Closed reduction and traction must be avoided in complex Kaplan's dislocation, which should be managed with open reduction with safe and easy dorsal approach.
Dr. Tushar Chandrakant Patil, Room No. 428, 300 Residents Hotel, GGMC and Sri JJ Group pf Hospital, Byculla - 400 008, Mumbai. Maharashtra. India. E-mail: tushar6919@gmail.com
Introduction:Finger dislocations account for 5% of upper extremity injuries. Metacarpophalangeal (MCP) joint/Kaplan dislocations post-trauma are of rare occurrence. An MCP joint dislocation is considered simple when it can be managed by closed reduction and considered complex when open reduction is necessary.
Case Report:Here, we present a rare case of dorsal Kaplan dislocation of left second MCP joint in an 11 years old male child, which was managed by open dorsal approach with stable reducion and good functional outcome.
Conclusion: We experienced closed reduction should not be tried in cases of complex dorsal dislocations. The dorsal approach of complex MCP dislocation is found to be safe and simple even in hands of inexperienced surgeons which may or may not need division of deep transverse ligament.
Keywords: Kaplan dislocation, metacarpophalangeal (MCP) joint, open reduction, dorsal approach, index finger.
Finger dislocations account for 5% of upper extremity injuries [1].
Metacarpophalangeal joint (Kaplan) dislocations post trauma are of rare occurrence. An MCP joint dislocation is considered simple when it can be managed by closed reduction and considered complex when open reduction is necessary. In 1876, Farabeuf et al. first described complex MCP dislocation in the thumb but described little about MCP dislocation in the index finger. In 1957, Kaplan described anatomy and pathophysiology of the metacarpal head of the index finger buttonholing into the palm and parameters preventing closed reduction [2, 3].
The metacarpal head forms a condylar type of joint with proximal phalanx with capsule extending from base of the proximal phalanx to neck of the metacarpal. The movements at MCP joint consist of flexion, extension, abduction, adduction, and circumduction [2].
Joint stability and mobility are both guarded by surrounding ligaments and injury to these can result in severe impairment of joint function [1].
Puckering of palmar skin over metacarpal head is pathognomonic of complex MCP dislocation which is similar to puckering of skin in breast carcinoma, making closed reduction difficult [4, 5].
MCP joint dorsal dislocations can be closed reduced by hyperextension of MCP joint deformity then pushing the proximal phalanx back over the metacarpal head. We avoid longitudinal traction as it predisposes to the creation of complex dislocations by the interposition of the proximally torn volar plate in between the MCP joint. The surrounding ligaments get further injured due to traction of already buttonholed metacarpal head [4].
Pain and loss of motion are seen in cases presenting early whereas osteonecrosis and arthritis are seen as late complications of MCP joint dislocation. Premature closure of physis and stunted metacarpal growth can be seen as complications in the immature skeleton. Poor prognosis is seen in delay in diagnosis and treatment, the association of osteochondral fractures, repeated failed attempts at closed reduction, open compound dislocations, and joint stiffness due to prolonged immobilization [6].
MCP joint dislocations are termed simple if they can be reduced with closed manipulations and termed complex if open reduction is necessary. Repeated failed reduction attempts and traction can convert simple dislocation into complex dislocation. This causes buttonholing of metacarpal head between natatory ligament and volar plate distally, proximally by superficial transverse metacarpal ligament, on the ulnar side by flexor tendons with pretendinous bands, and on the radial side by lumbrical [7].
Open reduction with dorsal approach has advantages of reduced risk to volarly displaced neurovascular structures, sufficient exposure for osteochondral fracture management, and adequate visualization of the volar plate. However, this approach requires splitting of the volar plate for optimum reduction, which may delay recovery [8].
