FAVA is a rare, but specific vascular anomaly that is often misdiagnosed with other intramuscular vascular malformations and therefore poses significant management challenges. It is imperative that clinicians have a thorough understanding of FAVA in order to provide proper diagnosis and treatment referrals
Dr. Manit K Gundavda, Department of Orthopaedic Oncology, Kokilaben Dhirubhai Ambani Hospital and Medical Research Institute, Mumbai, India. E-mail: manit.gundavda@gmail.com
Introduction: Fibroadipose vascular anomaly (FAVA) was described in 2014 as a distinct entity characterized by intramuscular replacement with fibro fatty tissue along with complex vascular malformation, phlebectesia, venous thrombosis and lymphatic involvement. Somatic mutations in the PIK3CA gene are detected in most lesions which diagnosed the FAVA in our report and occurrence of this mutation seems to be sporadic.
Case Report: Common presentation is a painful intramuscular swelling in young women – as was the presentation here in an 11 year girl with the swelling of the right thigh. Imaging features, phleboliths and long standing history of an intramuscular malformation in the young girl that was recalcitrant to treatment at previous attempts led us towards the suspicion of a fibro adipose vascular anomaly.
Conclusion: Surgery with en-bloc mass excision is recommended for good long term curative option for reducing pain and regaining movements. FAVA is a rare, but specific vascular anomaly that is often misdiagnosed with other intramuscular vascular malformations and therefore poses significant management challenges. It is imperative that clinicians have a thorough understanding of FAVA in order to provide proper diagnosis and treatment referrals.
Keywords: FAVA, vascular malformation, intramuscular, soft tissue tumor, genetic mutation
The recent description of a distinct entity in fibroadipose vascular anomaly (FAVA) by the International Society for the Study of Vascular Anomalies (ISSVA) in 2014 [1] and revised classification in 2018 [2,3] brings to light the complex vascular anomalous malformation occurring within the muscles of young women (female-to-male predisposition described as 3:1) [4]. The sporadically occurring somatic mutations in the PIK3CA gene have been associated with most of these lesions [5]. We aim to describe the clinical, radiological as well as pathology features of our patient, our methodology toward the diagnosis and treatment for FAVA, and how it all differed from its close and common differential in a slow flow vascular malformation.
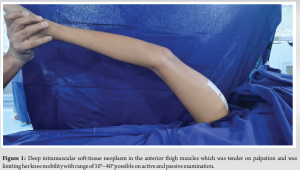
We present an 11-year-old girl with a painful anterior right thigh swelling for 4 years. It began as a painful small lump deep in her anterior mid-thigh region and gradually progressed to a large swelling that caused her severe local pain and limitation of movements at the knee. Her mother noticed a limp with pelvis and shoulders dropping to the affected side while walking and this has progressed over the past year. She had undergone an incisional biopsy which was inconclusive and treated with intra-lesional chemical/sclerosant injection before presentation to our institution. Our clinical evaluation brought to light a deep intramuscular soft-tissue neoplasm in the anterior thigh muscles which was tender on palpation and was limiting her knee mobility with range 10°–40° possible on active and passive examination (Fig. 1). Hypotrophy of calf muscles recorded on girth circumference and limb length discrepancy from >2 cm of limb shortening on the affected side was recorded (Fig. 2).

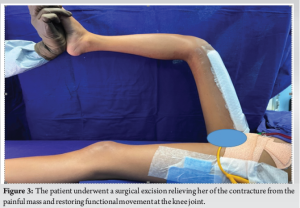
High-resolution ultrasound showed evidence of an ill-defined hyperechoic area within the muscles in the anterior compartment of thigh with few tubular vascular channels within on-power Doppler ultrasound, mostly representing a vascular malformation. A multiplanar multiecho plain and contrast magnetic resonance (MR) imaging of the right has been performed. In addition, MR angiogram of the right has been performed with arterial, venous, and delayed phases of scanning that reported a large heterogeneous intramuscular lesion in the anterior compartment of the right thigh predominantly involving the vastus muscles and sparing the rectus femoris with superoinferior length of approximately 24 cm. Regions of fat infiltration in relation to the muscles may represent the presence of fat component or fat atrophy of the vastus muscles. Additional plain computed tomography scan was also obtained that showed multiple poorly defined T2 hyperintense lobulated compartments with septations and multiple interspersed calcific foci which may represent phleboliths. On MR angiography, few dilated arterial branches from the deep femoral artery supplied the lesion with few areas of early enhancement without evidence of an early draining vein, definite venous shunting, or discrete nidus. Imaging features, phleboliths, and long-standing history of an intramuscular malformation in the young girl that was recalcitrant to treatment at previous attempts led us toward the suspicion of a FAVA rather than a vascular malformation or soft-tissue neoplasm and therefore a biopsy was recommended to confirmation. Pathology confirmed an intramuscular lesion with medium-sized arteries, veins, and lymphatics with intervening fibroadipose and muscle tissue. No evidence of atypia, necrosis, or malignancy was seen. Next-generation sequencing (NGS) was used for sequencing and variant/mutation detection, and a clinically relevant mutation was identified in the PIK3CA gene of the specimen clinching the diagnosis of FAVA. Keeping with the recommendations for management of FAVA as reported literature, the patient underwent a surgical excision relieving her of the contracture from the painful mass and restoring functional movement at the knee joint (Fig. 3).
