Glenohumeral dislocations are a rare entity in skeletally immature patients but, when associated with nerve palsies, anatomic nerve variants must be considered and if a spontaneous recovery is not achieved within 6 months of the onset, surgery should be recommended.
Dr. Frédéric Teboul, Rue George Bizet 23, 92 boulevard de Courcelles, Paris, France. E-mail: f_teboul@hotmail.com
Introduction: Traumatic glenohumeral dislocation is very rare in skeletally immature patients, and there are no reports in the literature describing the risk of associated nerve injuries. In the general population, the most commonly affected nerve is the axillary, but anatomical variations with a common origin between the musculocutaneous and median nerves exist that alter the respective positions and courses of these nerves and can make them more prone to injury during a glenohumeral dislocation.
Case Report: A 10-year-old girl presented with incomplete median nerve palsy without any recuperation 8 months after an anterior glenohumeral dislocation. Surgical exploration was performed and revealed a common origin of the musculocutaneus and median nerve, with bifurcation just distal to the glenohumeral joint, making it susceptible to compression-elongation trauma during dislocation. A careful neurolysis was performed, and there was a complete recovery of median nerve function.
Conclusion: Glenohumeral dislocation associated with nerve injury is very rare in children. When a nerve injury occurs, one should be aware of possible anatomical variations of the infraclavicular plexus.
Keywords: Shoulder dislocation, glenohumeral dislocation, high median nerve palsy, median nerve injury.
Traumatic glenohumeral dislocation is very rare in skeletally immature patients, especially in the age group younger than 12 years. Given the specific anatomy of the immature skeleton, fractures are more common than dislocations after trauma in this age group [1,2]. Due to the low incidence, little is known about the exact pathoanatomy of glenohumeral dislocation in pediatric patients, and there are no reports in the literature describing the risk of associated nerve injuries. In the general population, nerve injury after glenohumeral dislocation is not rare. Most often, the axillary nerve is involved. The median and ulnar nerves are involved less frequently due to the anatomical position of these nerves [3]. However, an anatomical variant of the median nerve is described in which the musculocutaneous (MC) and median nerve share a common origin [4]. This alters the respective position and course of these nerves and can make them more prone to injury during a glenohumeral dislocation. We present a case of an isolated high median nerve palsy after a shoulder dislocation in a 10-year-old child with an anatomical variation of the median nerve. To the best of our knowledge, this is the first report of a nerve injury after an anterior shoulder dislocation in a pediatric patient.
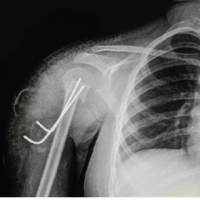
A 10-year-old female child presented with incomplete median nerve palsy without any recovery 8 months after an anterior glenohumeral shoulder dislocation. The shoulder dislocation was caused by a fall from a horse. A closed reduction was performed within 6 h after trauma, followed by a period of 4 weeks of relative immobilization and subsequent physiotherapy. The initial X-ray is shown in Fig. 1.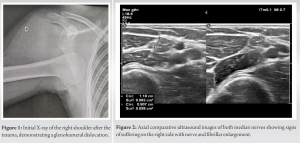
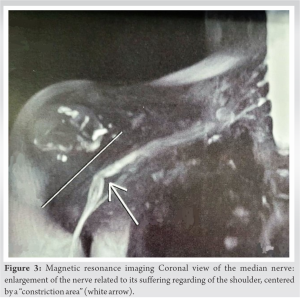
Clinical examination revealed an isolated incomplete palsy of the median nerve: hypoesthesia at the level of the palmar aspect of digits 3 and 4 (equivalent to a medical research council scale [MRCS] score S2); complete anesthesia at the level of the palmar aspect of digits 1 and 2 and at the thenar region (MRCS score S0); weakness of the second flexor digitorum profundus muscle (MRCS score M2); and paralysis of the flexor pollicis longus (MRCS score M0). There were no signs of instability in the shoulder. An electromyography performed 7 months after trauma showed no conduction through the median nerve. The interpretation of ultrasound examination and magnetic resonance imaging was complicated by scar tissue around the infraclavicular plexus; however, a clear image of nerve compression at the level of the proximal median nerve was seen (Fig. 2 and 3).