An 11 years old male, brought by parents to our casualty with pain in his left index finger after a history of slip and fall on outstretched hand while running 1 h back. There was no history of trauma to any other vital structures. On examination, the patient had swelling and tenderness over MCP joint of the left index finger. Range of motion was restricted and extension deformity at MCP joint (Fig. 1). On X-rays, dorsoulnar dislocation on the second MCP joint is seen (Fig. 2). Patient was immediately posted for emergency surgery after proper pre-anesthetic check-up.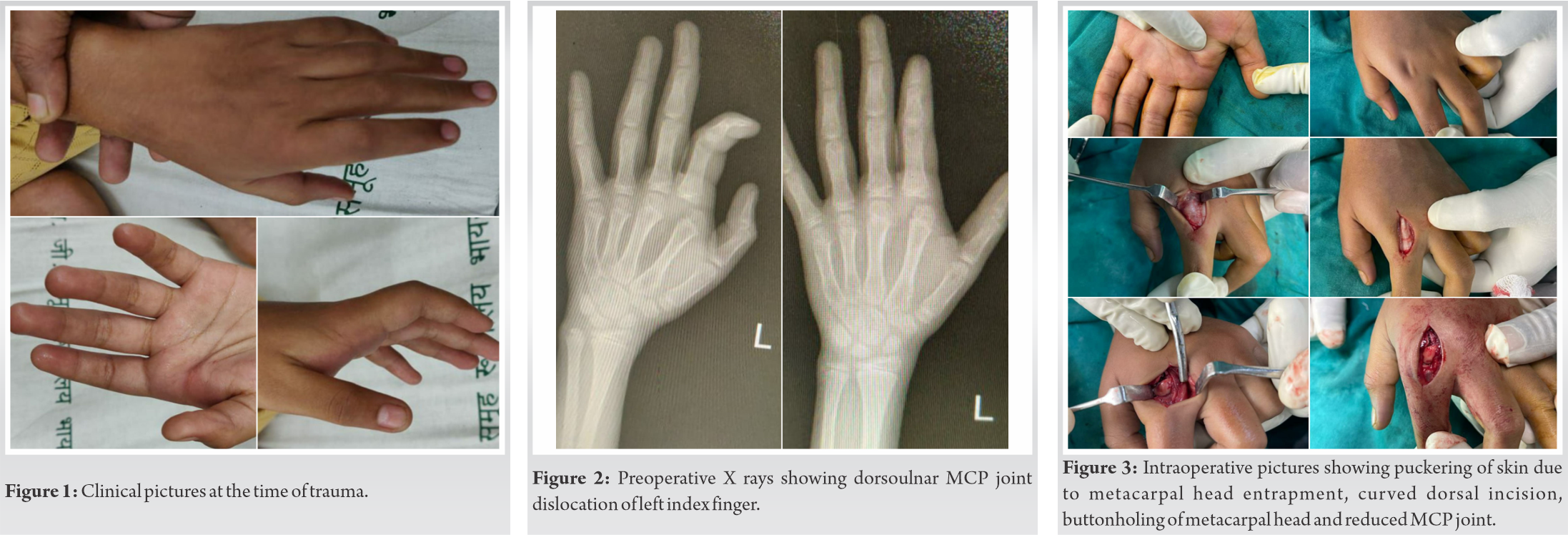
Patient was taken on the operating table under all aseptic precautions and under general anesthesia in supine position. Tourniquet applied. Scrubbing, painting, and draping done. Dorsal curved incision was taken over second MCP joint. Soft tissue dissected and extensor ligaments retracted. Longitudinal capsulotomy done to expose MCP joint. Intervening volar plate is pushed ventrally using freer elevator and joint reduced (Fig. 3). Reduction and stability is checked clinically (Fig. 4) and thorough wound wash is given. Closure done in layers.
Immediate postoperative X-rays show reduced second metacarpophalangeal joint (Fig. 5). Postoperatively cockup slab was given with MCP joint in 30o of flexion for 2 weeks, followed by the use of removable dorsal extension blocking splint for 4 weeks.
