The distal radius fracture management methods followed during COVID pandemic can be applied to regular practice.
Dr. Chandrashekara Maliyappa, Department of Trauma and Orthopaedics, Southend University Hospital, Westcliff on Sea, Essex, United Kingdom. E-mail: drshekar76@rediffmail.com
Background: COVID-19 pandemic created extreme pressure situation on health care services across the globe with shortage of medical staff and beds. The management of fragility fracture also affected significantly. The distal radius fractures (DRFs) are one of the common frailty fractures. There was a significant shift in the treatment of such injuries with new guidelines leaning toward more of non-operative management.
Case Report: A retrospective cross-sectional study of DRFs (DRF) treated during COVID pandemic for a period of 1 year in the United Kingdom. This included all radiologically confirmed cases of DRFs with isolated adult injuries excluding polytrauma, same limb other injuries, associated neurovascular injuries, and age below 18 years. All patient’s data were collected from hospital records retrospectively from April 2020 to March 2021. There was(were) a total of 179 patients with distal radius fracture, of which 141 (78.8%) were females and 38 (21.2%) males. The mean age was 68.2 years (SD 68.20 ± 15.63) and there were greater number of patients with intra-articular fracture. There were 28.5% (Grades 1 and 2, Group I) extra-articular fractures; 69.8% (Grades 3–8, Group II) were intra-articular fractures and 3 Barton’s fractures (Group III) accounted to 1.7%. 137 patients were (76.5%) treated to non-operatively and 42 (23.5%) were treated surgically. 135 (75.4%) patients had good and 43 (24%) satisfactory clinical outcomes. 3 (1.6%) patients required osteotomy for malunited fractures. Fracture grade I and II is significantly associated with non-operative procedure (100.0% vs 84.3%) with P < 0.001.
Conclusions: This study confirmed that non-operative treatment is still a good option even in intra-articular fractures. Surgical fixation should be considered in young patients and those with higher grade of fracture classification and greater angulation at presentation. A virtual physiotherapy is still a good option.
Keywords: Wrist fractures, COVID-19, retrospective study, adult.
During COVID-19 pandemic, there was extreme pressure on health-care services across the globe, resulting in re-deployment of hospital staff to support ICU and respiratory teams. There was acute shortage of hospital beds for COVID patients, resulting in redefining the indications for the surgeries. During this period, there was significant shift in management of distal radius fractures (DRFs). During COVID pandemic, British Orthopaedic Association (BOA) came up with new guidelines for the management of wrist fractures. Most upper limb fractures, including clavicle, humeral and wrist fractures have high rates of union and may be managed non-operatively, recognizing that some patients may require late reconstruction. They have advised a pragmatic approach to fracture management during the COVID-19 pandemic [1]. Knirk and Jupiter, in their study, concluded that distal radius intra-articular fractures with >2 mm displacement led to radiological signs of post-traumatic arthritis [2]. UK DRAFFT study showed no difference in functional outcomes between the patients with distal radius fracture treated either with K-wire or Volar locking plates [3]. The BOA and the NHS England also released guidelines that encouraged surgeons to “balance optimum treatment of a patient’s injury or condition against clinical safety and resources” [4,5]. During COVID, the surgical indications were narrowed further due to COVID risk, vulnerable population were advised for shielding and protecting by the UK government. Considering the restrictions on the availability of resources during COVID-19 pandemic, some of the fractures which are normally managed by surgery were treated conservatively [6]. Covid pandemic changed the way the patients were treated and followed up. During COVID, large number of these patients was followed up virtually [6]. During COVID pandemic, many hospitals adopted a new self-care pathway for minimally displaced distal radius fractures. Patient is discharged from a virtual fracture clinic without a physical review and is provided with written instructions on how to remove their own cast or splint at home, plus advice on exercises, and return to function [7]. Similarly, DRFs patients also had different ways of post-immobilization rehabilitation which included an advice leaflet; an advice video; or face-to-face therapy session(s) [8]. This study was done to assess the outcome analysis of all the adult DRFs treated during COVID pandemic with significant shift away from standard practice.
