Clinicians should consider osteonecrosis in the differential diagnosis of persistent ankle pain, even in the absence of obvious risk factors or associated symptoms, and choose surgical treatment after failed conservative management to prevent joint line involvement and collapse.
Joeffroy N Otayek, Department of Orthopedics and Traumatology, Faculty of Medicine, Lebanese American University, Beirut, Lebanon. E-mail: joeffroy@gmail.com
Introduction: Osteonecrosis (ON) is a serious pathological condition that can affect weight-bearing areas of the lower limbs, including the distal tibia. Although trauma is a common cause of ON, the condition has multiple possible etiologies. ON has been associated with a range of factors, including trauma, medication use, alcoholism, and vascular disease. Interruption of blood flow to a particular bone region is the first step in the pathophysiology of ON. Conservative management is typically indicated in the early stages of ON, but joint-preserving procedures may be necessary in cases where conservative treatment fails.
Case Report: This article presents a case of bilateral ON of the distal tibia in a 38-year-old female patient without a history of trauma or identifiable risk factors. The patient was initially managed conservatively but ultimately underwent joint-preserving surgery due to treatment failure.
Conclusion: Joint-preserving procedures should be considered in cases of early-stage distal tibia ON that do not respond to conservative management to prevent joint collapse. This case highlights the importance of considering ON as a possible diagnosis even in the absence of identifiable risk factors or trauma.
Keywords: Distal tibia, osteonecrosis, avascular necrosis, atraumatic, bilateral.
Osteonecrosis (ON), also known as avascular necrosis (AVN), is a condition characterized by the death of bone cells, leading to the destruction of osseous tissue [1]. This cellular destruction results from a vascular insult that eventually causes bone infarction and architectural collapse of the articular surface [2]. The long-term effects of ON range from a benign clinical course to persistent pain and discomfort [3]. Clinically, a patient experiences symptoms similar to arthralgias at an early stage. Although AVN commonly affects anatomical sites such as the femoral head, talus, and humeral head, cases of ankle involvement are rare, and the talus is the most commonly affected location [1,4]. ON can have various causes, with trauma being the most frequent [5]. However, non-traumatic etiologies such as sickle cell disease, metabolic issues, vascular or rheumatologic conditions, infections, alcoholism, corticosteroid (CS) use, hyperbaric events, and coagulation deficiencies can also be linked to the condition [1].
Here, we present the case of a previously healthy, non-smoker, and non-alcoholic woman with an unusual presentation of bilateral non-traumatic ankle pain due to ON of the distal tibia.
A 38-year-old non-smoker, non-alcoholic previously healthy woman presented with a complaint of bilateral ankle pain, with the left ankle being more affected, which had been present for the past 5 years. Medical history is positive only for 10 years of hypothyroidism treated with Euthyrox. Her pain started intermittently and gradually became constant, radiating to both feet and knees and was exacerbated by ambulation, with partial relief with non-steroidal anti-inflammatory drugs (NSAIDs). The patient also reported severe night pains. Physical examination revealed tenderness over the left distal tibia with a painful range of motion of both ankles, more so on the left. No swelling, redness, or edema were observed. Bilateral ankle radiographs were obtained, which showed a small radiolucent circumferential area suggestive of ON of the left distal tibia (Fig. 1).
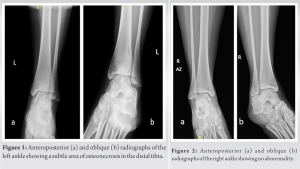 Radiographs of the right distal tibia were unremarkable (Fig. 2).
Radiographs of the right distal tibia were unremarkable (Fig. 2).
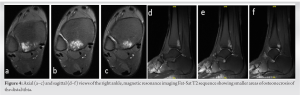
Bilateral ankles magnetic resonance imaging (MRIs) was then ordered showing a 3 × 2-cm area of ON involving the left distal tibia/tibial plafond with extension of edema onto the medial malleolus (Fig. 3),
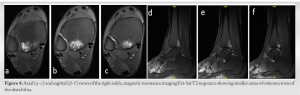 as well as a patchy subchondral well-delineated geographical low T1 and high T2 fat sat signal ON involving the right distal tibia posteriorly and laterally measuring 1.5 × 1.1 cm of transverse axis and around 2.5 cm of length (Fig. 4).
as well as a patchy subchondral well-delineated geographical low T1 and high T2 fat sat signal ON involving the right distal tibia posteriorly and laterally measuring 1.5 × 1.1 cm of transverse axis and around 2.5 cm of length (Fig. 4).
