Fixation of an osteoporotic fracture needs special planning, out-of-the-box execution, and prompt management of complications.
Dr. Bishnu Prasad Patro, Department of Orthopedics, All India Institute of medical Sciences, Bhubaneswar. India. E-mail: bishnucolours@gmail.com
Introduction: Osteoporosis is a known complication of prolonged steroid therapy. Osteoporotic fracture is common in such a scenario and poses several challenges in its management. We present a case of neglected proximal humerus fracture in a 57-year-old osteoporotic female and the difficulties encountered in its management.
Case Report: A 57- year-old female, rheumatoid arthritis patient, is on steroids for the past ten years. Four years back, she sustained a fracture of the left humerus neck following a trivial trauma. The fracture was not managed by an orthopaedician and was treated by a general practitioner. She presented to us in a state of painless displaced non-union of fragments with severe osteoporosis. DEXA scan revealed severe osteoporosis. She was started on oral calcium, magnesium, and vitamin D supplementation. Along with oral supplementation, the patient was advised 20 mcg of Teriparatide subcutaneously once daily and single dose of Denosumab 60 mg subcutaneously. Non -vascularized free fibular graft was harvested from the ipsilateral lower limb. A five-hole PHILOS plate was used to fix the fracture. Intra-operatively, the humeral head appeared too indistinct under fluoroscopy leading to difficulty in estimating screw length. An indirect method was used to assess the screw length. The post-operative radiograph was satisfactory but radiograph after two weeks showed an un-displaced fracture adjacent to the distal end of the plate. It was decided to continue with conservative management by a “‘U”’ cast. A follow- up radiograph at three3 months showed complete union of the stress fracture at the distal end of the plate end and progressive union of the fracture at the primary site. But En- block pull-out of the locking plate was noticed in the distal fragment of the fracture in the follow-up radiograph at 9 months from surgery. The limb was further immobilized in an arm sling for more four weeks. At one year from operation, there was good union of fracture with acceptable shoulder movement.
Conclusion: Osteoporotic fractures are often difficult to treat. Careful pre-operative planning, active osteoporosis management, good implant selection, careful bone handling, and judicious rehabilitation are key to avoid complications and achieve good functional outcome.
Keywords: Osteoporotic, humerus, fracture, stress fracture, locking plate, implant failure.
Managing osteoporotic fractures are challenging for several reasons. Following any injury, the fragile bones break into multiple fragments [1]. Due to brittleness of the bone, the bone has a chance of further comminution during the process of fracture reduction and internal fixation. The stress riser at the junction of implant and bone can lead to further fracture in an osteoporotic bone. Impaired callus mineralization in osteoporotic bone may lead to delay in fracture healing. Porotic bone fails to provide adequate screw fixation leading to implant loosening and screw back out [2]. Management of osteoporotic fractures has high chance of complications such as poor implant fixation due to low bone quality and delayed fracture healing [3]. In such a scenario, vigilant management of osteoporosis, efficient surgical skills to handle the fragile bones during fracture reduction, and selection of suitable implants for fracture fixation are of paramount importance. There is a place for augmented fixation in osteoporotic bones such as structural bone graft and intramedullary fixation, to improve the outcome of fixation [4]. We present a case of neglected osteoporotic proximal humerus shaft fracture and share our challenges encountered in its management.
