Atypical diaphyseal fractures of the femur in association with familial hypokalemic periodic paralysis (FHPP) is an unknown entity and a clinician should be watchful for them, especially when the patient complains of pain in the extremities.
Dr. Amit Sharma, Department of Trauma and Emergency, Orthopaedics, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India. E-mail: dramit.aks@gmail.com
Introduction:Hypokalemic periodic paralysis (HPP) is an important and a reversible but rare cause of paralysis. Periodic paralyses are of two types. The first one is primary which is also known as familial type and the second one is secondary periodic paralysis which is due to other underlying pathologies [1]. Important secondary causes can be categorized as metabolic, infectious and losses from the body, etc. [2]. HPP associated with bony abnormalities in form of spontaneous atypical fractures in femoral shaft with coxa vara is an unusual presentation.
Case Report:Here is a case report of 26 year old lady who presented with pain in the proximal part of right thigh and weakness in both the upper and the lower limbs. She was diagnosed as familial HPP (FHPP) with atypical fracture of proximal third diaphysis of femur. Confirmation of the expected diagnosis was done with history, laboratory tests, and plain radiographs. Previously also, she had similar episode of weakness and opposite side femur atypical fracture.
Conclusion:Association of atypical femur diaphysis fracture and FHPP is a rare presentation of an uncommon disease but should be kept in mind whenever treating any HPP patient. The patient complaining of pain in limbs should be taken seriously as atypical fractures are prone to be missed. In future, further genetic studies are required to establish this rare association.
Keywords:Hypokalemic periodic paralysis, atypical fracture femur, hypokalemic periodic paralysis.
Hypokalemic periodic paralysis (HPP) is a reversible and a treatable cause of acute flaccid paralysis, faced by physicians many times during emergency visits. Weakness may last from hours to days, and depends on the correct diagnosis and timely treatment. It’s a diagnosis of exclusion, and poses a challenge to the treating doctor. HPP has a prevalence rate of 1 in 100,000 [3]. HPP is classified as primary or familial HPP (FHPP) and secondary due to other underlying causes. FHPP is transmitted as an autosomal dominant trait in 2/3 of cases and sporadic in the remainders. FHPP mainly affects Caucasians with male predominance [4]. Important secondary causes of HPP are thyrotoxicosis, renal tubular acidosis, Gitelman syndrome, Barter syndrome, Liddle syndrome, diuretics, hyper-aldosteronism, gastrointestinal losses, barium poisoning, and drugs such as insulin and beta-2 agonist [4, 5].
We are presenting an extremely rare case of FHPP associated with an atypical fracture in the proximal third of shaft of right femur. Five years ago, she had a femur shaft fracture of the left side following a trivial trauma for which she was operated on in the form of intramedullary (IM) nailing. Association of an atypical fracture and a fracture following a trivial trauma in young age with FHPP is a rare occurrence. On literature search, we could not find any similar association. This signifies that some factors which regulate the bone metabolism also get affected in cases of FHPP.
A 26-year-old female presented with normal vitals and weakness in all four limbs with pain in the right proximal thigh (Fig. 1). On detailed history, it was noted that 5 years ago, she had fracture of proximal shaft of femur in the left side following a ground level fall for which she had medical and surgical treatment (Fig. 2). On detailed examination, motor weakness in all four limbs, diminished deep tendon reflexes, downgoing plantar reflex, absent clonus, and normal sensory and cranial functions were noted. There was negative history for fever, trauma, drug intake, or any chronic illness. On laboratory analysis, thyroid profile, blood counts, random and fasting blood sugar, erythrocyte sedimentation rate, C-reactive protein, kidney function test, liver function test, and urine analysis were in normal range. Antinuclear antibody test was negative and serum parathyroid hormone (PTH) was in normal range (23.4 pg/ml) with Vitamin D insufficiency (value – 24.9 ng/ml). Serum electrolytes were in normal range except potassium level which was low (2.31 mg/dl). Specific electrocardiogram changes for low potassium were absent. The patient had normal acid base balance with urinary potassium level in normal limit. On plain radiograph, there was an atypical fracture of proximal diaphysis of femur in the right side with united fracture of the left proximal diaphysis of femur with IM nail in situ. The current fracture was transverse in orientation with an increase in anterolateral bowing. There were sclerotic changes at the lateral cortex. Coxa vara of femoral head and neck in both sides was noted (Fig. 3). As there was no laboratory finding abnormality except for decreased serum potassium level and marginally low serum Vitamin D3 level, the patient was diagnosed as FHPP with an atypical femur fracture in the right side with operated left femur with implant in situ. On oral therapy of potassium replacement, the patient completely recovered from weakness. Since the fracture was incomplete, the fracture of femur was managed by non-weight-bearing for 6 weeks followed by guarded weight-bearing and activity modification. Injection teriparatide was started to stimulate the bone healing. By 3 months, she again started walking with full weight-bearing and radiologically the fracture showed signs of bone union (Fig. 4). Local pain and tenderness at the fracture site disappeared completely.
