A hip dislocation during pregnancy can be managed by careful attempt of closed reduction. Pelvic fractures must be reduced anatomically to avoid complications during labor.
Dr. Divya Tomer, Department of Orthopaedics, Byramjee Jeejeebhoy Government Medical College and Sassoon General Hospital, Pune, Maharashtra, India. E-mail: tomerdivya@gmail.com
Introduction: Trauma is the leading non-obstetric cause of maternal mortality during pregnancy and pelvic fractures are challenging to manage in such cases due to the effect of trauma on the gravid uterus and altered maternal physiology. About 8–16% of pregnant females can have fatal outcome after trauma, with pelvic fractures contributing majorly to the same, and also can have severe fetomaternal complications. There are only two cases reported till date of hip dislocation in pregnancy, with very little literature available on its outcome.
Case Report: We, hereby, present a case of a 40-year-old pregnant female hit by a moving car with the right superior and inferior pubic rami fracture and left anterior hip dislocation. Closed reduction of the left hip was done under anesthesia and pubic rami fractures were managed conservatively. On follow-up after 3 months, the fracture was completely healed and the patient had a normal vaginal delivery. We have also reviewed management protocols for such cases. Aggressive maternal resuscitation is important for both maternal and fetal survival. Pelvic fractures should not be left unreduced in such cases to prevent mechanical dystocia and can have a good outcome with both closed and open reduction and fixation techniques.
Conclusion: Pelvic fractures in pregnancy should be treated by careful maternal resuscitation and timely intervention. The majority of such patients can deliver vaginally if the fracture heals before delivery.
Keywords: Pelvic fractures in pregnancy, hip dislocation in pregnancy, trauma in pregnancy, acetabular plating, open reduction internal fixation in pregnancy.
Trauma is the most common non-obstetric cause of maternal mortality and accounts for 46% of all maternal deaths [1, 2]. About 6–7% of all pregnant women suffer from road traffic accidents. In such cases, the maternal mortality rate is 8–16% and the fetal mortality rate can be as high as 35–57% [3, 4]. Out of all the causes of death in trauma cases in pregnancy, pelvic trauma is more dangerous due to changes in maternal physiology which lead, to delay in diagnosis and treatment [3]. Up to 30% of blood loss can go undetected due to maternal hemodilution and cause further diagnostic delay. Complications such as hemorrhagic shock due to massive hemorrhage, coagulopathy, rhesus isoimmunization, abruptio placentae, uterine rupture, premature delivery, fetal distress, Intrauterine fetal deaths, and urethral/perineal injuries are common [3]. Pelvic fractures in pregnancy are challenging to manage because hemorrhage from many dilated venous tributaries can cause significant retroplacental hemorrhage which can go undetected if not suspected and properly investigated. Along with pelvic fractures, concomitant abdominal injuries were present in 42% of cases, thorax in 25%, closed head injury in 37%, and other bones in 48% [4]. Hence, management of such injuries requires an interdisciplinary team approach and knowledge of advanced trauma management protocols. Furthermore, care must be taken to prevent future deleterious effects on the fetus by careful use of ionizing radiation, antibiotics, and anticoagulation. To the best of our knowledge, there are only two cases reported till date of hip dislocation in pregnancy, one managed by closed reduction, and the other one treated by open reduction of hip and acetabular plating [5, 6]. We, hereby, present a case of hip dislocation with contralateral pubic rami fracture, to highlight the challenges that we faced and discuss the rationale of our management, and also review the literature present for the same.
A 40-year-old pregnant female, who was walking on the road was hit by a moving car. She was brought to the emergency room 2 h later, with a history of trauma to the pelvis. She was conscious and oriented, with a GCS of 15. She was vitally stable and did not report head, neck, chest, or abdominal trauma. On examination, her left lower limb was in flexion, abduction, and external rotation. The range of motion was restricted and painful. She also had tenderness bilaterally on the pelvic compression test. There was no distal neurovascular deficit in the lower limbs.