A 57-year-old female patient (height 141 cm and weight 50 kg and American Society of Anaesthesiologists physical status 2 presented with history of 4 years old neglected two-part fracture of neck of the left humerus. The fracture occurred by a trivial trauma while doing normal household activities. The fracture was not managed by an orthopedician and was treated by a general practitioner. The patient was a known case of rheumatoid arthritis and was on Deflazacort on varying doses for the past 10 years. On examination, the arm was deformed with angulation at proximal part, patient was moving the elbow and wrist in a tricky way as the fracture site was mobile and the arm was unstable. The fracture site was painless. The upper limb was supported by an arm sling to counter the heaviness of limb because of bony discontinuity. On the radiograph, there was two-part fracture of the neck of the humerus with thin cortices suggestive of osteoporosis. There was a loss of the medial cortex of the proximal segment of humerus and the distal fragment was resting on the lateral cortex. The distal fragment was placed at the right angle to the proximal fragment (Fig. 1). Routine biochemical evaluation including renal, liver, and thyroid function tests was within normal limits. Blood counts, serum electrophoresis, and para-thyroid hormone (PTH) levels were normal. Dual-energy X-ray absorptiometry (DEXA) scan was done which showed osteoporosis with a T score of –4.4. Patient was under the treatment of rheumatologist but on an irregular basis. The severely osteoporotic bone raised a possibility of decreased holding capacity for implants and subsequent failure of fracture fixation. Therefore, a decision to primarily manage osteoporosis and to defer fracture fixation was taken. She was started on oral calcium, magnesium, and Vitamin D supplementation. Teriparatide 20 mcg once daily subcutaneous injection was started. Serial radiographs were done at 6 weekly intervals to assess improvement in bone quality. Significant radiological improvement was not noted even after 9 months of teriparatide therapy. She was then administered a dose of Denosumab 60 mg subcutaneously hoping to improve bone quality and was planned for surgery. Pre-operative biochemical and hematological investigations were within normal limits. Pre-anesthetic check-up deemed the patient fit for surgery. The patient was taken for surgery under general anesthesia. With the patient in supine position, a deltopectoral approach was utilized to expose the fracture site. A large amount of fibrous tissue was encountered between the fracture fragments which was meticulously removed. As both the fracture fragments were at the right angle to each other, we encountered difficulty in reducing the fragments. When we tried to reduce the fragments with bone holding clamps, the clamp itself was crushing the bones. It was another difficulty that we encountered during the fracture fixation. Non-vascularized free fibular graft was obtained from the ipsilateral lower limb. The fibula was found to be very thin and was easily split into two halves by scissors. The split fibula was inserted inside the medullary canal and the fracture fragments were reduced over it. A five-hole PHILOS plate was used to fix the fracture fragments. The humeral head appeared too indistinct under fluoroscopic visualization leading to difficulty in estimating screw length while keeping a safe distance from the joint space (Fig. 2). A blunt Hohmann retractor was introduced in the joint space through the rotator interval and was used to demarcate the extent of humeral head under fluoroscopy to estimate screw length. While drilling, very minimal resistance was encountered and almost all screws in the humeral head were put without predrilling. As the rotator cuff was intact, we repaired the rotator interval that we incised during surgery and addressed the soft tissue as warranted during closure. Wound was closed in layers and a vacuum suction drain was placed. As the fixation of plate and screw to bone was not satisfactory due to porotic bones, a U-splint was applied to the patient’s limb along with a shoulder immobilizer to provide additional support to prevent implant failure. The post-operative course was uneventful. The post-operative radiograph was satisfactory, only one view of shoulder was possible due to the application of plaster U-splint (Fig. 3). A radiograph after 2 weeks of surgery during suture removal showed an un-displaced fracture adjacent to the distal end of the plate (Fig. 4).