Check the dress at postoperative day 3 and suture removal at day 21 was found to be healthy with a good range of motion (Fig. 6).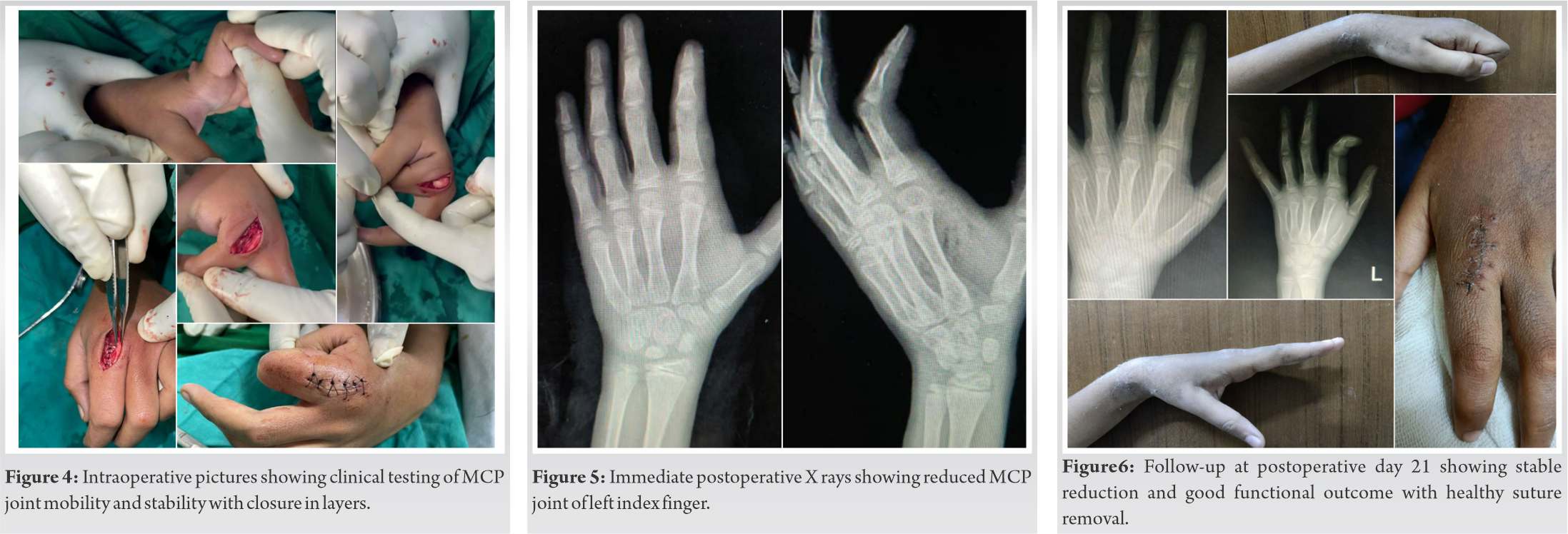
The primary stabilizer of MCP joint in adduction and abduction is radial and ulnar proper collateral ligament which originate from condyles of metacarpal head to the base of the proximal phalanx and distend obliquely from dorsal proximal to ventral distal direction. This act as restraints in MCP flexion. The accessory collateral ligament originates anterior to this ligament and inserts over the volar plate stabilizing the volar plate. This act as static restraint in MCP extension [1, 2].
The volar surface of the MCP joint is facilitated by joint capsule, flexor tendons, and A1 pulley which are placed anterior to the volar plate which stabilizes MCP joint ventrally. The dorsal part of the MCP joint is weakest due to the thin and loose joint capsule dorsally. This predisposes the MCP joint to dorsal dislocations to axial loads after a fall on outstretched hand due to forcible hyperextension. MCP joint of the index finger is most commonly involved [2, 3, 4].
There is a fibrocartilagenous structure known as volar plate ventral to MCP joint which is a rectangular reinforcement thickening of the joint capsule. In hyperextension injuries, the membranous attachment of the volar plate at the proximal metacarpal head is torn [5, 9].
In MCP joint dislocations of the index finger, there is radial displacement of lumbricals and ulnar displacement of flexor tendons. There is a dorsal displacement of natatory ligament and proximal displacement of the superficial transverse metacarpal ligament [6].