 Thorough investigations were conducted to rule out the presence of any systemic disease. Comprehensive laboratory tests, including sickle cell screening, lipid profile analysis, and screening for coagulopathies, all yielded negative results.
Thorough investigations were conducted to rule out the presence of any systemic disease. Comprehensive laboratory tests, including sickle cell screening, lipid profile analysis, and screening for coagulopathies, all yielded negative results.
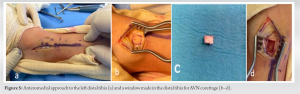
The patient, having failed conservative management including partial weight bearing and analgesics, opted for surgery for her left ankle due to severe pain and a painful ambulation. Using an anteromedial approach to the left distal tibia (Fig. 5a), and after careful dissection, a window was made on the anterior aspect of the distal tibia (Fig. 5b-d) through which the AVN was debrided with curetted (Fig. 6).
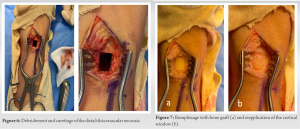 The bone defect was then irrigated using normal saline solution and hydrogen peroxide. Synthetic bone graft was then inserted into the defect for remplissage followed by reapplication of the window that was previously cut (Fig. 7).
The bone defect was then irrigated using normal saline solution and hydrogen peroxide. Synthetic bone graft was then inserted into the defect for remplissage followed by reapplication of the window that was previously cut (Fig. 7).
 The distal tibia was then fixed with a Mesh Plate and eight screws (Fig. 8) with satisfactory radiologic control (Fig. 9). A below-knee posterior splint was applied postoperatively on the left lower limb. The pathology report came back positive for ON, with an absence of malignancy.
The distal tibia was then fixed with a Mesh Plate and eight screws (Fig. 8) with satisfactory radiologic control (Fig. 9). A below-knee posterior splint was applied postoperatively on the left lower limb. The pathology report came back positive for ON, with an absence of malignancy.
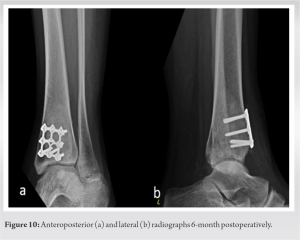 At 6-month follow-up, the patient was pain-free, walking full weight bearing with a below-knee boot. Radiographs show satisfactory bone growth at the level of the surgery (Fig. 10).
At 6-month follow-up, the patient was pain-free, walking full weight bearing with a below-knee boot. Radiographs show satisfactory bone growth at the level of the surgery (Fig. 10).
This case report presents the unusual diagnosis of bilateral distal tibia ON in a young lady who complained of bilateral ankle pain. ON can occur due to traumatic and atraumatic events [2]. The femoral head, talus, and proximal humerus are the most commonly affected sites for post-traumatic ON. However, distal tibial fractures in children can also lead to ON, albeit infrequently [1]. ON affecting the ankle is rare, with the talus being the most frequently affected site compared to the distal tibia [2]. To the best of our knowledge, bilateral distal tibia ON is particularly uncommon, and idiopathic cases are even rarer. ON can be asymptomatic or cause gradually worsening discomfort, leading to severe pain, bone fracture, and joint destruction, eventually resulting in disability and loss of productivity [2,5]. In our case, the patient complained only of bilateral ankle pain. It is important to note that bilateral involvement is possible, and therefore, contralateral ankle radiological assessment is recommended [6].
