or arthritic changes will develop regardless of the treatment method or accuracy of reduction.
Our patient was diagnosed 6 days after the injury, so closed reduction would be most probably unsuccessful. This delay in diagnosis may also rend open reduction more difficult due to fibrotic changes. The patient had no complaints and no functional limitation; however, the period follow-up was short.
More studies are needed to evaluate in what extent the delay in surgical treatment may influence the long-term outcome, and if open reduction is really associated with better long-term outcomes than correct closed reduction.
This report of a rare injury may help physicians to be aware and look for it in a polytrauma context, to avoid a delay in treatment.
References
- 1.Ballas EG, Raptis K, Stathopoulos IP, Stavropoulos NA, Spyridonos SG. Unusual complete isolated scaphoid dislocation, report of a case. Arch Bone Joint Surg 2017;5:332-6. [Google Scholar]
- 2.Chloros GD, Themistocleous GS, Zagoreos NP, Korres DS, Efstathopoulos DG, Soucacos PN. Isolated dislocation of the scaphoid. Arch Orthop Trauma Surg 2006;126:197-203. [Google Scholar]
- 3.Kiliç M, Kalali F, Unlü M, Yildirim OS. Isolated carpal scaphoid dislocation. Acta Orthop Traumatol Turc 2012;46:68-71. [Google Scholar]
- 4.Fernández JM, López JM, Galtés PG, Redondo FC. Palmar scaphoid dislocation associated with dorsal perilunate dislocation. A case report and review of the literature.Rev Esp Cir Ortop Traumatol 2013;57:140-4. [Google Scholar]
- 5.Lee BJ, Kim SS, Lee SR, Jin JM, Yoon MG, Moon MS. Palmar scaphoid dislocation associated with dorsal perilunate dislocation: Case report. J Hand Surg Am 2010;35:726-31. [Google Scholar]
- 6.Horton T, Shin AY, Cooney WP 3rd. Isolated scaphoid dislocation associated with axial carpal dissociation: An unusual injury report. J Hand Surg Am 2004;29:1102-8. [Google Scholar]
- 7.Baek JR, Cho SH, Lee YS, Roh YH. Neglected isolated scaphoid dislocation. Indian J Orthop 2016;50:693-6. [Google Scholar]
- 8.Yamabe E, Nakamura T, Matsumura T, Toyama Y. Re: Palmar dislocation of the scaphoid with dorsal perilunate dislocation. J Hand Surg Eur Vol 2008;33:682-3. [Google Scholar]
- 9.Sides D, Laorr A, Greenspan A. Carpal scaphoid: Radiographic pattern of dislocation. Radiology 1995;195:215-6. [Google Scholar]
- 10.Amaravati RS, Saji M, Rajagopal H, Gururaj H. Neglected dorsal dislocation of the scaphoid. Indian J Orthop 2009;43:213-5. [Google Scholar]
- 11.Polveche G, Cordonier D, Thery D, Desrousseaux JF. An unusual variation of luxation of the wrist: external vertical luxation. Apropos of a case. Review of the literature. Ann Chir Main Memb Super 1995;14:159-66. [Google Scholar]
- 12.Richards RS, Bennett JD, Roth JH. Scaphoid dislocation with radial-axial carpal disruption. AJR Am J Roentgenol 1993;160:1075-6. [Google Scholar]
- 13.Arora J, Anand P. Dislocation of the carpal scaphoid: A case report. Injury Extra 2006;37:184-6. [Google Scholar]
- 14.Leung YF, Wai YL, Kam WL, Ip PS. Solitary dislocation of the scaphoid. From case report to literature review. J Hand Surg Br 1998;23:88-92. [Google Scholar]
- 15.Sefcik R, Andrews K, Stirton J, Lea J, Tanios M, Skie M. A case report of an isolated dislocation of the scaphoid in a lesser arc injury and a review of the literature. Case Rep Orthop 2018;2018:9591502. [Google Scholar]
- 16.Cherif MR, Ben Ghozlen R, Chehimi A, Annabi H, Trabelsi M, Mbarek M, et al. Luxation isolée du scaphoïde carpien. A propos d’un cas avec revue de la littérature [Isolated dislocation of the carpal scaphoid. A case report with review of the literature]. Chir Main 2002;21:305-8. [Google Scholar]
- 17.Ritchie DA, Gibson PH. Isolated dislocation of the scaphoid. Injury 1988;19:405-6. [Google Scholar]
- 18.Connell MC, Dyson RP. Dislocation of the carpal scaphoid; report of a case. J Bone Joint Surg Br 1955;37-B:252-3. [Google Scholar]
- 19.Kolby L, Larsen S, Jørring S, Sørensen AI, Leicht P. Missed isolated volar dislocation of the scaphoid. Scand J Plast Reconstr Surg Hand Surg 2007;41:264-6. [Google Scholar]
- 20.Antuna SA, Antuna-Zapico JM. Open dislocation of the carpal scaphoid: A case report. J Hand Surg Am 1997;22:86-8. [Google Scholar]