A blunt Hohmann retractor was introduced in the joint space through the rotator interval and was used to demarcate the extent of humeral head under fluoroscopy to estimate screw length. While drilling, very minimal resistance was encountered and almost all screws in the humeral head were put without predrilling. As the rotator cuff was intact, we repaired the rotator interval that we incised during surgery and addressed the soft tissue as warranted during closure. Wound was closed in layers and a vacuum suction drain was placed. As the fixation of plate and screw to bone was not satisfactory due to porotic bones, a U-splint was applied to the patient’s limb along with a shoulder immobilizer to provide additional support to prevent implant failure. The post-operative course was uneventful. The post-operative radiograph was satisfactory, only one view of shoulder was possible due to the application of plaster U-splint (Fig. 3). A radiograph after 2 weeks of surgery during suture removal showed an un-displaced fracture adjacent to the distal end of the plate (Fig. 4). 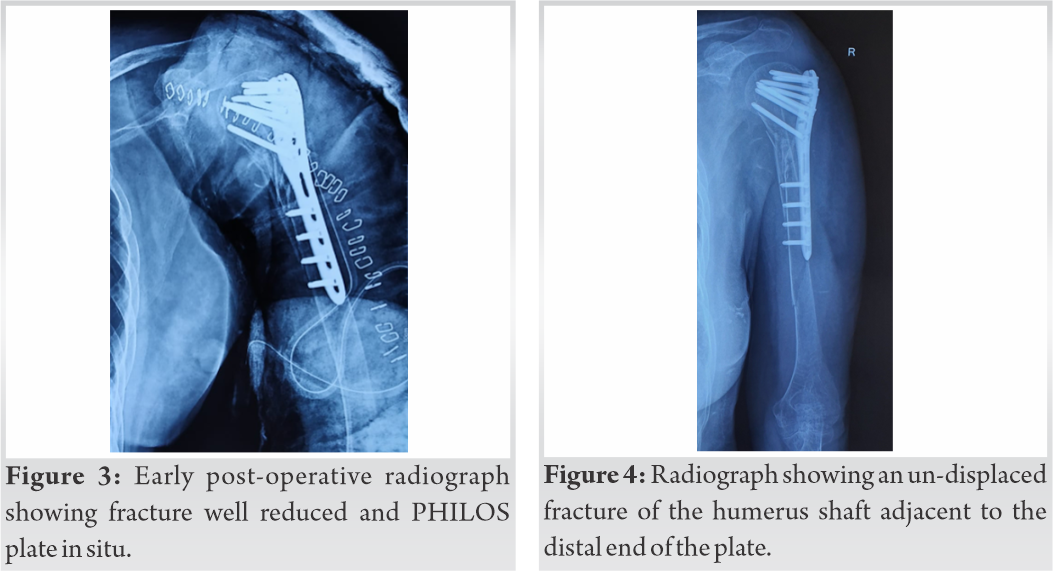 The options of management at this stage were either to revise the surgery with a longer plate or to proceed with a conservative management. After discussing both options with the patient, it was decided to continue with conservative management. In the conservative management, we had the option of functional bracing and U-cast, we preferred to go for U-cast as our experience in this case was different and we preferred to provide better stability of fracture. A follow-up radiograph at 6 weeks showed signs of fracture union and the cast was replaced with a custom-made functional brace. Although 6 weeks of U-cast can lead to joint stiffness, in our case, the prime objective was to achieve union of the fracture. Shoulder and elbow joint mobilization was started. A review radiograph after 12 weeks showed union of the stress fracture at the plate end and visible callus at the primary fracture site (Fig. 5). At 9-month postoperatively, en bloc pull-out of the locking plate was noticed in the distal fragment of the fracture (Fig. 6). The limb was further immobilized in an arm sling for 4 weeks. At 1 year, the limb was painless, had a sense of improved strength in her arm, and had an acceptable range of shoulder movement (Fig. 7).