The precise cause of ON remains unknown, although several factors are thought to contribute to its development. These factors include interruption of blood flow, ischemia, coagulopathies in the bony microcirculation, and mechanical forces [2]. ON is a multifactorial illness with numerous risk factors, including steroids, alcohol, SLE, antiphospholipid syndrome, trauma, sickle cell disease, Gaucher disease, decompression disease, transplantation, hereditary thrombophilia, radiation treatment, and HIV infection [7]. Big bone sections with weak blood flow, such as intraarticular or regions with few soft-tissue attachments, are more susceptible to ON [8]. The distal tibia is particularly vulnerable due to its precarious blood circulation, which increases the risk of ischemic damage after trauma [9]. The medial distal tibia is known to be more vascularized, while the lateral distal tibial epiphysis is considered a “watershed” area for blood circulation. The lateral tibia is nourished by periosteal branches from the tibialis anterior artery and perforating branch of the peroneal artery in 2/3 of cases, and by the tibialis anterior artery solely in 1/3 of cases [5]. Preservation of the distal tibial blood supply is essential to avoid bone infarct. An alternative explanation for the onset of a bone infarct is the absence of collateral microcirculation in conjunction with traumatic damage [1]. CS is the most common factor linked to the development of non-traumatic ON. Non-traumatic ON is mostly associated with CS, and it is crucial to note that the exact pathophysiology remains unclear [2]. The use of steroids has frequently been implicated as a contributing factor to bone AVN, most commonly in the femoral head. Uncertain pathogenesis makes ON a dangerous disease that can affect various skeletal areas with or without a history of trauma [6]. Atraumatic distal tibia ON in adults is rare, with postulated explanations including elevated bone endovascular pressure, vascular thromboembolism, and coagulation problems. Protracted course of steroid therapy induces osteoblast and osteoclast programmed cell death, reduces bone recycling, and decreases osteocyte lifespan. The alteration of adipogenesis and lysis, resulting in vascular fatty emboli of the bone microcirculation, is another hypothesized explanation of ON in patients treated with steroids [2]. Furthermore, bisphosphonates have been linked to ON, mostly in the jaw [4]. Further research is required to fully understand ON’s pathogenesis, as the combined impact of metabolic variables, genetic susceptibility, and various factors influencing blood flow are thought to be the cause [2].
Computed tomography scan and MRI imaging modalities are useful in making the diagnosis of AVN after standard weight-bearing radiographic images. MRI is essential for establishing the diagnosis of AVN with near 99% of sensitivity and specificity, particularly in early-stage lesion identification [2,5]. The Ficat and Arlet classification, which was initially applied to the femoral head, may be applied to any affected bone and is the most popular radiological grading technique. Simple radiography can be used to detect collapsed articular surfaces. The typical MRI presentation of ON is a segmental region of hypo signal intensity in the bone surrounded by a low signal intensity boundary, and a double line sign may also be visible. In some cases, distinguishing distal tibia AVN from tumors may be challenging, particularly when it manifests as a zone of dispersed hypo signal intensity [7]. MRI findings of ON may include widespread edema of the distal tibia, local coiled lines with an outside dark sclerotic aspect, central hypersignal intensity on T2, and osteochondral disintegration [5]. Our patient’s MRI scans reveal extensive bilateral ON of the distal tibia, with more severe involvement on the left side. There are several treatment options for ON of the distal tibia, but most of the available data has been focused on the femoral head, with only limited information reported regarding lower leg ON. Conservative treatment is the first option, which includes rest, painkillers, and NSAIDs. However, these measures have produced only mediocre outcomes [4]. In the early stages, this uncommon injury can be managed without surgery, but careful radiographic surveillance and MRI scans are recommended to verify bone regrowth and viability in the distal tibia [10]. Other conservative therapies include electromagnetic stimulation, hyperbaric oxygen therapy, shock waves, and physiotherapy [4]. Patients who do not respond to conservative management are the best candidates for surgical intervention. Joint-preserving procedures such as core decompression, vascularized, and neovascularized bone grafting are the initial surgical options for pre-collapse lesions [2]. Core decompression is usually implemented during the initial stages of ankle ON as a pain-reduction therapy and to delay the joint’s destruction [4]. Percutaneous drilling, a variant of core decompression, can also be used to provide channels for the necrotic segment’s revascularization [8]. However, compared to the femoral head and distal femur, the diseased part of the distal tibia is relatively small, which makes surgical management more challenging [4].
Core decompression has shown promising results in ankle ON compared to non-operative management [11]. As the disease progresses, the usual geometry of the ankle joint collapses, resulting in an inefficient distribution of stress across the articular surface. Thus, surgical reconstruction may be required to restore the lower extremity’s weight-bearing architecture and lessen the disease burden on the patient. While total ankle arthroplasty has been a relative contraindication for ON due to the need for bone ingrowth into implants and the typically active and non-elderly candidate patients, ankle arthrodesis is commonly recommended for young employees due to its durability, long-term outcomes, and consistent reliability [5]. Thus, ankle fusion or joint replacement might be the final option in such advanced cases of distal tibia ON. Therefore, early diagnosis is crucial to ON treatment without sacrificing the ankle joint [6]. In our case, we opted for excision of the necrotic tissue and filling with a bone graft to provide a supportive osteoinductive and osteoconductive matrix for bone growth and fill the necrotic area while keeping the joint intact. We believe that this technique would provide satisfactory support to the joint line, prevent collapse, and reduce the risk of ankle osteoarthritis and complications. As mentioned earlier, ON of the ankle is an uncommon occurrence, and bilateral distal tibia involvement is extremely rare. Our case is unique in that the patient presented with an unusual and persistent bilateral ankle pain, ultimately, leading to the diagnosis of bilateral distal tibia ON, without any obvious risk factors or associated symptoms.
