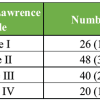
The utilization of the mid-resection workflow in robotic-assisted total knee arthroplasty for patients with complex deformities not only provides surgeons with enhanced ease but also provides a better implant position, thereby improved patient outcome.
Dr. J.S.S.N Manohar, Sunshine Bone and Joint Institute, Secunderabad, Telangana, India. E-mail: jssnmanohar.1992@gmail.com
Introduction: With the growing prevalence of robotic-assisted total knee arthroplasty (RATKA), the significance of effectively addressing complex deformities using this approach is gaining widespread recognition. This article underscores the importance of a novel mid-resection workflow specifically tailored for RATKA in cases with complex deformities.
Case Report: A 58-year-old female patient diagnosed with severe osteoarthritis in both knees and a stiff left knee underwent RATKA utilizing a mid-resection workflow. The surgery resulted in favorable intraoperative stability and achieved a satisfactory range of motion. Follow-up at the 1-year post-operative mark demonstrated a range of movement of 110° and a positive functional outcome for the patient.
Conclusion: Severe knee arthritis with flexion deformity represents a common condition encountered in surgical practice. The advent of RATKA has provided us with an opportunity to assess and establish the effectiveness of mid-resection workflow in managing such cases.
Keywords: Stiff knee, mid-resection workflow, osteoarthritis, robotic assisted.
After undergoing total knee arthroplasty, patients typically expect to experience pain relief, improved ability to walk, and increased range of motion. However, post-operative range of motion can be influenced by pre-operative range of motion, which can be a challenge in cases of stiff knee [1]. This condition can pose technical difficulties for surgeons, such as requiring extensive approaches to achieve proper exposure, risk of patellar tendon avulsion, difficulty with soft-tissue balancing, and component malposition [2]. Stiff knees also carry a higher risk of complications and revision rates. Nonetheless, some studies have suggested that post-operative range of motion in patients with stiff knee can be comparable to that of flexible knees following total knee arthroplasty (TKA) [3]. While conventional jig-based TKA with measured resection technique requires bone resections followed by soft-tissue releases to balance the knee, robotic-assisted TKA has emerged as a promising alternative to improve the accuracy of component positioning, achieve targeted alignments, and improve knee balancing [4]. This case report describes the use of a novel mid-resection workflow technique with robotic assistance to manage TKA in a patient with stiff knee.
We present the case of a 58-year-old female patient with complaints of bilateral knee pain for 4 years. The pain severity increased on the left side, accompanied by the onset of stiffness and deformity that progressively worsened over time. At present, the patient experiences severe limitations in the range of motion and has been reliant on a wheelchair for the past year. There is no history of inflammatory arthritis. During the clinical examination, the patient exhibited a fixed flexion deformity of 40° in the left knee with an additional free flexion up to 60°. Radiograph revealed end-stage arthritis on the left side in the anteroposterior view (Fig. 1). However, it should be noted that the anteroposterior view did not provide an accurate representation of the sagittal plane deformity, which was approximately 40°. Pre-operative investigations for inflammatory arthritis yielded negative results.
Pre-operative workup
The patient presented with poor knee scores, including an Oxford Knee score of 11, a Knee Society score of seven, and a Kujala score of 38. After evaluation, we determined that a total knee replacement using the Stryker Triathlon system, with the assistance of Mako Robotic Technology, was the most appropriate course of action. As part of the robotic planning process, a pre-operative computerized tomography scan was done to facilitate precise surgical planning (Fig. 2).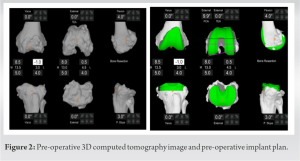
Surgical procedure
The surgical procedure was carried out with the patient under combined spinal and epidural anesthesia, with the application of a tourniquet. A medial parapatellar approach was utilized to access the left knee joint. Extensive intra-articular and patellofemoral adhesions were observed (Fig. 3). These adhesions were carefully and gradually released, resulting in the restoration of flexion up to 90°. After performing all possible releases, it was observed that the static limb deformity of the patient was 7° of varus and 32° of flexion deformity (Fig. 4). As per the Mako Robotic design, capturing medial and lateral gaps in extension is only feasible if the limb flexion is < 20°, which was not the case for our patient. Hence, we decided to implement the mid-resection workflow.
As per the Mako Robotic design, capturing medial and lateral gaps in extension is only feasible if the limb flexion is < 20°, which was not the case for our patient. Hence, we decided to implement the mid-resection workflow.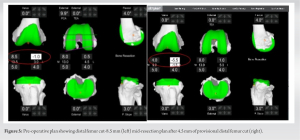 Although the pre-operative distal femur cut was planned to be eight millimeters (mm), we performed a preliminary distal femur cut of 4.5 mm (Fig. 5) to reduce the flexion deformity of the knee, which allowed us to capture the extension gaps (Fig. 6).