This is a retrospective cross-sectional study done after local ethical committee approval, included all adult patients seen either in A and E or in Orthopaedic clinics with radiologically confirmed DRF between April 2020 and March 2021, 1-year period of pandemic. These patients were identified by X-rays on PACS (Picture Archiving communications systems) and other details were collected from A and E attendances, Orthopaedic clinic records, surgical data, discharge letters, and physiotherapy outcomes. This study included adults aged 18 years and above, with radiologically confirmed DRFs, isolated closed fractures. Those patients with open fractures, aged less than 18, associated with same limb other injuries, polytrauma, neurovascular injuries, and those patients dead were excluded from the study. The DRFs were classified as per Frykman’s classification on X-rays taken at presentation [9]. In addition, the amount of radial shortening and angulation were also assessed. Displaced fractures were manipulated either in A and E or in plaster room under the hematoma block, Entonox, or Penthrox (alone or in combinations) and placed in below elbow back slab. If post-manipulation X-rays were satisfactory, the patient was brought back to fracture clinic within a week for check X-ray and completion of plaster. In stable fractures, plasters were continued for 4–6 weeks, and plaster was taken off either by patients themselves or in plaster room to reduce the risk of COVID infection. Unstable fracture at presentation, those with unacceptable reduction on post-manipulation X-rays and patients with low COVID risk underwent surgery during the next available theater space. Surgical indications were tailored to each patient depending on their comorbidities, patient expectations, and COVID risk. Those patients with significant comorbidities, on immunosuppressants, needs shielding were continued to be treated non-operatively irrespective of fracture stability. All the patients were followed up either virtually or in person until discharge from clinic or to physiotherapy. Those patients at the final follow-up who had good range of movements with no symptoms and good function were grouped with good outcome. While those with minimal symptoms and restrictions of movements were considered as satisfactory outcome, those patients with persistent symptoms and functional limitations were considered poor outcome. There were a total of 179 patients with DRFs, 141 (78.8%) female and 38 (21.2%) males. There were 106 (59.2%) left and 73 (40.8%) right DRFs. There were 129 (72.1%) patients aged 61 and above, while 50 (27.9%) were below 60 years of age. The mean age was 68.2 years (SD 68.20 ± 15.63).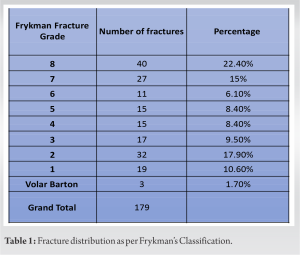
Fractures distribution as per Frykman’s classification is shown in . Group I with extra-articular fractures were 51 (28.5%, grade 1 and 2), while group-II intra-articular fractures were 125 (69.8%, grade 3–8) and group III with Barton’s fractures (3, 1.7%). The procedures were done by A and E doctor in 91 patients and 88 by Orthopaedic doctors. The fracture distribution in different age groups is shown in Table 2.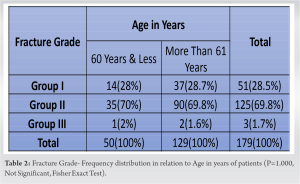
The list of primary procedures done is listed in Table 3. 79 (44%) patients did not require any intervention, while 81 (45%) needed manipulation. Surgical fixation was done in 20 patients (11.2%) as a primary procedure and 22 (12.3%) as secondary procedure in follow-up period. Out of total patients, 16.8% needed secondary procedures during follow-up period. Rest of the details are in Table 4.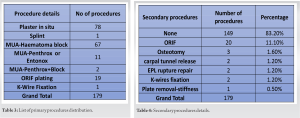
Physiotherapy was carried out virtually in 91 (50.8%) patients, in person in 35 (19.6%) and rest of the patients did not have physiotherapy. Average clinical follow-up was 82.6 days (range: 6–613 days) and median of 55 days.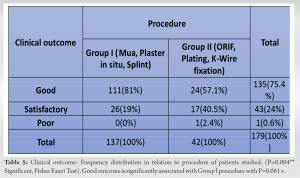
The clinical outcome in non-operative and operative groups is shown in Table 5. There is statistical significance difference in clinical outcome, and non-operative group had better outcome compared to surgical group with P = 0.004. Table 6 shows fracture distribution in relation to treatment type. The number of patients who underwent non-operative management was higher compared to the surgical group, which was statistically significant (P = 0.011*).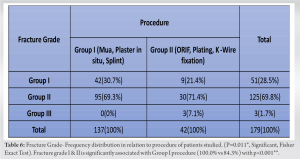
All the statistical calculations were done using SPSS 22.0, and R environment version 3.2.2 was used for the analysis of the data and Microsoft Word and Excel have been used to generate graphs, tables, etc.
This study was aimed to find the both radiological and functional outcomes of DRFs treated during COVID-19 pandemic. Before the pandemic, BOA Standards for Trauma and Orthopaedics guidelines for DRF management advocated manipulation of fracture under regional anesthesia and 72-h follow-up in fracture clinic post-manipulation [10]. In our study, fractures were manipulated with other methods, to minimize COVID exposure risk both to patients and hospital staff. Patients were followed up at around a week from manipulation, instead of 72 hours. A similar care plan was used in many centers in the UK during COVID [6,11]. The surgical fixation was considered in younger patients with unstable fracture and those with low risk of COVID infection. Keskin and Karslioglu’s study considered articular or periarticular fractures as “obligatory fractures to surgical treatment” during COVID pandemic [12]. In our study, we had more female patients and similar trends were noticed in other studies [6,13,14]. We have used Frykman’s classification as this is simple to use and has moderate reproducibility [15]. Many other studies have used classification, but when this classification used with subdivisions, its reliability and reproducibility are reduced significantly [6,15]. In our study, a total of 23.4% patients required surgical fixation, which is less compared to other studies [6,12,16]. The average follow-up was 82.6 days, which is less than other studies done during pandemic [6], this is because our patients had satisfactory to good outcome at discharge. In this study, out of 137 non-operatively treated patients, 3 required corrective osteotomy for malunited fractures in our study. Harvey et al.’s study had one malunion, treated non-operatively [11]. Five patients in our study required surgery for other complications and no patients had non-union. While other studies were done during COVID, there was no mention of malunion and other complications [12,14]. About 75.4% of our patients had good results and while 24% had satisfactory functional results at discharge. Only 1 patient had poor outcome who had malunion requiring corrective osteotomy. The patients who underwent non-operative management had higher percentage of satisfactory to good results. Although more than half of our patients had virtual physiotherapy, did not have negative impact on outcome. This case series covered the peak pandemic period of a year with three lockdown periods with all patients followed up.