ON is a complex condition with various etiologies that can affect any bone in the body. Although it most commonly involves the femoral head, talus, and humeral head, ON of the ankle is rare, and bilateral distal tibia involvement is even more uncommon. The case presented here underscores the importance of considering ON in the differential diagnosis of persistent ankle pain, even in the absence of obvious risk factors or associated symptoms. Clinicians should remain vigilant and consider a thorough radiological assessment of both ankles since bilateral involvement is quite possible. After the failure of conservative management, operative management should be considered to provide adequate support and prevent joint line involvement and collapse.
ON of the distal tibia can be a rare cause of ankle pain, and surgical intervention in the form of curettage and bone grafting should be considered if conservative management proves ineffective, as this can help prevent joint line involvement and collapse.
References
- 1.Ropri A, Badar Z, Khan A, Murtaza H, Jetty S, Chu J, et al. Pathogenesis and radiological findings in rare case of Salter Harris Type I distal tibial fracture with associated osteonecrosis in the paediatric population. J Ayub Med Coll Abbottabad 2018;30:463-7. [Google Scholar | PubMed]
- 2.Oesman I, Adhimukti DH. Osteonecrosis of the distal tibia in systemic lupus erythematosus: A rare case report. Int J Surg Case Rep 2020;77:126-8 [Google Scholar | PubMed]
- 3.Pugely AJ, Nemeth BA, McCarthy JJ, Bennett DL, Noonan KJ. Osteonecrosis of the distal tibia metaphysis after a Salter-Harris I injury: A case report. J Orthop Trauma 2012;26:e11-5. [Google Scholar | PubMed]
- 4.McLeod JM, Ng A, Kruse DL, Stone PA. Nontraumatic osteonecrosis of the distal tibia: A case presentation and review of the literature. J Foot Ankle Surg 2017;56:158-66. [Google Scholar | PubMed]
- 5.Cinats DJ, Stone T, Viskontas D, Apostle K. Osteonecrosis of the distal tibia after pilon fractures. Foot Ankle Surg 2020;26:895-901. [Google Scholar | PubMed]
- 6.Issa K, Naziri Q, Kapadia BH, Lamm BM, Jones LC, Mont MA. Clinical characteristics of early-stage osteonecrosis of the ankle and treatment outcomes. J Bone Joint Surg Am 2014;96:e73. [Google Scholar | PubMed]
- 7.Choi SM, Rad DR, Carpenter EC. An unusual case study of idiopathic bilateral deep vein thrombosis and osteonecrosis of the left distal tibia in an 11-year-old girl. J Orthop Case Rep 2022;12:56-60. [Google Scholar | PubMed]
- 8.Rajagopalan S, Lloyd J, Upadhyay V, Sangar A, Taylor HP. Osteonecrosis of the distal tibia after a pronation external rotation ankle fracture: Literature review and management. J Foot Ankle Surg 2011;50:445-8. [Google Scholar | PubMed]
- 9.Baldassarre RL, Pathria MN, Huang BK, Dwek JR, Fliszar EA. Periosteal stripping in high ankle sprains: An association with osteonecrosis. Clin Imaging 2020;67:237-45. [Google Scholar | PubMed]
- 10.Bhattacharjee A, Singh J, Mangham DC, Freeman R. Osteonecrosis of the distal tibial metaphysis after Salter-Harris Type-2 injury: A case report. J Pediatr Orthop B 2015;24:366-9. [Google Scholar | PubMed]
- 11.Gilmor R, Chen Z, Mont MA, Delanois RE, Nace J. Core decompression versus nonoperative management of osteonecrosis of the ankle: A systematic review. Surg Technol Int 2022;41:sti41/1619. [Google Scholar | PubMed]











