For cases presenting with unusual features, radiological investigation (Magnetic resonance imaging) and histopathological examination of excised specimen are of utmost importance for proper diagnosis and treatment.
Dr. Nandlal Bharwani, Room. No 637, PG Family Hostel, Dr. SN Medical College, Jodhpur, Rajasthan, India. E-mail: nandlalbharwani21@gmail.com
Introduction: Mycetoma is a form of chronic granulomatous disease which involves subcutaneous tissues and causes bone destruction in advanced stages. The characteristic features are sinus formation, granules formation, and mass in subcutaneous region.
Case Report: A 19-year-old male presented to our out-patient clinic with complaint of a painless swelling around the medial aspect of the right knee joint for 8 months with no sinus or discharge of granules. Pes anserinus bursitis was thought of as differential diagnosis for the present condition. “Staging-classification of mycetoma” is commonly used for classifying mycetoma and as per classification, the present case had Stage-A.
Conclusion: Single-stage local excision was performed and supplemented with anti-fungal agent for 6 months, which showed good outcome at the final follow-up of 13 months.
Keywords: Eumycetoma, wide excision, antifungal agents, knee.
It is commonly known as madura foot and maduramycosis [1]. Mycetoma is a form of chronic granulomatous disease which involves subcutaneous tissue and causes bone destruction in advanced stages [2]. The characteristic features are sinus formation, granules formation, and mass in subcutaneous region. Two types of mycetoma are commonly encountered: Eumycetoma (fungi) and actinomycetoma (bacteria) [2]. The most commonly affected part is foot, although mycetoma can affect any body part with slight male predominance (3-4:1) [3, 4]. Proper clinical history, investigations like ultrasound, magnetic resonance imaging, and fine-needle aspiration along with histopathological examination are of utmost importance for management of mycetoma. Causative agent, extent of disease, and location are of utmost importance for surgical planning and predicting the outcome. The treatment of choice for these cases is medical management and wide surgical excision[5, 6]. If not managed properly, it can lead to severe tissue destruction, secondary bacterial infections, deformities of limb, and other dreaded complications. Till date, very few literatures on such unusual presentation of mycetoma around knee joint are available.
A 19-year-old male presented to our outpatient clinic with complaint of a painless swelling around medial aspect of the right knee for 8 months with no sinus or discharge of granules, and pesanserinus bursitis was thought of as differential diagnosis for the present condition. Proper history and clinical examination showed no restriction of movement around knee. Hematological and digital radiographs were performed, but none of them were conclusive. Therefore, magnetic resonance imaging of knee joint (Fig. 1-3) was performed and it showed an ill-defined proton density fat-suppressed hyperintense mass lesion in the subcutaneous plane of the medial aspect of knee joint but not extending deep to the deep fascia. The lesion also demonstrated an oval hyperintensity with possible central hypointensities giving “dot-in-circle” sign.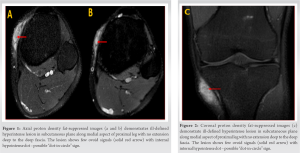 “Staging-classification of mycetoma” is commonly used for classifying mycetoma and as per classification, the present case had Stage-A.
“Staging-classification of mycetoma” is commonly used for classifying mycetoma and as per classification, the present case had Stage-A.
Stage description:
A – No sinuses only swelling
B – Sinuses/pustules formation with woody induration
C – Digital radiograph showed bony involvement
D – Multiple lesions/spreading to distant sites.