Although the pre-operative distal femur cut was planned to be eight millimeters (mm), we performed a preliminary distal femur cut of 4.5 mm (Fig. 5) to reduce the flexion deformity of the knee, which allowed us to capture the extension gaps (Fig. 6).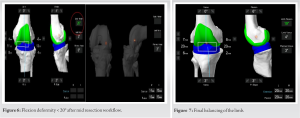 Following the assessment of gaps, we proceeded with knee balancing in both flexion and extension and set the tibial component in 3° of varus and 3° of posterior slope in functional alignment. The femur was positioned at 5° of external rotation with respect to the transepicondylar axis and 8° of flexion. To correct the varus, we performed a deep medial collateral ligament release and posteromedial release. After balancing, we noted a residual limb flexion deformity of 13°, which we corrected by performing a posterior capsular release (Fig. 7 and 8). The knee trial components were found to be stable in both flexion and extension. We used Stryker Triathlon system which included a femur component of size 3, a tibial component of size 3, a stem extension in tibia of size 12 mm × 50 mm, and a liner of size 11 mm. To reconstruct the defect in the posterolateral tibial condyle, we used a 3.5 mm × 30 mm cortical screw (Fig. 9). Before cementing the final prosthesis, pulse lavage was administered, and the components were found to be stable in both flexion and extension. We performed a non-resurfacing patelloplasty, and patellar tracking was optimal. The wound was then closed in layers.
Following the assessment of gaps, we proceeded with knee balancing in both flexion and extension and set the tibial component in 3° of varus and 3° of posterior slope in functional alignment. The femur was positioned at 5° of external rotation with respect to the transepicondylar axis and 8° of flexion. To correct the varus, we performed a deep medial collateral ligament release and posteromedial release. After balancing, we noted a residual limb flexion deformity of 13°, which we corrected by performing a posterior capsular release (Fig. 7 and 8). The knee trial components were found to be stable in both flexion and extension. We used Stryker Triathlon system which included a femur component of size 3, a tibial component of size 3, a stem extension in tibia of size 12 mm × 50 mm, and a liner of size 11 mm. To reconstruct the defect in the posterolateral tibial condyle, we used a 3.5 mm × 30 mm cortical screw (Fig. 9). Before cementing the final prosthesis, pulse lavage was administered, and the components were found to be stable in both flexion and extension. We performed a non-resurfacing patelloplasty, and patellar tracking was optimal. The wound was then closed in layers.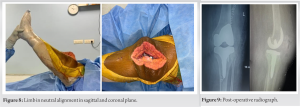
Post-operative protocol
The patient received antibiotics and deep vein thrombosis prophylaxis post-operatively. Physiotherapy was initiated on the 1st day after the surgery, and the patient was permitted to bear full weight with the aid of a hinged knee brace. Range of motion exercises was encouraged as much as possible, along with quadriceps strengthening and stretching exercises. At the end of 6 weeks, the patient achieved a knee flexion of 100°. After 1-year follow-up, patient achieved 110° flexion and good functional outcome.
