Chemotherapy is the mainstay of treatment in Pott’s spine, but when neurological deficits are present, the best treatment is debridement and anterior spinal fusion combined with ATT.
Dr. Pranav Gupta, Department of Orthopaedics, Guru Gobind Singh Medical College and Hospital, Faridkot, Punjab - 151203, India.. E-mail: pranavchd88@gmail.com
Introduction: Cervical Pott’s constitutes about 10% of all Pott’s spine cases. In tuberculous spondylitis, initially there occurs destruction of vertebral bodies and further progression may result in adjacent abscesses, leading to cord compression. Objective is to excise the diseased focus and to provide spinal stability.
Case Report: We are presenting 3 rare cases of cervical Pott’s spine with epidural collection at multiple levels in the cervical region without significant vertebral body destruction that were followed up for a period of 1 year postoperatively. Patients underwent single-level corpectomy and decompression from anterior aspect. In all three cases, we were able to decompress the cord and remove all the collections and also achieved spinal stabilization. Patients had a gradual and complete recovery of motor power within 6 months to 1 year after surgery.
Conclusion: Technique used allows accurate visual assessment of the extent of the disease and allows complete decompression of the cord at multiple levels in cervical spine without causing much instability.
Keywords: Antituberculosis therapy, cartridge-based nucleic acid amplification testing, epidural abscess, feeding tube, Pott’s spine.
Pott’s disease accounts for about 1%–2% of all cases of TB [1]. Cervical Pott’s constitutes about 10% of all Pott’s spine cases [1]. Furthermore, cases of cervical Pott’s spine with multiple level involvement are even lesser and collection ventral to the cord is even less common than dorsal collection as pus is more likely to accumulate in larger epidural spaces that contain infection prone fat [2,3]. However, since this disease is very rare in non-endemic zones, it’s diagnosis is delayed. Another cause for delay is that spinal tuberculosis has a subtle onset and advances slowly with average time span between onset of symptoms and clinical presentation being 11 months (4–24 months) [4]. In cases where Pott’s spine is associated with epidural abscess, it is because the host is immunocompromised or there is a history of surgical interventions [5]. In tuberculous spondylitis, initially, there occurs the destruction of vertebral bodies and further progression may result in adjacent abscesses, whereas in pyogenic abscess, vertebral body is usually preserved in early stages [6]. In Pott’s spine cases, decompression plus fixation is done when there is no evidence of neurologic improvement after 6 weeks of antituberculosis therapy (ATT) or the paralysis progresses further despite adequate ATT for over 4 weeks [5]. The objective is to excise the diseased focus, obtain adequate material for histopathology and culture; to provide spinal stability for the alleviation of pain, and to prevent the progression of kyphosis [7]. In carries spine, cord usually gets compressed from the anterior aspect. Therefore, it is necessary to approach the disease anteriorly without which magnitude of the disease will remain unrevealed [8]. This case report describes our experience with three surgical cases of cervical Pott’s disease with epidural collection involving multiple levels in cervical region and also explain an innovative surgical technique which has been used before for drainage of abscess around cervical cord with goal being to cure the disease with minimum residual deformity and without neurologic sequelae [3,9,10,11].
