CASE REPORT – Paediatric Orthopaedics
Dr Ashok K Shyam,
Indian Orthopaedic Research Group,
Mumbai, Maharashtra, India.
Email: drashokshyam@yahoo.co.uk
Introduction: Bony hemangiomas are rare lesions in growing skeleton. Affection of the epiphyseal plate by a bony hemangioma leading to growth retardation is rare.
Case report: We report the radiological picture of a juxtaphyseal osseous hemangioma affecting the capital femoral physis leading to coxa vara and coxa breva deformity. This hemangioma is also a rarity as it has both intracortical and intra medullary components. A diagnostic and therapeutic. CT guided core needle biopsy/decompression was performed to confirm the histopathological diagnosis and to decompress the lesion. Patient was treated conservatively with shoe raise and regular checkups and at two year follow-up there were no interval changes noted on the radiographs with patient completely asymptomatic.
Conclusion: Juxtaphyseal hemangiomas may be amenable to needle decompression, however longer follow will be required to assess the further response.
Keywords: osseous hemangioma, capital femoral physis, coxa vara.
Hemangiomas of the bone are rare lesions accounting for only 1% of primary bone tumors [1]. About 75% are located in the vertebrae and skull. Of the lesions in extremity, tibia is the most common site (43%) followed by femur (26%) [1]. In the long bones diaphysis and metadiaphysis account for 78% lesions and metaphyseal lesions are found in only 12%. The intraosseous hemangiomas are medullary in 55%, periosteal in 33% and intracortical in 12% [1].They are extremely rare in age less than 10 years (2% to 5%) [1]. The incidence of growth retardation secondary to bony haemangioma is reported by only one study as 7.5% [2]. We present a case of intraosseous hemangioma of proximal femur metaphysis in an 8 year old boy, with coxa vara and coxa breva deformity secondary to physeal growth arrest. Radiographic finding confirm it to be a combined intracortical and medullary lesion with involvement of the medial cortex of the neck of the femur. This is a very rare presentation and we believe it is the first case of intraosseous hemangioma having both intracortical and intramedullary components with affection of capital femoral physis
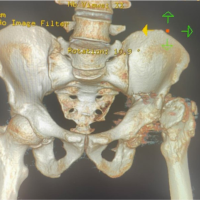
An 8 year 2 month old boy presented to our outpatient department with limping gait noticed since 6 month. Patient had intermittent dull ache localized to right groin since last 4 months. There was no history of trauma or fever. On examination there was diffuse tenderness over right groin and restricted range of hip movements that were terminally painful. Patient walked with abductor lurch with shortening of 1.5 cms in right lower limb on clinical examination. Plain radiograph of pelvis with both hips showed moth eaten pattern of osteolytic lesion in right proximal femur. There was growth plate widening and obvious coxa vara deformity at the right proximal femur (Fig. 1). The neck shaft angle was 115° on the right side as compared to 131° on the left side. Coxa breva was noted with right side axial length of the neck being 1.2 cms smaller than the left side (measurement adjusted for magnification). The lateral radiograph showed involvement from the physeal line up to the lesser trochanter with normal epiphysis (Fig. 1).
The pelvis on the right side was lowered down with mild right side thoracic scoliosis. The other soft tissue and contralateral side appeared unremarkable. Differential diagnosis on radiograph was eosinophilic granuloma, chronic osteomyelitis and hemangioma. Baseline haematological investigations showed ESR of 2 mm at end of one hour with C-reactive protein <0.1 mg/dl. Rest of the haematological profile was also within normal limits. MRI was performed on a 0.2 tesla MR system with images obtained in axial, coronal and sagittal planes. MRI shows high intensity lobulated tubular lesions on TW2 weighted images and hypointense on TW1 images (Fig. 2). The lesion is mostly intracortical in the medial cortex of the neck of femur extending from the medial part of capital femoral epiphysis up to the lesser trochanter. There is associated cortical thickening seen in the surrounding area. An intramedullary extension is also seen reaching up to the greater trochanter (Fig. 3). The entire capital femoral epiphysis shows altered signals as compared to the opposite side with the physeal hypodensity almost obliterated on the medial side. The axial cuts too show multi-chambered tubular lesion with axis parallel to the neck of femur mostly located in the inferomedial part of the neck. On contrast study, the lesion showed moderate enhancement (Fig. 4).
