The long platform PPP measurement system is useful for the evaluation of foot reconstructive surgery and the development of treatments that can yield further improvements in the results.
Dr. Akira Kodama,
Department of Orthopaedic Surgery, Biomedical and Health Sciences, Hiroshima University, 1-2-3, Kasumi, Minami-ku, Hiroshima, Hiroshima, 734-8551, Japan.
E-mail: akirakodama@hiroshima-u.ac.jp
Introduction: An extensor digitorum brevis (EDB) flap can be used to cover a small soft-tissue defect and has been widely used as pedicled flap to cover defects around the ankle and foot. However, its post-operative functional recovery is unknown. Few reports have evaluated gait after foot flap surgeries, although gait assessment is considered to be necessary for functional evaluation after foot reconstruction. We performed a reverse EDB flap to treat a right hallux injury and conducted a plantar partial pressure (PPP) analysis as a postoperative functional evaluation.
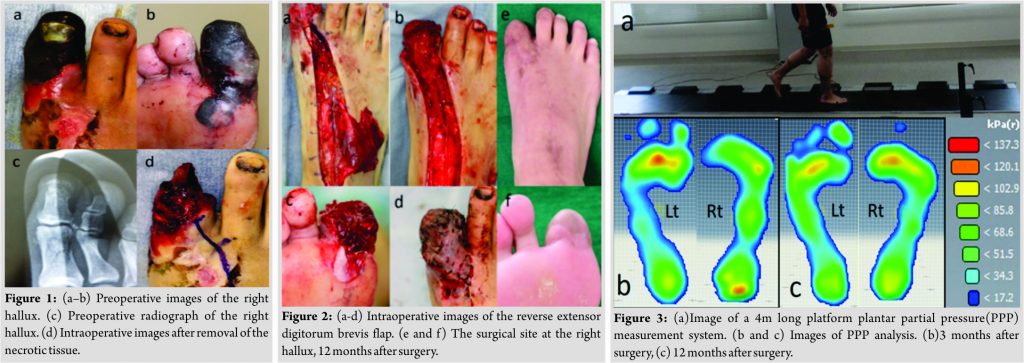
Case Report: A 30-year-old laborer suffered an injury resulting in necrosis of the distal phalanx and soft-tissue defect of the proximal phalanx. After amputation, the proximal phalanx was covered with a reverse EDB flap. PPP analysis involved a 4-m-long platform system (P-Walk) and was conducted 3- and 12-month post-surgery. Walking velocity and the single-support phase on the affected limb had increased markedly after 12 months. After 12 months, the PPP of the first metatarsal head was greater than on the unaffected side, and the cadence and single-leg support rate were equal to the unaffected side.
Conclusion: A nearly normal gait was obtained by covering the basal part of the hallux with an EDB flap and preserving the metatarsophalangeal joint.
Keywords: Extensor digitorum brevis flap, toe reconstruction, gait analysis, plantar partial pressure analysis, hallux.
The extensor digitorum brevis(EDB) has an average length and width of 5.9 and 2.4–3.9 cm, respectively [1]. It is vascularized by the lateral tarsal artery and vein, which is an independent vascular pedicle that branches from the dorsalis pedis artery and vein. An EDB flap can be used to cover a small soft-tissue defect and has been widely used as an island flap with antegrade flow to cover defects around the ankle and dorsal foot [2,3,4,5,6,7], a functioning free EDB muscle flap [8,9,10], and to cover the upper lip [11]. The EDB can also be used as a reverse-flow flap because of its connection to the plantar arterial system and ability to cover the distal dorsal foot and toe. However, there are few reports on such an approach for the toe [12,13]. Postoperative evaluation of flaps for foot reconstruction is conventionally conducted based on flap engraftment, appearance, and the use of subjective questionnaires such as the Enneking [14] and foot function index (FFI) [15] questionnaires. However, pain greatly affects the Enneking and FFI scores (by 26.9% and 33.3%, respectively [16]), so they can only be used as proxy assessments of lower limb function. Gaite valuation is considered necessary for foot function assessment. However, few reports evaluate gait after foot flap surgeries. Due to technological advancements, clinical gait can now be analyzed using three-dimensional motion analysis or pressure platforms. We hypothesized that these approaches could be used to evaluate gait after foot flap surgery. In this report, we describe a reverse EDB flap surgery to treat a hallux injury, and a plantar partial pressure (PPP) analysis performed as a postoperative functional evaluation.