On detailed examination, motor weakness in all four limbs, diminished deep tendon reflexes, downgoing plantar reflex, absent clonus, and normal sensory and cranial functions were noted. There was negative history for fever, trauma, drug intake, or any chronic illness. On laboratory analysis, thyroid profile, blood counts, random and fasting blood sugar, erythrocyte sedimentation rate, C-reactive protein, kidney function test, liver function test, and urine analysis were in normal range. Antinuclear antibody test was negative and serum parathyroid hormone (PTH) was in normal range (23.4 pg/ml) with Vitamin D insufficiency (value – 24.9 ng/ml). Serum electrolytes were in normal range except potassium level which was low (2.31 mg/dl). Specific electrocardiogram changes for low potassium were absent. The patient had normal acid base balance with urinary potassium level in normal limit. On plain radiograph, there was an atypical fracture of proximal diaphysis of femur in the right side with united fracture of the left proximal diaphysis of femur with IM nail in situ. The current fracture was transverse in orientation with an increase in anterolateral bowing. There were sclerotic changes at the lateral cortex. Coxa vara of femoral head and neck in both sides was noted (Fig. 3). As there was no laboratory finding abnormality except for decreased serum potassium level and marginally low serum Vitamin D3 level, the patient was diagnosed as FHPP with an atypical femur fracture in the right side with operated left femur with implant in situ. On oral therapy of potassium replacement, the patient completely recovered from weakness. Since the fracture was incomplete, the fracture of femur was managed by non-weight-bearing for 6 weeks followed by guarded weight-bearing and activity modification. Injection teriparatide was started to stimulate the bone healing. By 3 months, she again started walking with full weight-bearing and radiologically the fracture showed signs of bone union (Fig. 4). Local pain and tenderness at the fracture site disappeared completely.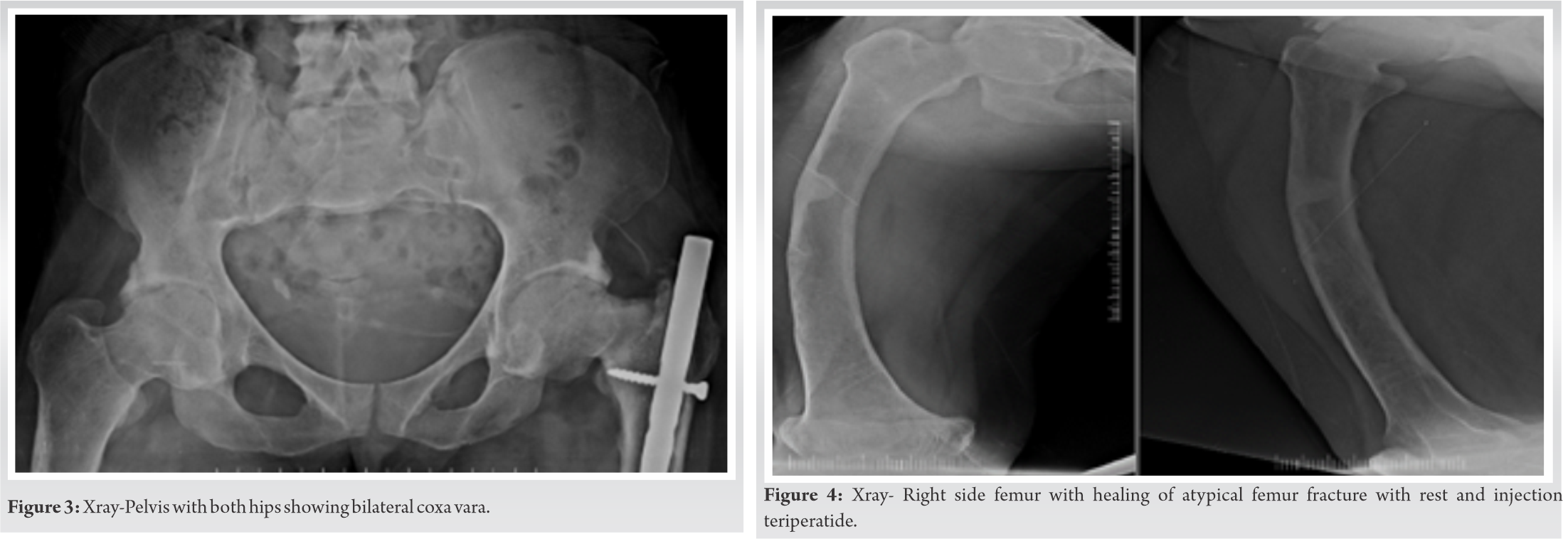
HPP is a considered as a rare differential diagnosis of acute flaccid paralysis but it’s reversible and treatable cause. Hence, every physician should take it into account after exclusion of other common entities. FHPP is primary cause of HPP with autosomal dominant trait presented before the age of 25 years [4]. FHPP is diagnosed when potassium level is below 3.5 mg/dl after excluding other secondary causes of HPP [6]. Calcium channelopathies are responsible in FHPP for acute influx of potassium into intracellular fluid which makes muscle fibers inexcitable. Mainly affected calcium channels are dihydropteridine binding voltage-gated skeletal muscle calcium channels [7]. New studies show that increase in sodium permeability is responsible for HPP [8, 9]. In secondary causes, literature is not agreed on one single cause as the most common cause. A few studies mention thyrotoxicosis, while others mention renal tubular acidosis as the most common cause [1, 5]. Treatment of choice is oral potassium replacement if the patient is able to take orally whereas acetazolamide is considered as prophylactic drug of choice [10].