The patient will continue to remain under surveillance for recurrence of the lesion while she continues to rehabilitate for lower limb muscle and range of movement physical therapy. While we were unable to explain the limb shortening, we hypothesize that the paradoxical vasodilatory response associated with the vascular anomaly reduced the blood flow to the impaired perfusion area as seen with steal phenomena resulting in stunted affected limb growth.
Initial working diagnosis before consultation at our institute was an arteriovenous malformation, considering it is the more common neoplasm [2]. However, we recognized the need for re-evaluation of the diagnosis in the presence of recalcitrant pain from an intramuscular neoplasm in the young girl, causing functional as well as growth limitations and failure to previous therapy [6]. The diffuse mass appearance on imaging not amenable to endovascular embolization due to lack of nidus or specific feeding or draining vessels led to the evaluation for a distinct clinical entity in FAVA which was described in 2014 [1] and later revised in the ISSVA classification in 2018 [2,7]. Pathology is essential to confirm the diagnosis [8] and availability of NGS to identify a clinically relevant PIK3CA gene anomaly may be used to differentiate FAVA from close differentials of soft-tissue hamartomas or vascular malformation syndromes as was demonstrated in this case [5]. Treatment options for FAVA differ from that of vascular malformations in the fact that surgical excision is the recommendation in literature as the curative option, especially in patients presenting with contractures and large mass lesions limiting the functional range of movement [4,9]. Near total excisions may be performed to limit the difficulty or disability resulting from large muscular resections due to the intramuscular tumor location [8]. Sirolimus has recently been used for treatment as an alternative to surgery in lesions in children under expert supervision [4]. Minimally invasive ablative procedures (radiofrequency/cryoablation) with or without embolization/sclerotherapy have been used with variable success aimed at pain relief rather than treatment of the lesion [7].
FAVA is a distinct and recently described entity posing a significant diagnostic and management challenge requiring a multidisciplinary team approach. While intramuscular lesions may lead to loss of muscle bulk with surgery, correction of deformities and resection of painful lesions improves function.
FAVA is characterized by intramuscular replacement with fibro-fatty tissue, complex vascular malformation, phelbectesia, venous thrombosis, and lymphatic involvement. Considering the fact that FAVA is yet to be classified in the pathology classification of soft tissue neoplasms as a distinct entity, the diagnosis involves genetic mutation analysis for FAVA in a suspected combination of clinical, radiographic, and pathological neoplasm. Furthermore, the treatment of FAVA differs from its close differential in an intramuscular arteriovenous malformation.
References
- 1.Alomari AI, Spencer SA, Arnold RW, Chaudry G, Kasser JR, Burrows PE, et al. Fibro-adipose vascular anomaly: Clinical-radiologic-pathologic features of a newly delineated disorder of the extremity. J Pediatr Orthop 2014;34:109-17. [Google Scholar | PubMed]
- 2.Amarneh M, Shaikh R. Clinical and imaging features in Fibro-adipose Vascular Anomaly (FAVA). Pediatr Radiol 2020;50:380-7. [Google Scholar | PubMed]
- 3.Merrow AC, Gupta A, Patel MN, Adams DM. 2014 revised classification of vascular lesions from the international society for the study of vascular anomalies: Radiologic-pathologic update. Radiographics 2016;36:1494-516. [Google Scholar | PubMed]
- 4.Lipede C, Nikkhah D, Ashton R, Murphy G, Barnacle AM, Patel PA, et al. Management of Fibro-adipose Vascular Anomalies (FAVA) in paediatric practice. JPRAS Open 2021;29:71-81. [Google Scholar | PubMed]
- 5.Rodriguez-Laguna L, Agra N, Ibanez K, Oliva-Molina G, Gordo G, Khurana N, et al. Somatic activating mutations in PIK3CA cause generalized lymphatic anomaly. J Exp Med 2019;216:407-18. [Google Scholar | PubMed]
- 6.Hori Y, Hirose K, Aramaki-Hattori N, Suzuki S, Nakayama R, Inoue M, et al. Fibro-adipose Vascular Anomaly (FAVA): Three case reports with an emphasis on the mammalian target of rapamycin (mTOR) pathway. Diagn Pathol 2020;15:98. [Google Scholar | PubMed]
- 7.Shaikh R, Alomari AI, Kerr CL, Miller P, Spencer SA. Cryoablation in Fibro-adipose Vascular Anomaly (FAVA): A minimally invasive treatment option. Pediatr Radiol 2016;46:1179-86. [Google Scholar | PubMed]
- 8.Driskill JH, Hwang H, Callan AK, Oliver D. Case report of Fibro-adipose Vascular Anomaly (FAVA) with activating somatic PIK3CA mutation. Case Rep Genet 2022;2022:9016497. [Google Scholar | PubMed]
- 9.Parmar B, Joseph JS, Kavin Ilangovan G, Khalil-Khan A, Anand R, Parthasarathy EA, et al. Fibro-adipose vascular anomaly: A case report and literature review. Cureus 2022;14:e30757. [Google Scholar | PubMed]
- 10.Gundavda MK, Sanghvi D, Athikari N, Sekhar R. A painful mass infiltrating the quadriceps compartment of a young female. Skeletal Radiol 2024;53(11):2503-5. [Google Scholar | PubMed]