In the reduction of simple dislocations, the MCP joint is hyperextended by 90o whereas in complex dislocations only 20o of hyperextension is given and then pressure is directed volarly over the dorsal surface of the base of the proximal phalanx, reducing it over metacarpal head [7].
In dorsal dislocations, there is puckering of palmar skin due to stretching of pretendinous and transverse group of fibers of palmar fascia and skin which are displaced by the metacarpal head. The presence of this sign contraindicates closed reduction [7, 10].
Surgical management of complex MCP joint dislocations consist of volar, dorsal and combined approach [6].
Kaplan had described volar open reduction approach offering advantages like direct visual access to MCP pathoanatomy which helps in surgical extraction and repositioning of volar plate from MCP joint. The neurovascular structures are ventral to lumbrical muscles which are at risk in volar approach to MCP joint along with radial digital nerve. Green and Terry et al. described the division of deep transverse ligament to aid reduction of volar plate [2, 3, 7].
In 1975, Becton et al. described dorsal open reduction approach with advantages like adequate volar plate visualization with avoidance of any digital neurovascular damage and proper reduction of osteochondral fracture of the metacarpal head. However, this approach might require splitting of the volar plate and extensor apparatus longitudinally which may compromise MCP stability [7].
We experienced closed reduction should not be tried in cases of complex dorsal dislocations. The dorsal approach for open reduction of complex MCP dislocation is found to be safe and simple even in hands of inexperienced surgeons which may or may not need division of deep transverse ligament. Volar approach though allows for anatomical reduction of volar plate and MCP joint, poses a risk for volar neurovascular bundle injury, and should be reserved for experienced hand surgeons. Both provide stable MCP joint with good functional outcomes.
Kaplan’s dislocation of the metacarpophalangeal joint should be considered an emergency. Categorizing it as simple or complex based on radiographs and clinical findings is necessary, so that immediate further management can be decided accordingly. Although simple dislocations can be tried for closed reduction. Complex dislocations usually necessitate open reduction, for which the dorsal approach is simple, safe, and effective.
References
- 1.Rozmaryn LM. The collateral ligament of the digits of the hand: Anatomy, physiology, biomechanics, injury, and treatment. J Hand Surg 2017;42:904-15. [Google Scholar]
- 2.Dinh P, Franklin A, Hutchinson B, Schnall SB, Fassola I. Metacarpophalangeal joint dislocation. J Am Acad Orthop Surg 2009;17:318-24. [Google Scholar]
- 3.Barry K, McGee H, Curtin J. Complex dislocation of the metacarpo-phalangeal joint of the index finger: A comparison of the surgical approaches. J Hand Surg Br 1988;13:466-8. [Google Scholar]
- 4.Calfee RP, Sommerkamp TG. Fracture-dislocation about the finger joints. J Hand Surg Am 2009;34:1140-7. [Google Scholar]
- 5.Kaplan EB. Dorsal dislocation of the metacarpophalangeal joint of the index finger. J Bone Joint Surg Am 1957;39:1081-6. [Google Scholar]
- 6.Rubin G, Orbach H, Rinott M, Rozen N. Complex dorsal metacarpophalangeal dislocation: Long-term follow-up. J Hand Surg 2016;41:e229-33. [Google Scholar]
- 7.Vigneswaran V, Bhardwaj P. Dorsal dislocation of the metacarpophalangeal joint of the index finger. J Bone Joint Surg Am 1957;39-A:1081-6. [Google Scholar]
- 8.Patterson RW, Maschke SD, Evans PJ, Lawton JN. Dorsal approach for open reduction of complex metacarpophalangeal joint dislocations. Orthopedics 2008;31:1099. [Google Scholar]
- 9.Light TR, Ogden JA. Complex dislocation of the index metacarpophalangeal joint in children. J Pediatr Orthop 1988;8:300-5. [Google Scholar]
- 10.Meurer WJ, Kronick SL, Lowell MJ, Desmond JS, Mudgal CS. Complex metacarpophalangeal dislocation. Int J Emerg Med 2008;1:227-8. [Google Scholar]