The options of management at this stage were either to revise the surgery with a longer plate or to proceed with a conservative management. After discussing both options with the patient, it was decided to continue with conservative management. In the conservative management, we had the option of functional bracing and U-cast, we preferred to go for U-cast as our experience in this case was different and we preferred to provide better stability of fracture. A follow-up radiograph at 6 weeks showed signs of fracture union and the cast was replaced with a custom-made functional brace. Although 6 weeks of U-cast can lead to joint stiffness, in our case, the prime objective was to achieve union of the fracture. Shoulder and elbow joint mobilization was started. A review radiograph after 12 weeks showed union of the stress fracture at the plate end and visible callus at the primary fracture site (Fig. 5). At 9-month postoperatively, en bloc pull-out of the locking plate was noticed in the distal fragment of the fracture (Fig. 6). The limb was further immobilized in an arm sling for 4 weeks. At 1 year, the limb was painless, had a sense of improved strength in her arm, and had an acceptable range of shoulder movement (Fig. 7).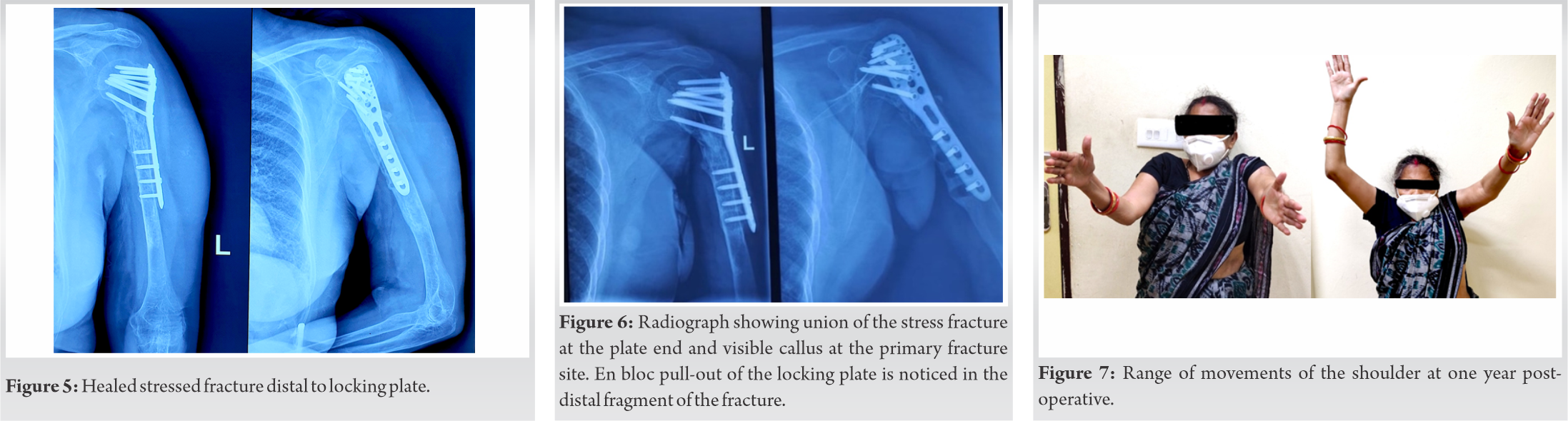
Osteoporotic fractures are often difficult to treat. There are multiple challenges both during conservative and surgical management of such fractures. In our case, we faced many challenges which may guide other surgeons in the planning and management of such a case. As the patient was on long standing steroids, our pre-operative osteoporotic management did not reflect a significant change in the bone quality of the patient. We were able to cut the fibula with a scissor. Reduction of fracture was a challenge and we did not find our routine method of fracture reduction to be helpful in such an osteoporotic bone. The reduction bone clamps needed to be applied gently to prevent any iatrogenic fractures. Intra-operative fluoroscopy as a guide for estimating screw length was not very reliable considering the poor radiopacity of the osteoporotic bones. Hence, other alternative methods like using a needle or a spike to demarcate the joint line in fluoroscopy or using the tactile feedback of a depth gauze need to be considered. Even in normal bone, there are complications as high as 35% due to primary and secondary screw perforations into the glenohumeral joint. In our case as the humerus head was poorly visible under fluoroscopy, there was a high chance of screw perforation to glenohumeral joint [5]. In porotic bones, complications related to fracture fixation can be as high as 40% [6]. Screw pull-out is dependent on bone mineral density which is markedly affected in osteoporosis [7]. Locking plates may minimize implant-related complications such as screw loosening and backout. The use of augmented fixation with biocomposites to fill the void may decrease the chance of screw loosening. Utilization of strut grafts similar to the presented case may improve fracture fixation and decrease implant loosening, but due to the generalized osteoporosis, our strut graft was porotic as well [8]. Although we used a locking plate, we could not eliminate complications such as peri-implant fracture and screw loosening. We had a screw loosening and backout evident at 9-month post-operation. A minimal pull-out not endangering fracture union can be managed conservatively by immobilization. It is known from epidemiological studies that neglected osteoporosis significantly increases the risk for a second fracture [9]. Hence, post-operative rehabilitation needs to be judiciously planned to prevent any further stress fracture at the plate ends. Although various in vitro studies support poor anchorage of implants to osteoporotic bones, still there is a lack of clinical evidence [10]. In our case, it was very evident that porotic bones have poor strength; as we were able to insert screws without pre-drilling, cut the bone with the help of scissors, presence of fracture at implant bone junction, and loosening noticed with backout of screws.