An atypical fracture of femur diaphysis associated with FHPP is a very rare presentation. After a thorough search, we could not find any similar case reported in the literature. Negative drug history, normal PTH levels, and normal renal profile excluded any calcium-Vitamin D metabolism abnormality. Furthermore, the patient had only marginally low level of serum Vitamin D level (24.9 ng/ml) and her BMI was not indicating of any severe form of osteoporosis which could explain an atypical diaphyseal femur fracture and a fracture following a ground level fall (T score – 0.5).
Limitation of our study was an absent genetic work-up due to the limitation of resources and patient’s unaffordability. An atypical fracture in this patient warrants searching for any possible genetic association between FHPP and bone metabolism.
Association of atypical femur diaphysis fracture and FHPP is a rare presentation of an uncommon disease but should be kept in mind whenever treating any HPP patient. The patient complaining of pain in limbs should be taken seriously as atypical fractures are prone to be missed. In future, further genetic studies are required to establish this rare association.
Atypical femur fracture is known in association with bisphosphonate therapy, but it is quite unusual to see in a case of FHPP. The case concerned has not been on bisphosphonate therapy. Furthermore, no metabolic cause was found on endocrinological evaluation.
References
- 1.Sinha U, Sengupta N, Sinharay K, Sahana PK. Recurrent hypokalemic paralysis: An atypical presentation of hypothyroidism. Indian J Endocr Metab 2013;17:174-6. [Google Scholar]
- 2.Bhatti S, Huq T, Uddin SM, Haq A, Kazmi SA, Yaqoob U, et al. Hypokalemic periodic paralysis with reversible electrophysiological abnormalities: A case report. J Med Cases 2018;9:177-8. [Google Scholar]
- 3.Fontaine B. Periodic paralysis. Adv Genet 2008;63:3-23. [Google Scholar]
- 4.Ahlawat SK, Sachdev A. Hypokalaemic paralysis. Postgrad Med J 1999;75):193-7. [Google Scholar]
- 5.Chandramohan G, Dineshkumar T, Arul R, Seenivasan M, Dhanapriya J, Sakthirajan R, et al. Spectrum of hypokalemic paralysis from a tertiary care centre in India. Indian J Nephrol 2018;28:365-9. [Google Scholar]
- 6.Stedwell RE, Allen KM, Binder LS. Hypokalemic paralyses: A review of the etiologies, pathophysiology, presentation and therapy. Am J Emerg Med 1992;10:143-8. [Google Scholar]
- 7.Fontaine B, Trofatter J, Rouleau GA, Khurana TS, Haines J, Brown R, et al. Different gene locii for hyperkalemic and hypokalemic periodic paralysis. Neuromusc Disord 1991;1:235-8. [Google Scholar]
- 8.Rudel R, Lehmann-Horn F, Ricker K, Kuher G. Hypokalemic periodic paralysis: In vitro investigation of muscle fiber membrane parameters. Muscle Nerve 1984;7:110-20. [Google Scholar]
- 9.Troni W, Doriguzzi C, Mongini T. Interictal conduction slowing in muscle fibers in hypokalemic periodic paralysis. Neurology 1983;33:1522-5. [Google Scholar]
- 10.Levitt JO. Practical aspects in the management of hypokalemic periodic paralysis. J Transl Med 2008;6:18. [Google Scholar]









