Morel-Lavallée lesion caused by partial degloving injury is best diagnosed by MRI of the limb followed by evacuation, irrigation with 3% hypertonic saline as a sclerosant followed by closed suction drainage.
Dr. Ketan Vagholkar, Department of Surgery, D. Y. Patil University School of Medicine, Navi Mumbai, Maharashtra, India. E-mail: kvagholkar@yahoo.com
Introduction: Morel-Lavalleé lesion is an uncommon closed degloving injury usually affecting the lower extremity. Although these lesions have been documented in literature, yet there is no standard treatment algorithm for the same. A case of Morel-Lavallée lesion following blunt injury to the thigh is therefore presented to highlight the diagnostic and therapeutic challenges in managing such lesions. The aim of presenting the case is to create awareness of clinical presentation, diagnosis, and management of Morel-Lavallée lesions, especially in the setting of polytrauma patients.
Case Report: A case of Morel-Lavallée lesion in a 32-year-old male with history of a blunt injury to the right thigh caused by a partial run over accident is presented. A magnetic resonance imaging (MRI) was done to confirm the diagnosis. A limited open approach for evacuating the fluid in the lesion was performed followed by irrigation of the cavity with a combination of 3% hypertonic saline and hydrogen peroxide in order to induce fibrosis to obliterate the dead space. This was followed by continuous negative suction accompanied with a pressure bandage.
Conclusion: A high index of suspicion is necessary especially in cases of severe blunt injuries to the extremities. MRI is essential for early diagnosis of Morel-Lavallée lesions. A limited open approach is a safe and effective option for treatment. The use of 3% hypertonic saline along with hydrogen peroxide irrigation of the cavity to induce sclerosis is a novel method for treating the condition.
Keywords: Morel-Lavallée lesion, diagnosis, management.
The Morel-Lavallée lesion is a closed degloving injury involving the soft tissues of the extremities [1]. It is usually caused by blunt high energy trauma. The thigh, hip, and pelvic region are particularly predisposed to such lesions. Morel-Lavallae was first described by Victor Auguste Morel-Lavallée in 1863 [1]. Although the lesion has typical characteristics, there is not an abundance of information on the issue. Awareness of this lesion, especially in trauma patients is essential for early diagnosis and prompt treatment. A case of Morel-Lavallée lesion is presented in order to highlight clinical features, the role of imaging, and the various surgical options available for treating this lesion.
A 32-year-old man presented with a history of blunt injury to the thigh following a vehicular accident. The patient was admitted to a peripheral hospital where he was treated for the injury to the thigh. The patient was treated for superficial abrasions over the thigh as well as for the shocked state. There was no evidence of any fracture of the pelvis, hip, and femur on the right side. The patient developed a swelling which was attributed to be a hematoma by the initial treating doctor. He was discharged from hospital after 1 week. Subsequently, the patient noticed an increase in the diameter of the injured thigh over the next 2 weeks. The swelling extended from the anterior superior iliac spine to the right knee joint. The patient was unable to move the right knee joint due to the swelling. He was advised to continue conservative treatment. However, as there was no change in the size of the swelling, he was referred to our facility. On examination, the vital parameters were within normal limits. Local examination of the right lower extremity revealed a massively enlarged thigh with the mid-thigh circumference of 82 cm as compared with a mid-thigh circumference of 59 cm of the normal left thigh. The swelling was predominantly occupying the anterior-lateral aspect of the thigh and was fluctuant. It extended from the groin to the lateral aspect of the right knee (Fig. 1).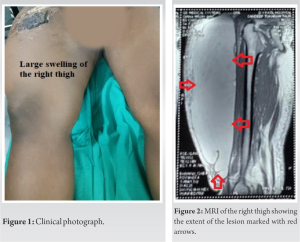 All laboratory investigations were within the normal range. A magnetic resonance imaging (MRI) of the right lower extremity was done, which showed a large extensive cystic swelling between the hypodermis and the deep fascia of the thigh. It had a distinct pseudo capsule (Fig. 2). The deeper muscular compartment was normal (Fig. 3). With the help of an ultrasound, the most dependent part of the swelling was identified. A longitudinal, 7 cm incision was marked under ultrasound guidance. Under regional anesthesia, the entire cystic swelling was drained. Approximately, 4 L of serosanguinous (altered blood) fluid was drained through the incision. A rigorous lavage with 300 cc of 3% hypertonic saline with 3 cc of hydrogen peroxide was given to ensure removal of all tissue debris consisting of semi liquefied fat from the cyst cavity. Hypertonic saline also serves as a sclerosing agent aiding in obliteration of the dead space. Two negative suction drains (16 French size) were placed in the cavity and brought out through separate incisions. The incision was closed in 2 layers (Fig. 4).