On obstetric examination, she had no per vaginal discharge, nor any abdominal tenderness or contractions with normal fetal heart sounds. On USG FAST, she had no free fluid in abdomen and pelvis and on obstetric scan gestational age was found to be 26 weeks. On Doppler ultrasound, fetal heart rate was normal and cardiotocography was also normal. A collective decision was taken to get a single anteroposterior radiograph of the pelvis with both hips done, on which the left anterior hip dislocation and right superior and inferior pubic rami fractures were detected (Fig. 1). The patient was posted for closed reduction of hip dislocation under spinal anesthesia, which was successfully performed by hip extension, longitudinal in-line traction, and external rotation; all the while having an obstetrics team in the operating room. The concentric reduction was achieved which was confirmed radiographically (Fig. 2). Fetal cardiotocography was continuously done for 4 h which was normal. She was observed for 48 h and, then, discharged and advised bed rest for one month. In-bed exercises and physiotherapy were taught to prevent venous thromboembolism. The patient came walking to outpatient department at 38 weeks of gestation without any pain in the hip and had a normal vaginal delivery. She delivered a full-term normal female child. At 1 year follow-up, the patient was asymptomatic and was performing all activities of daily living with ease. The child was also growing with normal milestones.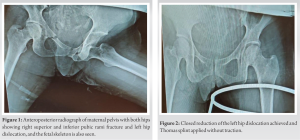
Pregnant patients suffering from major trauma require thorough examination and resuscitation, due to their unique physiology and the dependence of the fetus on maternal survival. Understanding these maternal physiological changes are thus important to prevent delay in diagnosis and to improve the outcome of the patient’s condition. Due to physiological hemodilution and compression of Inferior vena cava by the gravid uterus, cardiovascular response to shock can be blunted [6]. Hence, close hemodynamic monitoring is required, as causes like retroperitoneal hemorrhage may not be readily apparent and can cause severe hemodynamic instability before getting recognized. Furthermore, the presence of a fetus can be distracting to health-care providers, and if a standard treatment protocol is not followed, mismanagement can lead to catastrophic results [7]. Aggressive maternal resuscitation and stabilization as per advanced trauma life support (ATLS) protocol should be started, to save both the mother and the fetus [8]. Pelvic fractures, if suspected, necessitate radiographic confirmation for further management. One pelvis radiograph exposes the patient to 200 miliRad radiation, and one Computed tomography scan exposes to 1.5 Rad. According to the American College of obstetrics and gynecology guidelines, up to 5 Rad exposure is considered safe in pregnancy to prevent congenital anomalies, growth restriction, and gene line mutation [1, 9]. Therefore, limited radiological investigations are safe to be done if maternal injuries are suspected, especially in the last trimester.