We are presenting 3 rare cases of cervical Pott’s spine with epidural collection at multiple levels in the cervical region without significant vertebral body destruction that had been operated at Guru Gobind Singh Medical College and Hospital, a tertiary referral hospital located in Faridkot, Punjab between 2021 and 2022 and were followed up for a period of 1 year postoperatively. All were males between age group 30–45 years. All three patients had significant neurological deficit in bilateral upper limbs at the time of presentation. Pre- and post-treatment neurologic status was determined using the American Spinal Injury Association impairment scale. The following variables were extracted from the medical records: age at the time of admission, sex, symptoms at presentation, comorbidities, surgical details, preoperative neurologic status, bacteriology, and relevant past medical history. Based on magnetic resonance imaging (MRI), diagnosis of Pott’s spine was made. First patient had a history of chronic alcoholism, second one was HCV positive, and third was HIV positive. First patient had lesion involving vertebrae C2–C7, second one had lesion involving C3–C7, and third patient had lesion involving C1–C5 vertebrae. The following laboratory values at presentation were collected: white blood cell count (cells/mm3), erythrocyte sedimentation rate (ESR) (mm/h), and C-reactive protein (mg/L) (Table 1).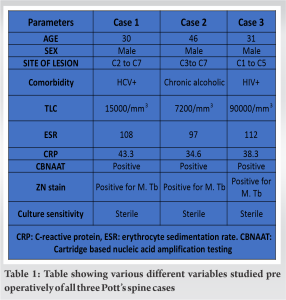 Patients underwent single level corpectomy and decompression from anterior aspect, following which we used a small diameter feeding tube of lumen size 6 French and carefully passed it anterior to the cord both cranially and caudally and drained the collection which was at a distance from the corpectomy site and also irrigated this space with normal saline (NS) using the same tube (Fig. 1).
Patients underwent single level corpectomy and decompression from anterior aspect, following which we used a small diameter feeding tube of lumen size 6 French and carefully passed it anterior to the cord both cranially and caudally and drained the collection which was at a distance from the corpectomy site and also irrigated this space with normal saline (NS) using the same tube (Fig. 1). This was followed by grafting and fusion. Graft of appropriate size was harvested from iliac crest in all three cases. Intraoperatively, biopsy samples were taken and pus samples were sent for Ziehl Neelsen staining, Gram staining, culture, and cartridge-based nucleic acid amplification testing (CBNAAT). Postoperatively, ATT was started, and the patient was given hard Philadelphia collar for providing stability to fixation. At the time of discharge, the patient was allowed sitting and walking with Philadelphia collar. Chemotherapeutic response, disease arrest, and healing processes were assessed by clinical findings, laboratory data (ESR), and serial spine radiographs. All three cases were aptly followed up with radiographs, LFT and ESR in view of continuing ATT. First case was a 30-year-old male. He was HCV positive. The patient had injury of upper back 15 months ago from the time of presentation due to which he had wound for which he took treatment from a quack. After 6 months, the patient developed discharging sinus on upper back, for which incision and drainage were done by the same person. After 4–5 months, the patient started complaining of neck and shoulder pain and weakness of bilateral upper limbs. Power was 2/5 at bilateral shoulder, elbow and wrist with decreased palmar grasp. MRI showed peripherally enhancing collection in anterior epidural space extending from C2 to C7 which was compressing the cord (Fig. 2a). MRI also showed changes involving C2, C3, and C4 vertebra with reduced height of C3 vertebra (Fig. 2b).