All laboratory investigations were within the normal range. A magnetic resonance imaging (MRI) of the right lower extremity was done, which showed a large extensive cystic swelling between the hypodermis and the deep fascia of the thigh. It had a distinct pseudo capsule (Fig. 2). The deeper muscular compartment was normal (Fig. 3). With the help of an ultrasound, the most dependent part of the swelling was identified. A longitudinal, 7 cm incision was marked under ultrasound guidance. Under regional anesthesia, the entire cystic swelling was drained. Approximately, 4 L of serosanguinous (altered blood) fluid was drained through the incision. A rigorous lavage with 300 cc of 3% hypertonic saline with 3 cc of hydrogen peroxide was given to ensure removal of all tissue debris consisting of semi liquefied fat from the cyst cavity. Hypertonic saline also serves as a sclerosing agent aiding in obliteration of the dead space. Two negative suction drains (16 French size) were placed in the cavity and brought out through separate incisions. The incision was closed in 2 layers (Fig. 4). 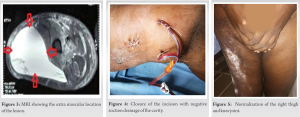 A firm pressure bandage was applied in order to obliterate the dead space. The tube drains were removed on the 18th post-operative day after ensuring that the daily drain tube output was less than 20 CC on 2 consecutive days. Suture removal was done on the 14th post-operative day. The patient has been following up for the last 6 weeks with no evidence of recurrence and normalization of the right thigh circumference and right knee movements (Fig. 5).
A firm pressure bandage was applied in order to obliterate the dead space. The tube drains were removed on the 18th post-operative day after ensuring that the daily drain tube output was less than 20 CC on 2 consecutive days. Suture removal was done on the 14th post-operative day. The patient has been following up for the last 6 weeks with no evidence of recurrence and normalization of the right thigh circumference and right knee movements (Fig. 5).
Morel-Lavallée lesion is a closed soft tissue degloving injury associated with high impact trauma [1]. It has particular predilection for the thigh, hip, and pelvic region [2]. Tangential force applied to the skeletal soft tissue envelope leads to severe shearing stress. This causes separation of the skin and subcutaneous tissues from the deep fascia of the thigh. A potential dead space is therefore created. Damage to the vasculature and lymphatics at this level lead to collection of blood, serosanguinous fluid, and necrotic fat. Inflammatory and metabolic product in the fluid stimulates cellular permeability and enhanced leakage from the vessels and lymphatics into the potential space created. This self-propagating cycle is responsible for continued enlargement of the swelling as was seen in the case presented. The fluid contains blood clots, fibrin, normal, and necrotic fat [2, 3]. With time, there is a high likelihood of bacterial contamination, eventually leading to ischemic necrosis of the overlying skin and subcutaneous tissues. If left untreated, local inflammation leads to the formation of a pseudo capsule and maturation of this fibrous capsule leads to a well-formed fluid-filled space. The predilection for the hip and thigh region is due to increased laxity of the skin in the area along with the presence of a dense capillary network. Morel-Lavallée lesion is an independent risk factor for the development of postoperative surgical site infection, especially in those patients who are undergoing pelvic stabilizing surgery. The lesion is overlooked in the early stages immediately following trauma and is usually attributed to a hematoma. Hence, in majority of cases, conservative treatment is resorted to in the initial phase and as seen in the case presented. Any high impact blunt trauma to the lower extremity followed by the development of large swelling should raise the suspicion of an impending Morel-Lavallée lesion. Imaging plays a pivotal role in the diagnosis of this lesion. MRI is the best investigation for diagnosis as compared to ultrasound and CT scan [4]. MRI reveals homogeneously hypointense images in T1-weighted sequences whereas hyperintense images are seen in T2-weighted images. These lesions will also appear homogeneously bright. On both T1- and T2-weighted sequences which is a reflection of high internal concentration of meth hemoglobin, the signal intensities on T1- and T2-weighted images vary depending on the age of the hematoma. T1- and T2-weighted images will reveal a hypointense peripheral ring representing hemosiderin and fibrous tissue seen in chronic lesions [4, 5]. Post-contrast images may show patchy enhancement in both internal and peripheral regions of the lesion consistent with an organizing hematoma. Various modalities of treatment have been advocated [1, 6, 7]. The choice of treatment depends on the site and size of the lesion. Proximity to an intended surgical incision for treating a coexisting injury is also an important determinant for an optimal choice of treatment. Formal open debridement has been advocated in the majority of cases. However, there is a high likelihood that it may compromise the subdermal vascular layer which supplies the skin and superficial tissues thereby leading to necrosis [2, 8]. A more limited open approach is an excellent option as was adopted in the case presented [2, 3, 9]. Ultrasound guided marking of the skin incision at the most dependent part ensures precise and complete evacuation of the fluid as well as necrotic tissue debris in the lesion. It also helps in copious irrigation of the cavity. In the case presented, initial irrigation was done with dilute solution of hydrogen peroxide in saline followed by irrigation with 3% hypertonic saline. About 3% hypertonic saline, it is a sclerosing agent and helps in obliteration of the dead space. Negative suction tube drains with super added compression dressing are essential to drain all possible fluid accumulating subsequently until the dead space is completely obliterated. The time frame for removal of the drains is variable and is dictated by the output. A daily drain output of <30 CC per 24 h for 2 consecutive days provides a safe indication for drain removal. Serial needle aspiration with injection of talc or doxycycline is another alternative [2, 3, 10]. However, serial aspiration enhances the risk of infection.