Closed or open reduction of these cases presents further difficulty due to risks associated with anesthesia in pregnancy. The use of general anesthesia may have increased the risk of spontaneous abortion in the first or second trimester [10]. The use of regional anesthesia/local anesthesia is preferred to prevent effects on the uterus and fetus [2]. Hip dislocation in pregnancy is a rare injury [5, 6]. However, pregnant women are probably at higher risk of this injury due to intrinsically lax ligaments during the third trimester due to the effects of hormones such as relaxin. Furthermore, pregnant women are often seated without the restraint of a seatbelt due to fear of compression of the gravid uterus which, further, increases the risk of severe pelvic fractures and hip dislocations in high-speed motor vehicular collisions [5]. If these fractures are untreated, it may lead to mechanical dystocia due to malunion of unreduced fracture resulting in an unsymmetrical pelvis [3]. Following pelvic fractures, whether or not natural childbirth can happen or not is often asked by both patients and clinicians. Studies have shown that a pelvic fracture is not a definite contraindication for vaginal delivery. However, a severe dislocated/unstable fracture with a large healing callus precludes an attempt at vaginal delivery. Leggon et al., in their study, showed results of 75% cases of pelvic fractures in the third trimester of pregnancy delivered by vaginal birth out of 101 cases of pelvic fractures in pregnancy [11]. If the fetus is not affected and the mother is also hemodynamically stable, fixation of pelvic fracture can be done with an acceptable level of fetal risk [12]. Until 2001, surgery on pelvic or acetabular fractures in pregnant patients was reported only in four published cases [13] Surgery was only used in cases of postpartum diastasis [14]. In those cases, with conservative management the reduction was rarely anatomical, with the possible formation of birth canal deformities with residual displacements being painful. Increased length of hospital stay and complications such as infections, thromboembolism, and decubitus ulcers was also common. Hence, they preferred to be surgically treated [14]. Similar indications can be thought to be pertinent for traumatic pelvic fractures in pregnancy, and hence, their surgical management becomes important to prevent long-term morbidity. Percutaneous fixation of the sacroiliac joint with screws under fluoroscopic control can expose the fetus to some amount of radiation. Porter et al. repaired eight acetabular fractures of pregnant patients and concluded that the use of radiographic images during surgical treatment, with minimum risk to the baby, could be used in an attempt to obtain acceptable articular reduction [12]. Rudloff performed acetabular ORIF in ten out of 12 patients with pelvic trauma in pregnancy with good outcomes [4]. Loegters et al. performed ORIF in unstable pelvic ring (vertical shear) injury in prone position with minimal use of fluoroscopy and reported good outcome [15]. Similarly, ORIF of unstable pelvic fractures in four pregnant patients with a mean gestational age of 23 weeks were done by Schwartsman et al. [16]. Two women had Malgaigne-type fractures and the other two had symphyseal disjunction associated with acetabular fractures. They showed that good evolution of pregnancy with the union of fracture was only possible with careful pre-, peri-, and post-operative care for the mother, as well as fetal assessment by a multidisciplinary team [16]. Young et al. performed ORIF for combined acetabulum fracture and hip dislocation in an 18-year-old female at 35 weeks of gestation [6]. Charnell et al. performed delivery as well as acetabular plating in the same sitting using the incision used for cesarean delivery and converting it to an extended ilioinguinal approach for anterior acetabular plating [17]. The management of pregnant patients with orthopedic injuries was called “Orthostetrics” by Matthews et al. They too emphasized that operative timing, imaging, and medication selection are factors that may vary based on trimester and clinical scenario. Thus, pregnant patients present a distinct challenge to the orthopedic surgeon in that the well-being of two patients must be considered in all steps of care [18]. The successful outcome of these injuries depends on multidisciplinary team-based management. Furthermore, safe methods for reduction of hip dislocation in pregnancy that do not increase the intra-abdominal pressure need to be identified. Long-term follow-up of these mothers and developmental disorders in these children need to be studied further.
The management of pelvic ring and/or acetabular fractures or hip dislocation in pregnant patients is based on patient-specific risk-benefit analysis and shared decision-making. It requires an interdisciplinary approach and strict adherence to ATLS principles. The best shot of fetal survival is maternal stabilization. If fetal distress can be ruled out, then, the management of pelvic fractures remains the same as for women who are not pregnant and have the same outcome. The outcome of pregnancy also remains favorable if the fracture heals before the time of delivery. Very displaced fractures preclude attempts of vaginal delivery and may cause mechanical dystocia with cesarean section being employed for such cases, followed by open reduction and internal fixation of the fracture in the same sitting or later. Overall favorable outcomes of both pregnancy and fracture can be achieved if managed properly.
It is important to manage pelvic fractures and hip dislocation during pregnancy with utmost urgency by following ATLS principles, and perform open or closed reduction to prevent mechanical dystocia.