This was followed by grafting and fusion. Graft of appropriate size was harvested from iliac crest in all three cases. Intraoperatively, biopsy samples were taken and pus samples were sent for Ziehl Neelsen staining, Gram staining, culture, and cartridge-based nucleic acid amplification testing (CBNAAT). Postoperatively, ATT was started, and the patient was given hard Philadelphia collar for providing stability to fixation. At the time of discharge, the patient was allowed sitting and walking with Philadelphia collar. Chemotherapeutic response, disease arrest, and healing processes were assessed by clinical findings, laboratory data (ESR), and serial spine radiographs. All three cases were aptly followed up with radiographs, LFT and ESR in view of continuing ATT. First case was a 30-year-old male. He was HCV positive. The patient had injury of upper back 15 months ago from the time of presentation due to which he had wound for which he took treatment from a quack. After 6 months, the patient developed discharging sinus on upper back, for which incision and drainage were done by the same person. After 4–5 months, the patient started complaining of neck and shoulder pain and weakness of bilateral upper limbs. Power was 2/5 at bilateral shoulder, elbow and wrist with decreased palmar grasp. MRI showed peripherally enhancing collection in anterior epidural space extending from C2 to C7 which was compressing the cord (Fig. 2a). MRI also showed changes involving C2, C3, and C4 vertebra with reduced height of C3 vertebra (Fig. 2b). 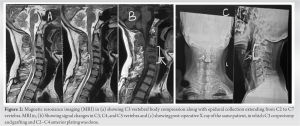 Atlantoaxial interval was maintained. Based on the MRI, provisional diagnosis of Pott’s disease was made. Because of the patient’s precarious neurologic state, it was decided to decompress the cervical cord immediately. Anterior Smith Robinson approach was taken. C3 corpectomy and decompression by the above mentioned method followed by anterior grafting and plating from C2 to C4 (Anterior Cervical Discectomy and Fusion) was done (Fig. 2c). CBNAAT and biopsy came out to be positive and ATT was started to be continued for 18 months. On follow-up at 6 weeks, ESR was 74, hand grip had improved and power at wrist, elbow, and shoulder was 3/5. At 3 months, ESR was 54, power at wrist, elbow and shoulder was 4/5. At 6 months, ESR was 18 and power at wrist, elbow and shoulder was 4+. Cervical spine X-ray film showed evidence of graft fusion with no loss of height (Fig. 2c). At the end of 1 year follow-up, the patient had fully recovered motor function with power at wrist, elbow, and shoulder being 5/5 and remained so in bilateral upper limb. In another case, a 46-year-old male came with neck pain and weakness bilateral upper limbs for 2 weeks which was gradually increasing. He was non-diabetic and non-immunocompromised. However, he had a history of chronic alcoholism. There was a history of multiple falls in the past 4 months. The patient was already on ATT since last 20 days. On examination, power in bilateral shoulder was 2/5, while that in bilateral elbow and wrist was 3/5. Power was 5/5 in bilateral lower limbs. MRI showed involvement of C3 to C7 vertebral bodies with anterior epidural collection extending from C2 to C7 causing spinal canal stenosis and compression of the exiting nerve roots (Fig. 3a).
Atlantoaxial interval was maintained. Based on the MRI, provisional diagnosis of Pott’s disease was made. Because of the patient’s precarious neurologic state, it was decided to decompress the cervical cord immediately. Anterior Smith Robinson approach was taken. C3 corpectomy and decompression by the above mentioned method followed by anterior grafting and plating from C2 to C4 (Anterior Cervical Discectomy and Fusion) was done (Fig. 2c). CBNAAT and biopsy came out to be positive and ATT was started to be continued for 18 months. On follow-up at 6 weeks, ESR was 74, hand grip had improved and power at wrist, elbow, and shoulder was 3/5. At 3 months, ESR was 54, power at wrist, elbow and shoulder was 4/5. At 6 months, ESR was 18 and power at wrist, elbow and shoulder was 4+. Cervical spine X-ray film showed evidence of graft fusion with no loss of height (Fig. 2c). At the end of 1 year follow-up, the patient had fully recovered motor function with power at wrist, elbow, and shoulder being 5/5 and remained so in bilateral upper limb. In another case, a 46-year-old male came with neck pain and weakness bilateral upper limbs for 2 weeks which was gradually increasing. He was non-diabetic and non-immunocompromised. However, he had a history of chronic alcoholism. There was a history of multiple falls in the past 4 months. The patient was already on ATT since last 20 days. On examination, power in bilateral shoulder was 2/5, while that in bilateral elbow and wrist was 3/5. Power was 5/5 in bilateral lower limbs. MRI showed involvement of C3 to C7 vertebral bodies with anterior epidural collection extending from C2 to C7 causing spinal canal stenosis and compression of the exiting nerve roots (Fig. 3a).