This study was approved by the institutional review board at the authors’ institution. The patient was informed that data from the case would be submitted for publication and gave his consent.
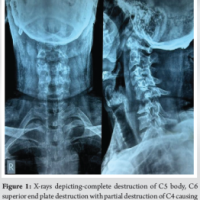
A 500 kg iron plate fell onto the right hallux of a male 30-year-old laborer, who was referred to our clinic 10 days later, due to necrosis of the hallux. Carbonization from the center of the proximal phalanx of the hallux and a fracture at the proximal phalanx without dislocation were observed (Fig. 1a-c). During surgery, carbonization and ischemia were observed in the distal phalanx. To remove necrotic tissue, the hallux was amputated at the interphalangeal joint (Fig. 1d), and the soft-tissue defect of the base phalanx was covered with a reverse EDB flap.
A straight skin incision was made along the dorsalis pedis artery, from the distal end of the extensor retinaculum to the stump of the hallux. The long extensor tendons were retracted to expose the EDB. The distal end of the EDB was separated at the muscle-tendon junction, and the proximal end of the muscle was dissected from the insertion at the metatarsal bone. The EDB flap was elevated, and the dorsalis pedis vascular pedicle was cut proximal to the flap. The deep peroneal nerve was preserved. The distal parts of the dorsalis pedis artery and vein were dissected to the pivot point to elevate the flap (Fig. 2a). This was rotated to cover the bony and tendinous surface of the base of the hallux, fixed with bolster sutures (Fig. 2b and c), and a split-thickness thigh skin graft was used to cover it (Fig. 2d). The muscle flap survived, but the plantar skin graft caused partial necrosis, so a supplemental skin graft was added 8 weeks later. 3 months post-surgery, the patient could walk without protection of the affected site. At the final follow-up 12-months post-surgery, the patient experienced no pain during walking and was able to jog. The donor and recipient sites healed completely (Fig. 2e and f).
We constructed a 4-m-long platform with eight 0.5-m-long foot pressure panels (P-Walk®, BTS Bioengineering, Italy; Fig. 3a). The patient walked on this platform at his normal walking speed. Data were analyzed using G-Studio software (BTS Bioengineering). Velocity (km/h), cadence(steps/min), percentage of single-leg support phase on the affected side, and PPP were evaluated. The maximum PPP for six regions (T1, hallux; M1, first metatarsal head; M3, third metatarsal head; M5, fifth metatarsal head; MF, midfoot; and HL, heel) was calculated from the averaged values of the last three steps taken on each foot (Table 1). Measurements were made three and 12 months after surgery.
The patient’s walking velocity increased over time. There was no substantial change in cadence, but the single-support phase on the affected limb increased markedly at 6-month post-surgery (Table 1). The load applied to M1 increased over time, whereas load was attenuated in MF (Tables 1; Fig. 3b and c).