References
- 1.Mirza FG, Devine PC, Gaddipati S. Trauma in pregnancy: A systematic approach. Am J Perinatol 2010;27:579-86. [Google Scholar]
- 2.Tejwani N, Klifto K, Looze C, Klifto CS. Treatment of pregnant patients with orthopaedic trauma. J Am Acad Orthop Surg 2017;25:e90-101. [Google Scholar]
- 3.Occelli B, Depret-Mosser S, Renault B, Therby D, Codaccioni X, Monnier JC. Pelvic trauma and pregnancy. Literature review and case report. Contracept Fertil Sex 1998;26:869-75. [Google Scholar]
- 4.Rudloff U. Trauma in pregnancy. Arch Gynecol Obstet 2007;276:101-17. [Google Scholar]
- 5.Kamarul T, Loh WY. Traumatic hip dislocation in late pregnancy: A case report. Med J Malaysia 2005;60 Suppl C:114-6. [Google Scholar]
- 6.Young JR, Vignaly L, Carroll J, Ross P, Mori BV, Czajka CM. Combined acetabulum fracture and hip dislocation in an 18-year-old female at 35-week gestation: A case report and review of the literature. Case Rep Orthop 2020;2020:8888015. [Google Scholar]
- 7.Flik K, Kloen P, Toro JB, Urmey W, Nijhuis JG, Helfet DL. Orthopaedic trauma in the pregnant patient. J Am Acad Orthop Surg 2006;14:175-82. [Google Scholar]
- 8.Timberlake GA, McSwain NE Jr. Trauma in pregnancy. A 10-year perspective. Am Surg 1989;55:151-3. [Google Scholar]
- 9.ACOG educational bulletin. Obstetric aspects of trauma management. Number 251, September 1998 (replaces Number 151, January 1991, and Number 161, November 1991). American college of obstetricians and gynaecologists. Int J Gynecol Obstet 1999;64:87-94. [Google Scholar]
- 10.Duncan PG, Pope WD, Cohen MM, Greer N. Fetal risk of anesthesia and surgery during pregnancy. Anesthesiology 1986;64:790-4. [Google Scholar]
- 11.Leggon RE, Wood GC, Indeck MC. Pelvic fractures in pregnancy: Factors influencing maternal and fetal outcomes. J Trauma 2002;53:796-804. [Google Scholar]
- 12.Porter SE, Russell GV, Qin Z, Graves ML. Operative fixation of acetabular fractures in the pregnant patient. J Orthop Trauma 2008;22:508-16. [Google Scholar]
- 13.Kloen P, Flik K, Helfet DL. Operative treatment of acetabular fracture during pregnancy: A case report. Arch Orthop Trauma Surg 2005;125:209-12. [Google Scholar]
- 14.Webb LX, Gristina AG, Wilson JR, Rhyne AL, Meredith JH, Hansen ST Jr. Two-hole plate fixation for traumatic symphysis pubis diastasis. J Trauma 1988;28:813-7. [Google Scholar]
- 15.Loegters T, Briem D, Gatzka C, Linhart W, Begemann PG, Rueger JM, et al. Treatment of unstable fractures of the pelvic ring in pregnancy. Arch Orthop Trauma Surg 2005;125:204-8. [Google Scholar]
- 16.Schwartsmann CR, Macedo CA, Galia CR, Miranda RH, Spinelli LF, Ferreira MT. Update on open reduction and internal fixation of unstable pelvic fractures during pregnancy: Case reports. Rev Bras Ortop 2018;53:118-24. [Google Scholar]
- 17.Charnell AM, Ferriman E, Dimitriou R, Panteli M, Giannoudis PV. Combined caesarean section and open reduction internal fixation for the treatment of an acetabular fracture in late pregnancy. JRSM Open 2018;9:2054270417732698. [Google Scholar]
- 18.Matthews LJ, McConda DB, Lalli TA, Daffner SD. Orthostetrics. Management of orthopedic conditions in the pregnant patient. Orthopedics 2015;38:e874-80. [Google Scholar]