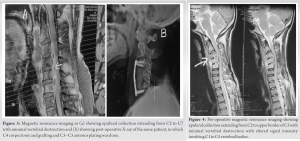 However, there was no significant vertebral body destruction as height of body was maintained. Atlantoaxial joint space was normal. In March 2021, the patient underwent C4 corpectomy and decompression followed by anterior grafting and plating from C3 to C5 (ACDF) (Fig. 3b). ATT was started after the CBNAAT report. The patient had improved power in bilateral arm at 6-week follow-up with power being 3/5 at bilateral shoulder and 4/5 at elbow and wrist. On follow-up 3 month later, ESR was 56 and power at wrist, elbow and shoulder was 4/5. At 6 months after surgery, ESR was 16, and the patient had fully recovered motor function with power at wrist, elbow, and shoulder being 5/5 and remained so in bilateral upper limb. At 6 months, cervical spine X-ray film showed evidence of graft fusion with no loss of height. The patient is still under follow-up and on ATT. In other case, a 31-year-old male presented with neck pain and weakness in bilateral upper limbs of 2-month duration. The patient was HIV positive. Power was 2/5 at bilateral shoulder, elbow, and wrist with poor hand grip. History of fever, loss of appetite, and loss of weight was present. Another doctor who had advised ATT to the patient based on MRI which patient had been taking for the past 2 months; however, there was no improvement in symptoms. MRI showed epidural collection extending from C2 to upper border of C5 vertebra causing scalloping and compression of cord (Fig. 4). There was evidence of altered signal intensity involving C1 to C5 vertebral bodies but no vertebral body destruction (Fig. 4). In August 2021, the patient underwent C4 corpectomy and decompression by the same method, followed by anterior grafting and plating from C3 to C5 (ACDF). ATT was continued after the positive CBNAAT report. At 6-week follow-up, power had improved in bilateral arm with power being 3/5 at bilateral shoulder and 3/5 at elbow and wrist. On follow-up 3 months later, ESR was 47 and power at wrist, elbow, and shoulder was 4/5. At 6 months after surgery, ESR was 32 and patient had shown further improvement in motor power. At 9 months, ESR was 12 and motor power at wrist, elbow, and shoulder was 5/5 and remained so in bilateral upper limb. The patient continues to be under our follow-up and on ATT. In all three cases, we were able to decompress the cord and were able to remove all the collections and caseous material and also achieved spinal stabilization. All three patients had a gradual and complete recovery of motor power within 6 months to 1 year after surgery. There was no recurrence in this period. We had no major complications. Patients did have pain at the operative site postoperatively which gradually subsided. All three cases received ATT postoperatively. All three cases showed gradual healing on subsequent follow-ups based on plain radiographs and MRI done postoperatively showing good fusion of graft with the adjacent vertebrae. Overall patients are free of pain and made a good recovery in terms of neurological deficit. Patients are still under regular follow-up periodically with monthly LFT and ESR reports as patients are on ATT.
However, there was no significant vertebral body destruction as height of body was maintained. Atlantoaxial joint space was normal. In March 2021, the patient underwent C4 corpectomy and decompression followed by anterior grafting and plating from C3 to C5 (ACDF) (Fig. 3b). ATT was started after the CBNAAT report. The patient had improved power in bilateral arm at 6-week follow-up with power being 3/5 at bilateral shoulder and 4/5 at elbow and wrist. On follow-up 3 month later, ESR was 56 and power at wrist, elbow and shoulder was 4/5. At 6 months after surgery, ESR was 16, and the patient had fully recovered motor function with power at wrist, elbow, and shoulder being 5/5 and remained so in bilateral upper limb. At 6 months, cervical spine X-ray film showed evidence of graft fusion with no loss of height. The patient is still under follow-up and on ATT. In other case, a 31-year-old male presented with neck pain and weakness in bilateral upper limbs of 2-month duration. The patient was HIV positive. Power was 2/5 at bilateral shoulder, elbow, and wrist with poor hand grip. History of fever, loss of appetite, and loss of weight was present. Another doctor who had advised ATT to the patient based on MRI which patient had been taking for the past 2 months; however, there was no improvement in symptoms. MRI showed epidural collection extending from C2 to