There is a previous report of eight patients with reverse-flow EDB flaps on their feet, one of whom had an EDB flap covering the dorsal side of the hallux [12]. A reverse EDB flap also has been used to cover the dorsal toe, with an advanced flap over the plantar side [13]. Although it is preferable to use tissue with thick skin to cover the load-bearing sole, the advanced flap may affect walking by diminishing sensation or causing pain in the first metatarsophalangeal (MTP) joint. Here, we used an EDB flap to cover the dorsal and plantar sides of the proximal phalanx. The plantar-side skin of the proximal phalanx is thin and not suitable for load bearing; however, the load at the first MTP is more important than that at the proximal phalanx, and we were able to preserve normal conditions at that point by avoiding surgical intervention there. However, flap distance is limited to the length from the dorsal to the plantar sides of the proximal phalanx. Thus, the same flap cannot cover both the dorsal and plantar side of the distal phalanx. There are few reports of gait evaluation in postoperative assessment following foot reconstruction involving flaps or in donor-site assessment after harvesting a lower limb flap. One study, using three-dimensional gait analysis and platform-type plantar pressure analysis, found significant differences in lower-limb joint mobility between the donor and contralateral limbs after a medial plantar artery flap [17]. Walking patterns were compared in patients who received flap coverage of either the sole or non-weight-bearing areas of the foot. In both groups, peak pressures were greater, and the single-leg support phase on the affected side was shorter [16]. Finally, an analysis of the dynamic loading performance of patients with fasciocutaneous flaps over their heels found that the affected heels retained high functionality [18]. Various quantification equipment using different technologies including insole type [19,20] and platform type [21,22] have been developed for foot pressure analysis. Among them, the long-platform PPP measurement system used in this report has several advantages over other methods. First, we could observe changes in dynamic pressure during continuous walking and take at least five footsteps for each foot. In contrast, only one 0.4–0.5 m panel was used in the aforementioned studies [16,18]. Second, we could evaluate stride, walking cycle, and single-leg support rate without further motion analysis. Third, there was no need to attach or calibrate a marker, and measurements could begin without preparation. This study provides a case study of the evaluation of gait recovery after a reverse EDB flap, using the long-platform-type PPP measurement system. The results indicate the following: MF was compensating for M1, which could not bear a full walking load during the early postoperative period; the PPP of M1 was higher than that of the unaffected side; and the cadence and single-leg support rate were equal to the unaffected side 12-month post-surgery. A normal gait was thus obtained by covering the basal part of the hallux with an EDB flap and preserving the MTP joint. In addition, although the distal phalanx was absent and the proximal phalanx had no weight-bearing ability, we suggest that the MTP bores a greater pressure than the unaffected side because it was compensating for the hallux. This study has some limitations. First, it lacks comparison with preoperative findings; we were unable to assess pre-surgery PPP because the patient could not walk. Instead, we observed postoperative gait recovery by comparing the post-surgical results. Second, we cannot conclude that preserving the base phalanx is better for walking because this study is a case report, and there is no control group that has lost the base phalanx. The answer will come out if further study is done to compare the gait changes due to differences in the defect level of the great toe using the gait analysis presented in this study. Finally, the short follow-up period is one of the limitations of this study. As a long-term complication, Osteoarthritis at the first MTP is concerned. The first MTP was not damaged at the initial injury, so it is considered unlikely to progress to arthritis even in the long term. However, since the maximum value of the partial pressure of M1 was found to be higher than that of the health side also in this research result, it is thought that deletion of toe may have some effect on overload.
This report provides a case study of the evaluation of gait recovery after a reverse EDB flap, using the long platform-type PPP measurement system. A nearly normal gait was obtained by covering the basal part of the hallux with an EDB flap and preserving the MTP joint.
