The awareness of Baker's cyst causing rare consequences like combined tibial and peroneal nerve compression neuropathy along with a judicious strategy results in early diagnosis and prudent treatment, thereby preventing permanent impairment.
Dr. Surya Teja Malasani, Department of Orthopaedics, Saveetha Medical College, Chennai, Tamil Nadu, India. E-mail: surya.malasani@gmail.com
Introduction: Popliteal cysts (Baker cysts) causing compressive neuropathy of combined tibial and common peroneal nerves is an exceptional entity. Especially, an isolated multi-septate unruptured cyst (usually posteromedially) dissecting posterolaterally, thereby causing compression of multiple components of the popliteal neurovascular bundle as seen in this case report is unique in clinical field and in the literature. Awareness and early diagnosis of such cases along with a prudent technique will preclude permanent impairment.
Case Report: A 60-year-old man with a 5-year history of a symptomless popliteal mass in his right knee was hospitalized with aberrant gait and walking difficulty that had deteriorated during a 2-month period. The patient reported hypoesthesia across the sensory innervations of tibial and common peroneal nerves. Clinical examination indicated a prominent painless and unfixed cystic, fluctuant swelling extending around 10 × 7 cm in the popliteal fossa encroaching into the thigh. Motor examination showed decrease in the power of ankle dorsiflexion, plantar flexion as well as inversion and eversion of the foot resulted in progressive difficulty in walking with high stepping gait. The action potential amplitudes of the right peroneal and tibial compound muscles were dramatically decreased with a drop in motor conduction velocities and a prolonging of the F-response latencies, according to nerve conduction studies. Magnetic resonance imaging of the knee showed a multi septate popliteal cyst measuring 13.8*6.5*6.8 cm along the medial head of gastrocnemius, and the T2-weighted sagittal and axial sections revealed the cyst connecting with the right knee. He was planned and undergone open cyst excision with decompression of the peroneal and tibial nerves.
Conclusion: This exceptional case establishes that Baker’s cyst very rarely can cause compressive neuropathy vandalizing both the common peroneal and tibial nerves. Excision of the cyst by open technique along with neurolysis may be a more judicious and successful strategy for resolving symptoms quickly as well as to prevent permanent impairment.
Keywords: Baker cysts, compressive neuropathy, tibial and peroneal nerves, open cyst excision.
Popliteal cysts (Baker cysts) are a somewhat typical occurrence in people over the age of 50 who report with knee discomfort or knee pathologies that disrupt the synovial fluid dynamics, such as meniscal tears, arthritis, or, in rare cases, gout [1,2]. A 2004 prospective research on the origin of this cyst revealed that popliteal cysts often develop in the posteromedial popliteal fossa due to a deficient anatomic support in this location of the synovial capsule[3]. Fluid buildup inside the bursa in this region of the knee usually spares the posterolaterally situated neurovascular structures. The growing cyst may sporadically move posterolaterally and compress multiple components of the popliteal neurovascular structures (typically located posteromedially). Nerve entrapment symptoms that can occur include tibial or peroneal neuropathy, which causes foot drop, gastrocnemius muscle wasting, or, in unusual cases, combined tibial and common peroneal neuropathy. Syndromes associated with neurovascular structures compression include intraneural ganglion cysts of the lower branches of the sciatic nerve [4,5,6], deep vein thrombosis of the lower extremity causing thrombophlebitic syndrome, popliteal entrapment syndrome, knee joint synovial sarcoma, lower leg posterior region compartment syndrome, popliteal artery aneurysm, and Baker’s cyst.
A 60-year old man has presented to Arvindam hospital with complaints of a swelling in his right knee joint over the posterior aspect of his knee for 5 years associated with difficulty in walking for 2 months. The swelling was noticed 5 years back which was insidious in onset and asymptomatic at the time of presentation, had gradually increased, and reached the present size. However, he had started experiencing discomfort for 5 months in his right knee with progressive hypoesthesias across the skin of the anteromedial aspect of leg, as well as the sole of the foot, as well as the lateral leg and dorsum of the foot. In addition, he had progressive difficulty in walking with high stepping gait worsening over a 2-month period. Therefore, he was admitted for further evaluation and management. Clinical examination indicated a prominent painless and unfixed cystic, fluctuant swelling extending around 10 × 7 cm in the popliteal fossa encroaching into the thigh (Fig. 1).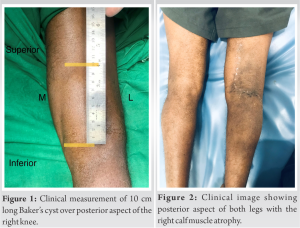 The cyst was noted to be compressible and unruptured with positive transillumination test. The left mid-calf circumference was 33 cm whereas that of the right calf was 30 cm, thus demonstrating atrophy of the right calf (Fig. 2).