upper border of C5 vertebra causing scalloping and compression of cord (Fig. 4). There was evidence of altered signal intensity involving C1 to C5 vertebral bodies but no vertebral body destruction (Fig. 4). In August 2021, the patient underwent C4 corpectomy and decompression by the same method, followed by anterior grafting and plating from C3 to C5 (ACDF). ATT was continued after the positive CBNAAT report. At 6-week follow-up, power had improved in bilateral arm with power being 3/5 at bilateral shoulder and 3/5 at elbow and wrist. On follow-up 3 months later, ESR was 47 and power at wrist, elbow, and shoulder was 4/5. At 6 months after surgery, ESR was 32 and patient had shown further improvement in motor power. At 9 months, ESR was 12 and motor power at wrist, elbow, and shoulder was 5/5 and remained so in bilateral upper limb. The patient continues to be under our follow-up and on ATT. In all three cases, we were able to decompress the cord and were able to remove all the collections and caseous material and also achieved spinal stabilization. All three patients had a gradual and complete recovery of motor power within 6 months to 1 year after surgery. There was no recurrence in this period. We had no major complications. Patients did have pain at the operative site postoperatively which gradually subsided. All three cases received ATT postoperatively. All three cases showed gradual healing on subsequent follow-ups based on plain radiographs and MRI done postoperatively showing good fusion of graft with the adjacent vertebrae. Overall patients are free of pain and made a good recovery in terms of neurological deficit. Patients are still under regular follow-up periodically with monthly LFT and ESR reports as patients are on ATT.
Majority of spinal epidural abscess (SEA) are related to a distant infectious focus such as dental abscesses, pharyngitis, or skin and soft-tissue infections [6,12]. Previous surgical interventions also predispose toward the development of SEA [5]. First patient in our study had a history of abscess in upper back. Other predisposing factors include comorbidities such as diabetes, immunodeficiency, and intravenous drug abuse [5]. In the present study, the first patient was HCV positive due to a history of IV drug abuse, second patient had a history of chronic alcoholism, and third patient was HIV positive. There was no history of pulmonary tuberculosis in any patient. SEA commonly occurs in association with vertebral destruction in tuberculosis spine rather than occurring alone [13]. Tuberculous spondylitis typically initially involves destruction of vertebral bodies. Further spread may result in adjacent abscesses, whereas in pyogenic abscess, vertebral body is usually preserved in early stages [6] Chang et al. also concluded that vertebral body was damaged more severely in tuberculous spondylitis than in pyogenic spondylitis [14]. However, in our cases, though epidural collection was present at multiple consecutive levels in cervical spine, but vertebral bodies were more or less intact due to which diagnosis was going more toward pyogenic infection. However, intra-operative samples came out to be positive for TB, whereas bacterial cultures were negative. As tuberculous spondylitis advances, there occurs progressive vertebral body collapse, resulting in kyphosis and gibbus formation which leads to cord compression. Formation of SEA causes further cord compression [15]. In our study, deficit was due to cord compression by abscess and not due to vertebral destruction as vertebral height was more or less maintained in all three cases. Cervical region is a much smaller epidural space compared to midthoracic, and lumbosacral regions due to which it is less prone to infection explaining the relatively fewer incidence of upper cervical epidural abscess [5]. Furthermore, epidural extension and SEA formation have been reported to be observed more in tuberculous spondylitis [13]. Epidural collection was present in all three cases. From Hong Kong, Hsu and Leong diagnosed 1100 cases of Pott’s disease, out of which only 4.2% involved the cervical spine [16]. In the United States, approximately 4000 cases of extrapulmonary TB are identified every year out of which cervical spine was involved only in 0.4% to 1.2% of the cases [17]. In developing countries like India, diagnosis of Pott’s disease is also usually delayed because of illiteracy and poor medical facilities