To walk normally, the knee needs to be flexed at least 60°–70°, while climbing stairs require 90 be flexed at least 60 ear full weight with°. Stiff knee can make walking difficult, cause limping, and severely impact daily life, leading to psychological distress. TKA may be considered by patients seeking to reduce pain and increase knee range of motion, thereby improving their quality of life [5]. Stiff knee can have various causes, including prior knee surgery, advanced primary knee osteoarthritis, post-traumatic osteoarthritis, reflex sympathetic dystrophy, neuromuscular disorders, sequelae of previous infection, inflammatory diseases (such as rheumatoid and psoriatic arthritis), arthrofibrosis, and hemophilic arthropathy. Individuals who have experienced knee immobilization or rely on wheelchairs are at a higher risk of developing ankylosis [6]. Patients with stiff knee commonly exhibit clinical features such as patella baja, quadriceps contracture, intra-articular adhesions, posterior capsule contracture, poor patellar gliding, and heterotopic ossification [3]. Performing TKA in patients with stiff knee is a challenging procedure, with the primary aim being to improve knee mobility and ambulatory ability during gait. Other goals include pain relief, correction of knee deformity, and knee stability. TKA is a viable option for enhancing functional capacity and achieving a mobile knee. RATKA is a promising surgical technique for treating knee osteoarthritis due to several advantages. One such advantage is the ability to pre-balance the knee before bone cuts are made. This pre-balancing involves the use of the robotic arm to evaluate the tension and stability of the soft tissues surrounding the knee joint, allowing the surgeon to determine the optimal position and alignment of the implants. As a result, the surgeon can make the most conservative bone cuts and perform soft-tissue releases optimally. According to Lustig et al., soft-tissue releases may not be necessary if kinematic or functional alignment is achieved during TKA. There are two primary surgical workflows utilized in RATKA for pre-balancing the knee: the pre-resection workflow and the mid-resection workflow. The pre-resection workflow is typically used in cases where the deformity is correctable, and adjustments in the implant position can achieve both balance and targeted alignment. In this approach, the knee gap is balanced first, and then, the bone cuts are made sequentially without requiring major soft-tissue releases. Based on our experience, while the pre-resection workflow has been helpful in achieving pre-balance in many cases, there have been instances where additional soft-tissue releases were necessary [7-9]. The mid-resection workflow is used when pre-balance cannot be achieved by adjusting the implant position alone. In such cases, the extension gap is balanced initially, followed by balancing the flexion gap. This approach is typically reserved for cases where there are more complex deformities or when the soft tissue is too tight to allow for pre-resection balancing. In such cases, the initial two cuts made during the pre-resection workflow provided access to the tibial side, which allowed for the required soft-tissue releases to be performed. This highlights the importance of a tailored approach to each patient’s unique anatomy and condition, and the need for flexibility in adapting surgical workflows to meet individual patient needs [10]. To our knowledge, there is currently no existing literature that supports the efficacy of using distinct robotic-arm-assisted TKA workflows in the management of patients with challenging cases of stiff knee.
Severe knee arthritis with flexion deformities is a prevalent condition in surgical practice. The use of RATKA has enabled us to evaluate and establish the efficacy of different pre-balance workflows in managing these cases. By utilizing the mid-resection flow technique in RATKR, we can optimize soft-tissue balance, implant positioning, and alignment, thereby enhancing our ability to provide better outcomes and improve the quality of life for patients with severe deformities.
This article highlights the significance of a novel mid-resection workflow that is designed specifically for RATKA in cases of osteoarthritis with a stiff knee.
References
- 1.De Carvalho RT. Primary total arthroplasty in stiff knees. In: Arthroplasty, Advanced Techniques and Future Perspectives. United Kingdom: IntechOpen; 2023. [Google Scholar | PubMed]
- 2.Debette C, Lustig S, Servien E, Lording T, Villa V, Demey G, et al. Total knee arthroplasty of the stiff knee: Three hundred and four cases. Int Orthop 2014;38:285-9. [Google Scholar | PubMed]
- 3.Rodríguez-Merchán EC. The stiff total knee arthroplasty: Causes, treatment modalities and results. EFORT Open Rev 2019;4:602-10. [Google Scholar | PubMed]
- 4.St Mart JP, Goh EL. The current state of robotics in total knee arthroplasty. EFORT Open Rev 2021;6:270-9. [Google Scholar | PubMed]
- 5.Nam CH, Lee SC, Kim JH, Ahn HS, Baek JH. Robot-assisted total knee arthroplasty improves mechanical alignment and accuracy of component positioning compared to the conventional technique. J Exp Orthop 2022;9:108. [Google Scholar | PubMed]
- 6.Vaish A, Vaishya R, Bhasin VB. Etiopathology and management of stiff knees: A current concept review. Indian J Orthop 2020;55:276-84. [Google Scholar | PubMed]
- 7.Masilamani S, Mulpur P, Annapareddy A, Hippalgaonkar K, Roche MW, Reddy AV. Enhanced mid-resection workflow technique for severe varus deformity correction using robotic-arm assisted total knee arthroplasty. Surg Technol Int 2022;41:sti41/1612. [Google Scholar | PubMed]
- 8.Grau L, Lingamfelter M, Ponzio D, Post Z, Ong A, Le D, et al. Robotic arm assisted total knee arthroplasty workflow optimization, operative times and learning curve. Arthroplast Today 2019;5:465-70. [Google Scholar | PubMed]
- 9.Lustig S, Sappey-Marinier E, Fary C, Servien E, Parratte S, Batailler C. Personalized alignment in total knee arthroplasty: Current concepts. SICOT J 2021;7:19. [Google Scholar | PubMed]
- 10.Cievet-Bonfils M, Batailler C, Lording T, Servien E, Lustig S. Performing patient-specific knee replacement with intra-operative planning and assistive device (CAS, robotics). In: Rivière C, Vendittoli PA, editors. Personalized Hip and Knee Joint Replacement. Cham: Springer; 2020. [Google Scholar | PubMed]