Proper informed consent was taken before taking the patient for surgical procedure. Therefore, excisional biopsy was planned. The patient was given neuraxial anaesthesia. With the patient lying supine on operating table, with tourniquet pressure 320 mmHg, 3–4 cm skin incision given on the medial aspect of knee. Intraoperatively, the pathology was present in subcutaneous plane. Complete excision was carried out, thorough wash was given and closure was performed in layers. Size of the excised tissue (Fig. 4) measured 4 ×2.5 × 1 cm and was sent for Gram’s staining, histopathological examination, and fungal culture. Histopathological examination (Fig. 5) showed multiple fungal colonies which were surrounded by inflammatory infiltrates which confirmed the diagnosis of mycetoma (Madurella mycetomatis), and fungal culture was also conclusive. Therefore, tablet itraconazole (200 mg, twice a day) was given for 6 months. Range of motion around knee joint was normal at the final follow-up. The patient was followed for 13 months postoperatively and the period was uneventful.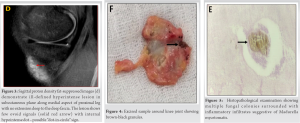
Mycetoma is a form of chronic disease with involvement of skin and subcutaneous tissue and, leading to bony destruction in the advanced stage of disease and if not managed properly, can lead to recurrence [2, 7]. This condition is usually seen in tropical regions such as India, Yemen, and Mexico, at a latitude of 30° north and 15° south. The case presented is from Western Rajasthan which is a very dry area and a knee joint infection by Madurella in this part of the country explains the rarity of condition. The incidence of this condition cannot be commented upon due to its delayed presentation in outpatient department. Usually, mycetoma presents with typical features, but in 10-15% patients, unusual presentation can be noted, as seen in present case.1 For such presentations, clinical history, local examination, and magnetic resonance imaging along with histopathological examination are key to diagnosis. For eumycetoma patients, gold standard treatment is anti-fungal drugs such as itraconazole or ketoconazole and wide local excision. The advantage of adding an anti-fungal agent to the treatment is that it reduces the burden of disease and reduces fibrous tissue formation around the lesion which leads to adequate excision of the lesion[8]. In various literatures, adequate margins for local excision are 0.5-2 cm, but nothing is well defined till date [9, 10]. For present case, local excision was done and tablet itraconazole (200 mg, twice a day) was given for 6 months. It was chosen over ketoconazole as it is less hepatotoxic.
hepatotoxic.
The case presented with painless swelling around medial aspect of knee and was diagnosed as Stage-A mycetoma as per the “Staging classification of mycetoma.” Madurella mycetomatis was the organism isolated. A single-staged wide local excision was performed and supplemented with anti-fungal agent for 6 months, which showed good outcome at its final follow-up of 13 months.
For cases presenting with unusual features, radiological investigation ( Magnetic resonance imaging) and histo-pathological examination of excised specimen is of utmost importance for proper diagnosis and treatment.
References
- 1.Suneet S, Anurag K, editors. Surgical Diseases in Tropical Countries. New Delhi, India: Jaypee Brothers; 1996. [Google Scholar]
- 2.Baki R, Mathur DR. Incidence and changing pattern of Mycetoma in Western Rajasthan. Indian J Pathol Microbiol 2008;51:154-5. [Google Scholar]
- 3.Mahgoob ES. Mycetoma. In: Gurrent RL, Walker DH, Weller PF, editors. Tropical Infectious Diseases: Principles, Pathogens and Practice. 1st ed. New York: Churchill Livingstone; 2000. p. 616-20. [Google Scholar]
- 4.Welsh O, Vera-Cabrera L, Salinas-Carmona MC. Mycetoma. Clin Dermatol 2007;25:195-202. [Google Scholar]
- 5.Fahal AH. Management of mycetoma. Expert Rev Dermatol 2010;5:87-93. [Google Scholar]
- 6.Fahal AH. Mycetoma thorn on the flesh. Trans R Soc Trop Med Hyg 2004;98:3-11. [Google Scholar]
- 7.Rajkumar SA, Angamuthu N. Multiple foot sinues due to schizomycetes. Indian J Orthop 2005;39:125-6. [Google Scholar]
- 8.Suleiman SH, Wadella ES, Fahal AH. The surgical treatment of my cetoma. PLoS Negl Trop Dis 2016;10:e0004690. [Google Scholar]
- 9.Tamir G, Adler A, Hagler DJ, Goldberg I. Mycetoma of the foot-surgical treatment with free flap reconstruction. Eur J Plast Surg 1995;18:124-6. [Google Scholar]
- 10.Gismalla MD, Abdulla GM, Ali MM, Mohamed SM. Wide surgical and reconstruction of eumycetoma in Gezira Mycetoma Centre. Glob J Med 2016;16:14-7. [Google Scholar]