at grassroots level. Delay ranges from 3 to 12 months due to which many patients have already developed neurological changes [13]. All three patients in our study also presented with a delay of 4–6 months due to which neurological deficit had already occurred. Furthermore, the onset of neurologic deficit in all three cases was slow and symmetrical which is usually the case in Pott’s spine [16]. In spinal tuberculosis, operative intervention is required if there is neurological deterioration at any stage which was there in all three cases [7]. Roy et al. have also proposed that if severe neurologic compromise is present at the time of diagnosis, or if less prominent neurologic signs do not improve within 6 weeks of ATT, then surgical debridement and anterior spinal fusion using an iliac crest bone graft should be done [18]. In 1991, Slater et al. also concluded that, when neurologic deficits are present, the best treatment is debridement and anterior spinal fusion combined with ATT [17]. Elsawaf in his study also observed better results in surgically treated cases [19]. The same principal was followed in all three cases. Surgical treatment cuts the period of treatment from years to months and also prevents gross vertebral destruction and development of deformity [20]. Furthermore, in Pott’s spine, cord usually gets compressed from the anterior aspect. Therefore it is necessary to approach the disease anteriorly as it completely unveils the pathology of the disease and also helps in complete removal of diseased tissue [8]. In our study, spine was approached anteriorly through the Southwick-Robinson approach in all three cases. We did corpectomy only at single level and then passed small size feeding tube anterior to the cord both cranially and caudally to drain rest of the collection, followed by irrigation of the space with NS using the same feeding tube. In the first patient, we did C3 corpectomy, and in the second and third patients, we did C4 corpectomy followed by introduction of an anterior graft harvested from iliac crest and plating anteriorly from C2 to C4 and C3-C5, respectively. Iliac crest bone grafts are preferable to rib or fibular strut grafts as cancellous bone is not strong enough, and rib transplants have insufficient end-bearing surfaces [6]. This technique did effective decompression and eliminated the focus of infection without causing much instability. This technique though has been used previously by Muzii et al., Fujii et al., Kim et al., and Kotheeranurak et al., but it is worth mentioning that Muzii et al. inserted radiopaque silicon spinal catheter 1.5 mm in diameter into anterior epidural space using fluoroscopy [3,9,10,11], Fujii et al. also did the decompression of cord in dorsolumbar region using 5 Fr catheter from posterior approach under fluoroscopic guidance [9], Kim et al. drained epidural abscess located in thoracic region through posterior approach by doing laminectomy using same technique [10]. and Kotheeranurak et al. used this technique to drain epidural abscess from cervical region from anterior aspect, but here they used endoscope guided 8F nasogastric tube [11]. In our study, we did not have the luxury of having endoscope or fluoroscopy-guided approach to drain cervical abscess from anterior aspect. We drained the abscess by passing feeding tube only. Hence, we had to rely only on our surgical skills. However, there is certain limitation to this technique such as it is not recommended when solid granulation tissue is encountered instead of liquid pus. Furthermore, this technique has a long and steep learning curve.
Diagnosis of tuberculosis of cervical spine is often delayed. Chemotherapy is the mainstay of treatment, but when neurologic deficits are present, the best treatment is debridement and anterior spinal fusion combined with ATT. Technique used in this study allows complete decompression of the cord at multiple levels in cervical spine without causing much instability. This technique can thus serve as guide for future surgeries where decompression needs to be done at multiple levels in cervical spine; however, since we are passing the tube without any image guidance, it should be done only by experienced surgeons.
Since the technique used in this study allows complete decompression of the cord at multiple levels in cervical spine without causing much instability, it can serve as a guide for emerging spine surgeons for future surgeries.