The cyst was noted to be compressible and unruptured with positive transillumination test. The left mid-calf circumference was 33 cm whereas that of the right calf was 30 cm, thus demonstrating atrophy of the right calf (Fig. 2). 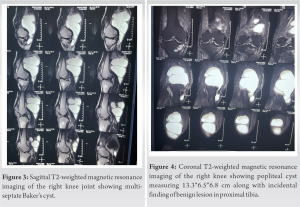 Neurological examination revealed decreased sensations to pin-prick and fine touch over the common peroneal and tibial nerve innervations. Motor examination showed Medical Research Council Grade-3 plantar flexion and Grade-1 dorsiflexion of the ankle joint as well as Grade-3 inversion with Grade-1 eversion of the foot were noticed.
Neurological examination revealed decreased sensations to pin-prick and fine touch over the common peroneal and tibial nerve innervations. Motor examination showed Medical Research Council Grade-3 plantar flexion and Grade-1 dorsiflexion of the ankle joint as well as Grade-3 inversion with Grade-1 eversion of the foot were noticed.
Initially, the patient underwent a lumbar spine magnetic resonance imaging (MRI) to rule out spinal disease, and radiographs of the knee as well as duplex ultrasonography of the right lower limb were confirmed to be normal; hence, a nerve conduction study (NCS) was done. The action potential amplitudes of the right peroneal and tibial compound muscles were dramatically decreased with a drop in motor conduction velocities and a prolonging of the F-response latencies, according to nerve conduction studies. The action potential amplitudes of the left tibial and peroneal complex muscles, on the other hand, were normal. An MRI of the right knee was requested. A multi septate popliteal cyst of 13.8*6.5*6.8 cm along the medial head of the gastrocnemius was seen in the T2-weighted sagittal image (Fig. 3), and the cyst communicated with the knee joint in the T2-weighted axial view (Figs. 4 and 5). 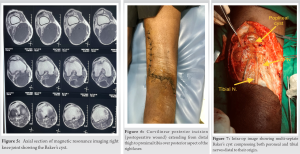 Therefore, he was planned for surgery after taking a written consent. The cyst was addressed through the posterior approach with a wide curvilinear incision with blunt dissection between the medial head of the gastrocnemius and semimembranosus muscles (Fig. 6). A massive multi-septate cyst measuring 13*6*6 cm was discovered, spanning from the distal thigh to the proximal tibia and obviously compressing the tibial nerve with outward displacement of the peroneal nerve (Fig. 7). After dissecting from the capsular bed, it was entirely resected, and the cystic wall hole was repaired. The post-operative period went smoothly, with functional progress. At the 6-month follow-up, the patient’s ankle dorsiflexors had improved to Grade-4 muscular power and his plantar flexion had improved to Grade-5, with sensory recovery. On subsequent visit, NCS which was conducted at 1-year follow-up showed increase in the amplitude of the common peroneal and tibial nerve and no recurrence. The patient was able to return to his work with no difficulty in walking and had a near normal gait.
Therefore, he was planned for surgery after taking a written consent. The cyst was addressed through the posterior approach with a wide curvilinear incision with blunt dissection between the medial head of the gastrocnemius and semimembranosus muscles (Fig. 6). A massive multi-septate cyst measuring 13*6*6 cm was discovered, spanning from the distal thigh to the proximal tibia and obviously compressing the tibial nerve with outward displacement of the peroneal nerve (Fig. 7). After dissecting from the capsular bed, it was entirely resected, and the cystic wall hole was repaired. The post-operative period went smoothly, with functional progress. At the 6-month follow-up, the patient’s ankle dorsiflexors had improved to Grade-4 muscular power and his plantar flexion had improved to Grade-5, with sensory recovery. On subsequent visit, NCS which was conducted at 1-year follow-up showed increase in the amplitude of the common peroneal and tibial nerve and no recurrence. The patient was able to return to his work with no difficulty in walking and had a near normal gait.