The long platform PPP measurement system we created made it possible to measure not only the PPP but also multiple gait parameters including velocity, cadence and walking cycle simultaneously. We recommend to perform gait analysis as functional evaluation after foot reconstruction.
References
- 1. Bakhach J, Demiri E, Chahidi N, Baudet J. Extensor digitorum brevis muscle flap: New refinements. Plast Reconstr Surg 1998;102:103-10. [Google Scholar] [PubMed]
- 2. Houdek MT, Wagner ER, Pensy RA, Eglseder WA. Extensor digitorum brevis flap for the coverage of ankle and dorsal foot wounds: A technical trick. J Orthop Trauma 2016;30:e404-8. [Google Scholar] [PubMed]
- 3. Chattar-Cora D, Pederson WC. Experience with the extensor digitorum brevis muscle flap for foot and ankle reconstruction. Ann Plast Surg 2006;57:289-94. [Google Scholar] [PubMed]
- 4. Kim JK, Choi SJ, Chung MS, Baek GH. Extensor digitorum brevis muscle flap using parallel incision. J Plast Reconstr Aesthet Surg 2009;62:1317-20. [Google Scholar] [PubMed]
- 5. Attinger CE, Ducic I, Cooper P, Zelen CM. The role of intrinsic muscle flaps of the foot for bone coverage in foot and ankle defects in diabetic and nondiabetic patients. Plast Reconstr Surg 2002;110:1047-54. [Google Scholar] [PubMed]
- 6. Giordano PA, Argenson C, Pequignot JP. Extensor digitorum brevis as an island flap in the reconstruction of soft-tissue defects in the lower limb. Plast Reconstr Surg 1989;83:100-9. [Google Scholar] [PubMed]
- 7. Landi A, Soragni O, Monteleone M. The extensor digitorum brevis muscle island flap for soft-tissue loss around the ankle. Plast Reconstr Surg 1985;75:892-7. [Google Scholar] [PubMed]
- 8. del Piñal F, Herrero F. Extensor digitorum brevis free flap: Anatomic study and further clinical applications. Plast Reconstr Surg 2000;105:1347-56. [Google Scholar] [PubMed]
- 9. Wang T, Regmi S, Liu H, Pan J, Hou R. Free lateral tarsal artery perforator flap with functioning extensor digitorum brevis muscle for thenar reconstruction: A case report. Arch Orthop Trauma Surg 2017;137:273-6. [Google Scholar] [PubMed]
- 10. Zhu SX, Zhang BX, Yao JX, Li ZY, Wang XL, Fu ZG, et al. Free musculocutaneous flap transfer of extensor digitorum brevis muscle by microvascular anastomosis for restoration of function of thenar and adductor pollicis muscles. Ann Plast Surg 1985;15:481-8. [Google Scholar] [PubMed]
- 11. Oh SJ, Chung CH. Upper-lip reconstruction using a free dorsalis pedis flap incorporating the extensor hallucis and digitorum brevis muscles. J Craniofac Surg 2011;22:998-9. [Google Scholar] [PubMed]
- 12. Hirase Y, Kojima T, Fukumoto K, Misu H, Yamaguchi T. Indication and practice of reverse flow extensor digitorum brevis muscle flap transfer. Ann Plast Surg 2003;51:273-7. [Google Scholar] [PubMed]
- 13. Koul AR, Patil RK, Philip VK. Coverage of defects over toes with distally based local flaps: A report of four cases. Indian J Plast Surg 2008;41:62-6. [Google Scholar] [PubMed]
- 14. Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res 1993;286:241-6. [Google Scholar] [PubMed]
- 15. Budiman-Mak E, Conrad KJ, Roach KE. The foot function index: A measure of foot pain and disability. J Clin Epidemiol 1991;44:561-70. [Google Scholar] [PubMed]
- 16. Meyer-Marcotty MV, Sutmoeller K, Kopp J, Vogt PM. Postoperative insole-paedobarographic gait analysis for patients with flap coverages of weight-bearing and non-weight-bearing areas of the foot. J Plast Reconstr Aesthet Surg 2012;65:482-8. [Google Scholar] [PubMed]
- 17. Paget JT, Izadi D, Haj-Basheer M, Barnett S, Winson I, Khan U, et al. Donor site morbidity of the medial plantar artery flap studied with gait and pressure analysis. Foot Ankle Surg 2015;21:60-6. [Google Scholar] [PubMed]
- 18. Karakostas T, Hsiang SM, Sarantopoulos C, Krause J. Dynamic loading performance of fasciocutaneous flaps and implications for gait. Clin Biomech (Bristol, Avon) 2007;22:478-85. [Google Scholar] [PubMed]
- 19. Hida T, Okuda R, Yasuda T, Jotoku T, Shima H, Neo M, et al. Comparison of plantar pressure distribution in patients with hallux valgus and healthy matched controls. J Orthop Sci 2017;22:1054-9. [Google Scholar] [PubMed]
- 20. Deleu PA, Leemrijse T, Vandeleene B, Maldague P, Devos Bevernage B. Plantar pressure relief using a forefoot offloading shoe. Foot Ankle Surg 2010;16:178-82. [Google Scholar] [PubMed]
- 21. Daglar B, Deveci A, Delialioglu OM, Kanatli U, Tasbas BA, Bayrakci K, et al. Results of triple arthrodesis: Effect of primary etiology. J Orthop Sci 2008;13:341-7. [Google Scholar] [PubMed]
- 22. Nawata K, Nishihara S, Hayashi I, Teshima R. Plantar pressure distribution during gait in athletes with functional instability of the ankle joint: Preliminary report. J Orthop Sci 2005;10:298-301. [Google Scholar] [PubMed]