References
- 1.Okwudire EG, Ezenwugo UM, Ugwoegbu JU, Okoro CA, Isiozor I. Atypical presentation of cervical Pott’s disease: A case report. J Tuberc Res 2021;9:211-8. [Google Scholar | PubMed]
- 2.Darouiche RO. Spinal epidural abscess. N Engl J Med 2006;355:2012-20. [Google Scholar | PubMed]
- 3.Muzii VF, Mariottini A, Zalaffi A, Carangelo BR, Palma L. Cervical spine epidural abscess: Experience with microsurgical treatment in eight cases. J Neurosurg Spine 2006;5:392-7. [Google Scholar | PubMed]
- 4.Ramani PS, Sharma A, Jituri S, Muzumdar DP. Anterior instrumentation for cervical spine tuberculosis: An analysis of surgical experience with 61 cases. Neurol India 2005;53:83-9. [Google Scholar | PubMed]
- 5.Al-Hourani K, Al-Aref R, Mesfin A. Upper cervical epidural abscess in clinical practice: Diagnosis and management. Global Spine J 2016;6:383-93. [Google Scholar | PubMed]
- 6.Griffith JF, Kumta SM, Leung PC, Cheng JC, Chow LT, Metreweli C. Imaging of musculoskeletal tuberculosis: A new look at an old disease. Clin Orthop Relat Res 2002;398:32-9. [Google Scholar | PubMed]
- 7.Moon MS, Moon JL, Kim SS, Moon YW. Treatment of tuberculosis of the cervical spine: Operative versus nonoperative. Clin Orthop Relat Res 2007;460:67-77. [Google Scholar | PubMed]
- 8.Hodgson AR, Stock FE. Anterior spinal fusion a preliminary communication on the radical treatment of Pott’s disease and Pott’s paraplegia. Br J Surg 1956;44:266-75 [Google Scholar | PubMed]
- 9.Fujii M, Shirakawa T, Shime N, Kawabata Y. Successful treatment of extensive spinal epidural abscess with fluoroscopy-guided percutaneous drainage: A case report. JA Clin Rep 2020;6:4. [Google Scholar | PubMed]
- 10.Kim CY, Kim P, Ju CI, Kim SW. Treatment of extensive spinal epidural abscess with skipped laminotomy using a pediatric feeding tube: A case report. Korean J Neurotrauma 2021;17:193-8. [Google Scholar | PubMed]
- 11.Kotheeranurak V, Jitpakdee K, Singhatanadgige W, Limthongkul W, Yingsakmongkol W, Kim JS. Anterior transcorporeal full-endoscopic drainage of a long-span ventral cervical epidural abscess: A novel surgical technique. N Am Spine Soc J 2021;5:100052. [Google Scholar | PubMed]
- 12.Baker AS, Ojemann RG, Swartz MN, Richardson EP Jr. Spinal epidural abscess. N Engl J Med 1975;293:463-8. [Google Scholar | PubMed]
- 13.Lee KY. Comparison of pyogenic spondylitis with tuberculous spondylitis. Asian Spine J 2014;8:216-23. [Google Scholar | PubMed]
- 14.Chang MC, Wu HT, Lee CH, Liu CL, Chen TH. Tuberculous spondylitis and pyogenic spondylitis: Comparative magnetic resonance imaging features. Spine (Phila Pa 1976) 2006;31:782-8. [Google Scholar | PubMed]
- 15.Njoku CH, Makuside MA, Ezunu EO. Experiences in management of Pott’s paraplegia and paraparesis in medical wards of usmanu danfodiyo university teaching Hospital, Sokoto, Nigeria. Ann Afr Med 2007;6:22-5. [Google Scholar | PubMed]
- 16.Hsu LC, Leong JC. Tuberculosis of the lower cervical spine (C2 to C7). A report on 40 cases. J Bone Joint Surg Br 1984;66:1-5. [Google Scholar | PubMed]
- 17.Slater RR Jr., Beale RW, Bullitt E. Pott’s disease of the cervical spine. South Med J 1991;84:521-3. [Google Scholar | PubMed]
- 18.Roy TM, Giles C, Mendieta J, Ossorio MA. Pott’s disease in Kentucky: Diagnosis and treatment. J Ky Med Assoc 1988;86:499-502. [Google Scholar | PubMed]
- 19.Elsawaf A. Outcome of surgical versus conservative management of cervical spine myelopathy secondary to cervical tuberculosis. Neurosurg Rev 2013;36:621-8 [Google Scholar | PubMed]
- 20.Fang D, Leong JC, Fang HS. Tuberculosis of the upper cervical spine. J Bone Joint Surg Br 1983;65:47-50 [Google Scholar | PubMed]