It is thought that Baker cysts are an expansion of the gastrocnemio-semimembranosus bursa. In 50% of healthy adult participants, it has been demonstrated that this bursa communicates with the joint space of the knee. The substantial correlation between intra-articular disease and Baker cysts has been verified by recent studies. The popliteal cysts are frequently asymptomatic, but they can occasionally cause symptoms such as posterior knee soreness, a restricted range of movements, and complaints attributed to other knee diseases. Popliteal vein or artery aneurysms and benign tumors can frequently be mistaken for Baker cysts. It is an unusual consequence of Baker’s cyst, resulting in compressive neuropathy of both peroneal and tibial nerves. Very few examples of Baker cysts causing nerve compression have been documented in the literature out of which only one case report documented by Ji et al. in 2007 showed a Baker cyst induced tibial and peroneal nerve compression, which was also linked with a medial meniscal lesion which depicts that our case report is exceptionality rare[7]. Robertson et al. reported a case of ruptured popliteal cyst causing sciatic nerve compression in 2003 whereas our study showed intact popliteal cyst compressing at and distal to the sciatic nerve bifurcation [8]. Daneyemez et al., in 1998 reported a Baker’s cyst case that culminated in deep peroneal nerve compression[9]. DiRisio et al., in 1994 described a case of Baker’s cyst that produced compression of the tibial nerve motor branch to the medial gastrocnemius muscle[10]. Kashani et al., in 1985 reported a Baker’s cyst case causing tibial nerve entrapment in knee joint arthritis[11]. A clinical diagnosis and subsequent planning and treatment are frequently delayed in such cases due to wide range of differential diagnosis and inadequate clinical awareness which could result in incomplete recovery or even permanent impairment of the nerves jeopardizing the outcome of the treatment. Our case report showed a 60-year-old male patient with 5-year asymptomatic history of Baker’s cyst with insidious onset and a non-traumatic etiology presented with a 5-month history of hyposthesias of the right leg along with knee discomfort that worsened in 2 months with calf atrophy and foot drop with a high stepping gait along with progressive difficulty in walking. He was thoroughly evaluated, examined, and ultimately confirmed the diagnosis with NCS and MRI right knee after ruling out spinal and deep vein pathology. Therefore, patient was planned for open cyst excision and repair that revealed a large multi-septate cyst communicating with the joint; thereby compressing the tibial and displacing the peroneal nerves. The cyst was completely resected and patient improved gradually over a 6 week–6-month period with resolution of foot drop and sensory impairment.
Compressive neuropathy of both peroneal and tibial nerves secondary to an isolated and unruptured Baker’s cyst is exceedingly a rare entity and an uncommon consequence. An early diagnosis and a prudent treatment are essential to have a good functional outcome. Early decompression by an open cyst excision and repair with nerve decompression resulted in better prognosis, a near normal recovery of the patient with no recurrence.
This case demonstrates that an isolated Baker’s cyst can cause an uncommon consequence like compression neuropathy involving combined common peroneal and tibial nerves. MRI of the knee joint as well as NCS plays a crucial role in the diagnosis. Cyst excision by open method and repair of the defect with decompression of the tibial and peroneal nerves may be a more judicious and successful strategy for resolving symptoms quickly, experiencing minimal recurrence as well as to prevent permanent impairment.
References
- 1.Costello PB, Kennedy AC, Green FA. Dissected popliteal cyst: An unusual presentation of acute gout. Am J Med Sci 1981;281:57-9. [Google Scholar]
- 2.Nelson C, Haines JD Jr., Harper CA 3rd. Gout presenting as a popliteal cyst. A case of pseudothrombophlebitis. Postgrad Med 1987;82:73-4. [Google Scholar]
- 3.Labropoulos N, Shifrin DA, Paxinos O. New insights into the development of popliteal cysts. Br J Surg 2004;91:1313-8. [Google Scholar]
- 4.Spinner RJ, Atkinson JL, Harper CM Jr., Wenger DE. Recurrent intraneural ganglion cyst of the tibial nerve. Case report. J Neurosurg 2000;92:334-7. [Google Scholar]
- 5.Rawal A, Ratnam KR, Yin Q, Sinopidis C, Frostick SP. Compression neuropathy of common peroneal nerve caused by an extraneural ganglion: A report of two cases. Microsurgery 2004;24:63-6. [Google Scholar]
- 6.Adn M, Hamlat A, Morandi X, Guegan Y. Intraneural ganglion cyst of the tibial nerve. Acta Neurochir [Wien] 2006;148:885-90; discussion 889-90. [Google Scholar]
- 7.Ji JH, Shafi M, Kim WY, Park SH, Cheon JO. Compressive neuropathy of the tibial nerve and peroneal nerve by a Baker’s cyst: Case report. Knee 2007;14:249-52. [Google Scholar]
- 8.Robertson CM, Robertson RF, Strazerri JC. Proximal dissection of a popliteal cyst with sciatic nerve compression. Orthopedics 2003;26:1231-2. [Google Scholar]
- 9.Daneyemez M, Baysefer A, Acka G, Kirdemir V, Seber N. Nerve entrapment by a firmly wrapped Baker cyst. Minim Invasive Neurosurg 1998;41:172-4. [Google Scholar]
- 10.DiRisio D, Lazaro R, Popp AJ. Nerve entrapment and calf atrophy caused by a Baker’s cyst: Case report. Neurosurgery 1994;35:333-4; discussion 334. [Google Scholar]
- 11.Kashani SR, Moon AH, Gaunt WD. Tibial nerve entrapment by a Baker cyst: Case report. Arch Phys Med Rehabil 1985;66:49-51. [Google Scholar]