This case series confirmed that non-operative treatment is still a good option even in intra-articular fractures. Surgical fixation should be considered in young patients, those with higher fracture grades, and greater angulation at presentation.
The distal radius fracture management methods followed during COVID pandemic can be applied to regular practice.
References
- 1.British Orthopaedic Association. 2021 BOAST-management of Patients with Urgent Orthopaedic Conditions and Trauma During the Coronavirus Pandemic. Available from: https://www.boa.ac.uk/uploads/assets [Last accessed on 2021 Sep 26]. [Google Scholar | PubMed]
- 2.Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am 1986; 68:647-59. [Google Scholar | PubMed]
- 3.Costa ML, Achten J, Plant C, Parsons NR, Rangan A, Tubeuf S, et al. UK DRAFFT: A randomised controlled trial of percutaneous fixation with Kirschner wires versus volar locking-plate fixation in the treatment of adult patients with a dorsally displaced fracture of the distal radius. Health Technol Assess 2015;19:1-124, v-vi. [Google Scholar | PubMed]
- 4.BOAST-management of Patients with Urgent Orthopaedic Conditions and Trauma During the Coronavirus Pandemic; 2020. Available from: https://www.boa.ac.uk/uploads/assets/782e0b20-f9ce-4fc919f943740161405/201ebd61-5828-4c81-b45a8b80ac47fd50/covid-19 [Google Scholar | PubMed]
- 5.NHS England and NHS Improvement. Specialty Guides. Coronavirus. United Kingdom: NHS England; 2020. [Google Scholar | PubMed]
- 6.Okereke IC, Ramadan O, Sampalli SR. The management of wrist fractures during COVID-19: A preliminary report. Cureus 2021;13:e19982. [Google Scholar | PubMed]
- 7.Hutchison AM, Bodger O, Whelan R, Russell ID, Man W, Williams P, et al. Functional outcome and patient satisfaction with a ‘self-care’ protocol for minimally displaced distal radius fractures: A service evaluation. Bone Jt Open 2022;3:726-32 [Google Scholar | PubMed]
- 8.Coughlin T, Norrish AR, Scammell BE, Matthews PA, Nightingale J, Ollivere BJ. Comparison of rehabilitation interventions in nonoperatively treated distal radius fractures: A randomized controlled trial of effectiveness. Bone Joint J 2021;103-B:10339. [Google Scholar | PubMed]
- 9.Frykman G. Fracture of the distal radius including sequelae-shoulder-hand-finger syndrome, disturbance in the distal radio-ulnar joint and impairment of nerve function. A clinical and experimental study. Acta Orthop Scand 1967;38:1-61. [Google Scholar | PubMed]
- 10.British Orthopaedics Association. Best Practice for Management of Distal Radius Fractures. BOA, BSSH. Bluebook DRF; 2018. Available from: https://www.bssh.ac.uk/_userfiles/pages/files/professionals/radius/blue%20book%20drf%20final%20document [Google Scholar | PubMed]
- 11.Harvey J, Varghese BJ, Hahn DM. Displaced distal radius fracture: Reduction, follow-up, and clinical outcomes: Learning from a pragmatic approach during the 2020 COVID-19 lockdown transition. Bone Jt Open 2021;2:338-43. [Google Scholar | PubMed]
- 12.Keskin AE, Karslioglu B. Did Covid-19 pandemic narrow the spectrum of surgical indications? J Clin Invest Surg 2021;6:58-63. [Google Scholar | PubMed]
- 13.Tse CY, Lee LH, Akbari AR, Niazi NS, Pillai A. The impact of COVID-19 restrictions and changes in guidelines on adult wrist fracture management. J Wrist Surg 2021;11:322-9. [Google Scholar | PubMed]
- 14.Akti S, Çankaya D. The effect of the COVID-19 pandemic on the epidemiology of distal radius fractures. Cumhuriyet Med J 2021;43:79-84. [Google Scholar | PubMed]
- 15.Shehovych A, Salar O, Meyer C, Ford DJ. Adult distal radius fractures classification systems: Essential clinical knowledge or abstract memory testing? Ann R Coll Surg Engl 2016;98:525-31. [Google Scholar | PubMed]
- 16.Olech J, Ciszewski M, Morasiewicz P. Epidemiology of distal radius fractures in children and adults during the COVID-19 pandemic-a two-center study. BMC Musculoskelet Disord 2021;22:306. [Google Scholar | PubMed]