There was no fluid-fluid level and subtle reactive synovitis was noted in the right hip. Differential diagnosis after MRI was hemangioma and eosinophilic granuloma. A bone scan showed mild increase in uptake in the right proximal femur with no other lesions in the skeleton. The extent of the lesion, closeness to the physis and the intracortical location in the inferomedial part of the neck of femur discouraged us from performing open procedure. We hypothesised increase in the intraosseous pressure to be the cause of symptoms and planned a CT guided needle biopsy/decompression. A fleshy sample of size 0.5×0.2×0.1 cms was obtained. Intraoperative CT scan showed multiple bony channels in the inferomedial part of the femoral neck filled with blood and air leaked into the area after the procedure (Fig. 5).
Surrounding hematoma due to needle biopsy was noted too. Histopathology showed proliferation of capillary vessels and sinuses with no malignant features suggesting diagnosis of cavernous hemangioma. Patient was given short term analgesic for pain and shoe raise for limb length discrepancy and was advised to avoid contact sports. Within two weeks patient was walking pain free although shortening persisted. Regular follow up of the patient was done and at two years follow up the patient is having no pain, with full range of movement. He walks comfortably with shoe raise with no abductor lurch. The recent radiographs showed no interval changes and the coxa vara and coxa breva did not increase in magnitude. Patient is advised regular follow up till skeletal maturity to monitor the progress of the hip deformities.
Growth abnormalities are seen commonly in congenital vascular malformations [2]. Most of these abnormalities are growth acceleration and incidence of growth retardation is low. A study of limb length discrepancy in purely intraosseous vascular lesion is lacking. However it is generally considered that increase in blood flow to the physis stimulates the growth process leading to overgrowth. For undergrowth venous hypertension or phleboectasia are pathological processes that are involved. Only about 25% of the osseous hemangiomas involve the extremities. They can be classified into medullary intracortical and periosteal. Intracortical is the rarest of them all. The medullary type is further subdivided into diaphyseal (48%), metadiaphyseal (30%), metaphyseal (12%), metaepiphyseal (4%), epimetadiaphyseal (3%) and epiphyseal (1%) [1]. Our case had a major intracortical component starting at juxtaphyseal area involving the inferomedial cortex with involvement of the medullary cavity reaching up to the greater trochanter. Such an involvement of mixed intracortical and intramedullary type has never been reported before. Haemangiomas involving the axial skeleton are commonly asymptomatic [3] and may remain undetected for long time. They are often discovered incidentally during a radiographic study [3], whereas haemangiomas of the appendicular skeleton are often symptomatic. In one series, peripheral haemangioma were symptomatic in 91% of cases, out of which 37% had pain, 7% had swelling and 7% had restriction of function due to pathological fracture [1]. The pain may be secondary to an embolic phenomenon, intraosseous hypertension or pathological fractures. In our case, we believe, was due to intraosseous hypertension and needle decompression lead to pain relief.
Diagnosis of a hemangioma is based on the radiological and pathological picture of the individual cases. Radiologically, on radiographs the intraosseous hemangiomas have varied presentations. They may show coarse loculated, sunburst, moth-eaten, and soap bubble appearance due to expansive proliferation of engorged vessels and thickened, remodelled bone trabeculae [4]. On MRI, haemangiomas show a variable appearance and may demonstrate low, intermediate or high signal intensity. The MR signal characteristics of a hemangioma are dependent on the quantity of slowmoving venous blood and on the ratio of red marrow to converted fatty marrow present within the lesion. Haemangiomas may sometimes appear hyperintense on T1 WI because of their fat content. They are usually hyperintense on T2 WI or STIR [4]. Hyperintensity seen on T2 WI is due to free water in stagnant blood within the haemangioma. On STIR images, these lesions appear markedly intense due to suppression of normal bone marrow. Haemangiomas can show marked to minimal or no enhancement after contrast administration [3]. In our case, the lesion was hypointense on T1 WI and markedly hyperintense on T2 WI. Low or high signal may be seen on T1-weighted images, and high signal on water-sensitive sequences [4]. Small lesions may appear bright on T1-weighted images; however, in larger lesions, the trabeculae typically show low signal on T1-weighted images. A well-defined lesion with distinctive thickened irregular trabeculae having a lattice-like pattern on plain radiographs, and presence of high signal intensity on MRI is the most helpful diagnostic imaging features for making the diagnosis of an intraosseous vascular malformation in long bones5. A CT scan is generally done for axial hemangiomas. The CT appearance is variable, and in the calvaria most commonly shows a characteristic sharply marginated expansile lesion with intact inner and outer tables and a sunburst pattern of radiating trabeculae. ‘‘Soap bubble’’ and ‘‘honeycomb’’ configurations may also occur [4]. In our case the intra-operative CT-scan confirmed that lesion was mostly intracortical with trabeculaes seen running along the axis of the neck of femur.