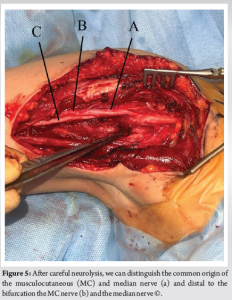
There were no signs of structural lesions of the glenohumeral joint or the capsule. As there was no functional recovery of the median nerve 8 months after trauma, and considering the imaging and electrodiagnostic findings, the decision was made to proceed with surgical exploration. An infraclavicular approach to the brachial plexus was performed. The plane between the deltoid and pectoralis major muscles was developed, and the pectoralis major was partially detached from its insertion. The conjoint tendon was retracted laterally, and the pectoralis minor tendon was spread medially. A proximal dissection of the infraclavicular plexus was carried out. The physiological fat embracing the brachial plexus had completely turned into fibrous scar tissue. A careful dissection of all terminal branches of the infraclavicular plexus was performed. However, the median nerve could not be retrieved initially. When stimulating the posterior aspect of the putative MC nerve, a response was elicited at the level of the median nerve musculature. The dissection was continued more distal, and a common origin of the MC and median nerves was revealed, with bifurcation just distal to the glenohumeral joint. The common nerve trunk of the MC and median nerve presumably underwent a compression-elongation injury during dislocation, with the subsequent formation of surrounding scar tissue. Given that the nerve fascicles of the median nerve lie posteriorly at the level of the common nerve trunk, these were more susceptible to the trauma. A careful neurolysis was performed with resection of the surrounding scar tissue (Fig. 4 and 5). The post-operative course was uncomplicated. Four months after surgery, there was a complete motor recovery, and the patient resumed horseback riding and artistic gymnastics. After 4 months, there was still some dysesthesia in the median nerve area with an MRCS score between S3+ and S4 at the median pulp of the thumb and index finger. Twelve months after surgery, there was complete motor and sensory recovery.
Shoulder dislocation in young children is very rare. The proportion of shoulder dislocations under the age of 10 is considered to be <2% of all dislocations [5]. However, the epidemiology of shoulder dislocations in children is described in a few studies [6,7]. Zacchilli and Owens reported an incidence of shoulder dislocation of 0.92/100,000 people-year in the age group between zero and 9 years old [6]. Leroux et al. stated an overall incidence density rate (IDR) of primary anterior shoulder dislocation of 20.1/100,000 people-year in subjects with an age range of 10–16 years and an IDR of 1.3/100,000 people-year among female patients aged 10 years [7]. The reason for this low incidence of shoulder dislocations in younger children is manifold. The insertion of the capsule on the glenoid is located more laterally in the skeletally immature patient, thereby resulting in a smaller anterior-inferior recess and less risk of dislocation. Furthermore, the proximal humeral physis is almost entirely extra-articular in the skeletally immature shoulder. Since ligaments are stronger than bones and physis in these immature patients, shoulder injury leads to physeal or metaphyseal fractures rather than dislocation. To the best of our knowledge, there are no reports in the literature about nerve lesions after shoulder dislocation in children. This is possibly due to the low incidence of shoulder dislocations and/or greater tolerance of nerve tissue in the child to trauma [3]. In the general population, peripheral nerve injuries following anterior dislocation are common, with an incidence varying from 5.4% to 55% [3]. Injury to the axillary nerve is the most common, with a reported incidence of about 10% or higher [8]. The incidence of injuries to other nerves of the brachial plexus varies in different studies [3]. Median nerve injury is infrequently reported, possibly because of the relatively greater distance between the humerus and the course of this nerve. Only one case report was found describing an isolated median nerve neuropathy following a fall and anterior shoulder dislocation [9]. In our patient, the median nerve was more prone