Management of fractures in osteoporotic bones requires stable fixation besides management of osteoporosis. Strut graft definitely adds to the stability and better implant purchase. Although we could not achieve stable fixation, a resultant stable fixation allows early mobilization of the limb and promotes return of muscle power. Correction of osteoporosis will prevent implant loosening and backout of screws. Hence, a careful pre-operative planning, active osteoporosis management, good implant selection, careful bone handling, and judicious rehabilitation are key to avoid complications and achieve a good functional outcome.
Osteoporotic fractures are challenging to treat. Complications can be encountered at any step. Aggressive osteoporotic management before attempting fixation is advisable and may prevent intra-operative and post-operative fixation failure.
References
- 1.Hollensteiner M, Sandriesser S, Bliven E, Rüden CV, Augat P. Biomechanics of osteoporotic fracture fixation. Curr Osteoporos Rep 2019;17:363-74. [Google Scholar]
- 2.Rüden CV, Augat P. Failure of fracture fixation in osteoporotic bone. Injury 2016;47:3-10. [Google Scholar]
- 3.Marongiu G, Mastio M, Capone A. Current options to surgical treatment in osteoporotic fractures. Aging Clin Exp Res 2013;25:15-7. [Google Scholar]
- 4.Marecek G, Centomo H. Augmented fixation for fractures of the appendicular skeleton. J Am Acad Orthop Surg 2019;27:823-33. [Google Scholar]
- 5.Brunner F, Sommer C, Bahrs C, Heuwinkel R, Hafner C, Rillmann P, et al. Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: A prospective multicenter analysis. J Orthop Trauma 2009;23:163-72. [Google Scholar]
- 6.Goldhahn S, Kralinger F, Rikli D, Marentet M, Goldhahn J. Does osteoporosis increase complication risk in surgical fracture treatment? A protocol combining new endpoints for two prospective multicentre open cohort studies. BMC Musculoskelet Disord 2010;11:256. [Google Scholar]
- 7.Seebeck J, Goldhahn J, Städele H, Messmer P, Morlock MM, Schneider E. Effect of cortical thickness and cancellous bone density on the holding strength of internal fixator screws. J Orthop Res 2004;22:1237-42. [Google Scholar]
- 8.Hsiao CK, Tsai YJ, Yen CY, Lee CH, Yang TY, Tu YK. Intramedullary cortical bone strut improves the cyclic stability of osteoporotic proximal humeral fractures. BMC Musculoskelet Disord 2017;18:64. [Google Scholar]
- 9.Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, et al. A meta-analysis of previous fracture and subsequent fracture risk. Bone 2004;35:375-82. [Google Scholar]
- 10.Goldhahn J, Suhm N, Goldhahn S, Blauth M, Hanson B. Influence of osteoporosis on fracture fixation-a systematic literature review. Osteoporos Int 2008;19:761-72. [Google Scholar]