Histologically, diagnosis by an en bloc specimen is quite easy. The hemangiomas can be classified into cavernous, capillary venous or mixed [1]. Amongst these cavernous is the most common type accounting for 50% of the cases reported. Capillary hemangiomas are 10% and other types are rare. The conformation generally requires an excisional biopsy which can be a destructive procedure especially in juxtaphyseal and intracortical location as in our case. Akira et al reported that when imaging findings suggest hemangioma, a CT guided biopsy is appropriate for confirmation of the diagnosis [6]. Recently Nakamura et al too emphasized the value of needle biopsy in cases of hemangiomas to confirm the diagnosis [7]. We performed a CT guided biopsy and obtained an adequate specimen to confirm the diagnosis of hemangioma. No complications, such as massive bleeding or subcutaneous hematoma, occurred in relation to the biopsy. We found CT guided biopsy to be safe and useful procedure for obtaining a definitive diagnosis. Treatment of intraosseous hemangiomas depends on many factors. Asymptomatic lesions in non weight bearing areas can be safely treated conservatively. In weight bearing areas the risk of pathological fracture depends on the type of bone and extent of the lesion. Treatments for symptomatic bone hemangiomas include surgery, radiotherapy, and transarterial embolization. En bloc excision has achieved excellent results in the skull, rib, and nasal bone. If symptomatic lesions are located in the spine or pelvis, treatment is quite difficult [8]. Surgical treatment is often associated with profuse hemorrhage, incomplete resection, local recurrence, and lengthy convalescence. Percutaneus injection of ethanol for bone and soft-tissue hemangiomas has proved efficacious [8]. If severe operative blood loss is expected, such a procedure may be considered the treatment of choice. Our lesion was located in the weight bearing area however surgical excision in this juxtaphyseal area was deemed to cause more damage to the physes. Keeping in mind the chances of spontaneous regression in cases of soft tissue hemangiomas especially during this period of childhood, we decided to try the conservative approach. The patient was given simple analgesics and rest and was pain free within 2 weeks post needle decompression. Patient was completely asymptomatic and was walking fine with shoe raise at one year follow up. Absence of radiological interval changes prompted us to continue the conservative treatment with regular follow up.
We present a rare case of epiphyseal growth arrest secondary to a juxtaphyseal hemangioma causing coxa vara and coxa breva deformity treated conservatively with needle decompression.
CLINICAL MESSAGE
Some cases of Juxtaphyseal hemangiomas may be amenable to needle decompression with minimal complications
The authors will like to acknowledge Indian Orthopaedic Research Group for help in manuscript preparation
References
- 1.Kaleem Z, Kyriakos M, Totty WG. Solitary skeletal hemangioma of the extremities. Skeletal Radiol 2000;29:502–13 [Google Scholar | PubMed]
- 2.Kim YW, Lee SH, Kim DI, Do YS, Lee BB. Risk factors for leg length discrepancy in patients with congenital vascular malformation. J Vasc Surg 2006;44(3):545-53 [Google Scholar | PubMed]
- 3.Sung MS, Kim YS, Resnick D. Epithelioid hemangioma of bone. Skeletal Radiol 2000;29:530–4. [Google Scholar | PubMed]
- 4.Moore SL, Chun JK, Mitre SA, Som PM. Intraosseous Hemangioma of the Zygoma: CT and MR Findings. AJNR Am J Neuroradiol 2001;22(7):1383-5. [Google Scholar | PubMed]
- 5.Wenger DE, Wold LE. Benign vascular lesions of bone: radiologic and pathologic features. Skeletal Radiol 2000;29:63-74. [Google Scholar | PubMed]
- 6.Ogose A, Hotta T, Morita T, Takizawa T, Ohsawa H, Hirata Y. Solitary osseous hemangioma outside the spinal and craniofacial bones. Arch Orthop Trauma Surg 2000;120(5- 6):262-6. [Google Scholar | PubMed]
- 7.Nakamura H, Kawasaki N, Taguchi M, Kitamura H. Cavernous hemangioma of the rib diagnosed preoperatively by percutaneous needle biopsy. Gen Thorac Cardiovasc Surg 2007;55(3):134-7 [Google Scholar | PubMed]
- 8.Doppman JL, Oldfield EH, Heiss JD. Symptomatic vertebral hemangiomas: treatment by means of direct intralesional injection of ethanol. Radiology 2000;214(2):341 [Google Scholar | PubMed]