to injury because of its anatomical variant. The common trunk of the median and MC nerves was located just anterior to the glenohumeral joint. Such variations in connections between the MC and median nerves are not rare, but there are rarely reports on their clinical relevance. An anatomical study performed on 138 cadavers showed variations in 64 cadavers (46.4%) [4]. Fusion of both nerves was seen in 19.2% of the cases [4]. Another study described communications between the MC and median nerves in 53.6% of 56 dissected upper limbs. In one case (1.8%), the MC and the median nerve presented a distal origin, as was the case in our patient [10]. In the majority of infraclavicular lesions after shoulder dislocation, spontaneous improvement or return of limb function can be expected after a period of observation and/or rehabilitation. Spontaneous recovery of injured nerves has been described in 75–100% of the patients [3]. In the case of poor recovery, surgical treatment is imminent. External neurolysis can improve nerve conductivity, and additional internal neurolysis is required when severe neuropathic pain accompanies or thickened epineurium compressing nerve bundles and causing compression of the vasa nervorum is observed intraoperatively [3]. The timing of brachial plexus surgery for insufficient recovery remains a controversial issue that needs balancing between allowing time for spontaneous nerve regeneration and undertaking surgery before atrophy due to denervation occurs. According to current literature, the optimal time frame for surgery is considered to be between 6 and 9 months. However, early surgery within 3 months of the injury is being advocated by a growing number of authors [3].
Glenohumeral dislocation associated with a nerve injury is a very rare entity in children. When a nerve injury occurs, possible anatomical variations of the infraclavicular plexus should be taken into consideration. If there is no spontaneous recovery within 6 months, surgical exploration should be considered.
Traumatic shoulder dislocation is a very rare occurrence in pediatric patients, and its association with nerve palsy is even rarer. Given its rarity, it is important to consider and investigate the presence of anatomical variants when a nerve lesion occurs. Typically, there is spontaneous recovery following an infraclavicular palsy, but if this does not occur within 6 months, surgical exploration should be considered.
References
- 1.Li X, Ma R, Nielsen NM, Gulotta LV, Dines JS, Owens BD. Management of shoulder instability in the skeletally immature patient. J Am Acad Orthop Surg 2013;21:529-37. [Google Scholar | PubMed]
- 2.Longo UG, Salvatore G, Locher J, Ruzzini L, Candela V, Berton A, et al. Epidemiology of paediatric shoulder dislocation: A nationwide study in Italy from 2001 to 2014. Int J Environ Res Public Health 2020;17:2834. [Google Scholar | PubMed]
- 3.Gutkowska O, Martynkiewicz J, Urban M, Gosk J. Brachial plexus injury after shoulder dislocation: A literature review. Neurosurg Rev 2020;43:407-23. [Google Scholar | PubMed]
- 4.Choi D, Rodríguez-Niedenführ M, Vázquez T, Parkin I, Sañudo JR . Patterns of connections bet ween the musculocutaneous and median nerves in the axilla and arm. Clin Anat 2002;15:11-7. [Google Scholar | PubMed]
- 5.Bishop JY, Flatow EL. Pediatric shoulder trauma. Clin Orthop 2005;432:41-8. [Google Scholar | PubMed]
- 6.Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in theUnited States. J Bone Joint Surg Am 2010;92:542-9. [Google Scholar | PubMed]
- 7.Leroux T, Ogilvie-Harris D, Veillette C, Chahal J, Dwyer T, Khoshbin A, et al. The epidemiology of primary anterior shoulder dislocations in patients aged 10 to 16 years. Am J Sports Med 2015;43:2111-7. [Google Scholar | PubMed]
- 8.Cutts S, Prempeh M, Drew S. Anterior shoulder dislocation. Ann R Coll Surg Engl 2009;91:2-7. [Google Scholar | PubMed]
- 9.Silsby M, Robertson A, Yiannikas C. Proximal median neuropathy following anterior shoulder dislocation: The use of magnetic resonance neurography. Neurohospitalist 2021;11:75-9. [Google Scholar | PubMed]
- 10.Guerri-Guttenberg RA, Ingolotti M. Classif ying musculocutaneous nerve variations. Clin Anat 2009;22:671- 83. [Google Scholar | PubMed]