Morel-Lavallée is a unique and uncommon form of closed degloving injury usually affecting the lower extremity.
Development of a massive swelling should raise a doubt of Morel-Lavallée lesion. MRI is a radiological investigation of choice for Morel-Lavallée lesions. A limited open approach with evacuation of fluid and debris, irrigation with a combination of 3% hypertonic saline and hydrogen peroxide followed by a closed suction drainage of cavity with compression dressing is an effective and safest therapeutic approach for this lesion.
Morel-Lavallée lesion is an uncommon post traumatic lesion necessitating awareness to avoid misdiagnosis thereby causing delay in treatment. MRI of the affected limb is diagnostic. Limited open drainage and evacuation followed by vacuum drainage of the cavity are therapeutic. The use of a combination of 3% hypertonic saline and hydrogen peroxide for irrigation of the cavity with a view to obliterate the cavity has not been described as yet and therefore is a novel method in treating this condition.
References
- 1.Bonilla-Yoon I, Masih S, Patel DB, White EA, Levine BD, Chow K, et al. The Morel-Lavallée lesion: Pathophysiology, clinical presentation, imaging features, and treatment options. Emerg Radiol 2014;21:35-43. [Google Scholar]
- 2.Greenhill D, Haydel C, Rehman S. Management of the Morel-Lavallée lesion. Orthop Clin North Am 2016;47:115-25. [Google Scholar]
- 3.Dawre S, Lamba S, Harinatha S, Gupta S, Gupta AK. The Morel-Lavalée lesion: A review and proposed algorithmic approach. Eur J Plast Surg 2012;35:489-94. [Google Scholar]
- 4.Mukherjee K, Perrin SM, Hughes PM. Morel-Lavallee lesion in an adolescent with ultrasound and MRI correlation. Skeletal Radiol 2007;36(Suppl 1):S43-5. [Google Scholar]
- 5.Volavc TS, Rupreht M. MRI of the Morel-Lavallée lesion-a case series. Radiol Oncol 2021;55:268-73. [Google Scholar]
- 6.Jalota L, Ukaigwe A, Jain S. Diagnosis and management of closed internal degloving injuries: The Morel-Lavallée lesion. J Emerg Med 2015;49:e1-4. [Google Scholar]
- 7.Powers ML, Hatem SF, Sundaram M. Morel-Lavallee lesion. Orthopedics 2007;30:322-3. [Google Scholar]
- 8.Boushnak MO, Rabah H, Saleh MH, Aaraj GA, Hajjar S, Moussa MK. Post-traumatic late presentation of Morel-Lavallée: Case report and review of literature. J Orthop Case Rep 2021;11:92-5. [Google Scholar]
- 9.Diviti S, Gupta N, Hooda K, Sharma K, Lo L. Morel-Lavallee lesions-review of pathophysiology, clinical findings, imaging findings and management. J Clin Diagn Res 2017;11:TE01-4. [Google Scholar]
- 10.Molina BJ, Ghazoul EN, Janis JE. Practical review of the comprehensive management of Morel-Lavallée lesions. Plast Reconstr Surg Glob Open 2021;9:e3850. [Google Scholar]






